Dental Implant Materials
- Implanting a foreign material directly into the bone in order to replace missing teeth has been a goal sought since ancient times.
- Though many materials have been tried, currently, the vast majority of implant systems use titanium in some form.
Dental Implant Materials Definition
A dental implant is a material or device placed in and/or on oral tissues to support an oral prosthesis (GPT-8).
History And Development Of Dental Implants
- Man has been searching for ways to replace missing teeth for thousands of years.
- Ancient Egyptians used tooth-shaped shells and ivory to replace teeth.
- The Etruscans living in what is now modern Italy replaced missing teeth with artificial teeth carved from the bones of oxen.
- Further evidence of tooth replacement was found in 1931 by an archeological team excavating in Honduras.
- A mandible of Mayan origin was discovered that had tooth-shaped pieces of shells placed in the sockets of three missing lower incisor teeth.
- Modern implant dentistry began in the early 19th century. A lot of experiments were conducted on what material would work best.
- Attempts were first made at implanting natural teeth from another person’s mouth, but these implants failed due to infection or were rejected by the host tissue.

- Implants made of gold, porcelain, silver, and even lead were being tried, with only a fair measure of success and little or no predictability.
- As early as 1918, Greenfield devised the Iridoplatinum root form basket implant.
- Other early implants were those of Chercheve, Formiggini, and others.
- An interesting design was the Tripodal pin implant of Scialom.
- Interestingly some of these early designs were ahead of their times.
- Their failure to gain widespread popularity could probably be attributed to the fact that prosthetic techniques, antibiotic use, infection control, instrumentation, and impression materials had not yet advanced far enough.
- One of the early pioneers in this field Dr. AE Strock in 1931, suggested using Vitallium, a metal alloy for dental implants.
- In 1947, Manlio Formiggini of Italy developed an implant made of tantalum.
- At the same time, Raphael Chercheve was using implants made of a chrome-cobalt alloy.
- By 1964, commercially pure titanium was accepted as the material of choice for dental implants.
- Ever since almost all dental implants are made of titanium.
- The body does not recognize titanium as a foreign material, resulting in less host rejection of the implant.
- Other areas of medicine recognize this fact and use titanium for other implants such as joint replacements and heart valves.
- In the 1950s an important discovery was made which had great implications for tooth replacement therapy.
- During an experiment involving the study of blood circulation in animals.
- Dr. Per-Ingvar Branemark discovered that the hollow titanium rod used in the study was not retrievable.
- When the experiment was complete. Further studies showed that the animals’ bone had directly attached to the titanium surface.
Read And Learn More: Basic Dental Materials Notes
- This phenomenon was called osseointegration, defined by the American Academy of Implant Dentistry as “the firm, direct and lasting biological attachment of a metallic implant to the vital bone with no intervening connective tissue.”
- This firm anchor is what makes dental implants a wonderful option for replacing teeth.
- Experimentation with implant designs, not just those that were shaped like the tooth root, was also being done.
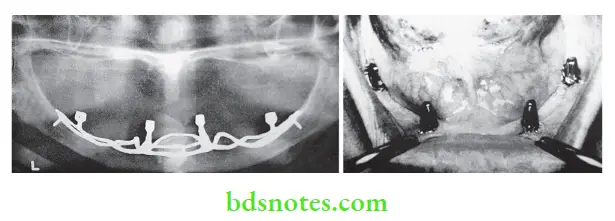
- In 1941, Dr. Gustav Dahl of Sweden provided a retentive mechanism for jaws that were completely edentulous.
- This was the introduction of the subperiosteal implant.
- Dr. Leonard Linkow of New York introduced the blade form implant in 1967.
- These blades came in a variety of sizes and forms and were the most widely used type of implant until the 1980s.
- Implants are no longer restricted to the mouth.
- They have been successfully used all over the body for various roles.
- Whether implants are here to stay is no longer a question, but research into perfecting materials, procedures, and training will continue in this exciting field of dentistry.
Types Of Dental Implants
- Subperiosteal—A framework that rests upon the bony ridge but does not penetrate it
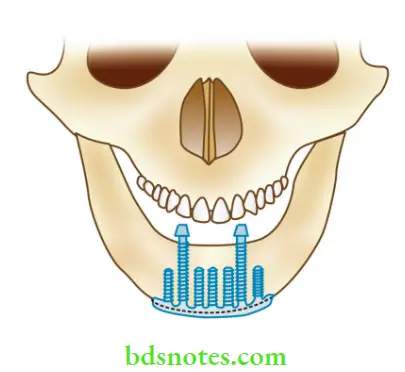
- Transosteal—Penetrates completely through the mandible.
- Endosseous—Partially submerged and anchored within the bone


Materials Used for Dental Implants
- Metals — Stainless steel
- Cobalt-chromium-molybdenum based
- Titanium and its alloys
- Surface coated titanium
- Ceramics — Hydroxyapatite
- Bioglass
- Aluminum oxide
- Polymers and composites
- Others — Gold, tantalum, carbon, etc.
Titanium
Commercially pure titanium (cp Ti) is currently the most widely used material for implants. It has become the material of choice because of its
- Low density (4.5 gm/cm 2) but high strength.
- Minimal biocorrosion due to its passivating effct.
- Excellent biocompatibility.
- The titanium also has good stiffness. Although its stiffness is only half that of steel, it is still 5 to 10 times higher than that of bone.
- Titanium alloys Alloyed forms of titanium are also used. Its alloyed form contains 6 wt.% aluminum and 4 wt.% vanadium.

Surface Coated Titanium
- The newer implant designs use titanium that is coated with a material that bonds and promotes bone growth (bioactive).
- The implant is coated with a thin layer of tricalcium phosphate or hydroxyapatite that has been plasma sprayed.
Ceramics
- These may be bioactive on bioinert. Their applications are still limited because of their low tensile strength and ductility.
- Currently, they are primarily used as surface coats on titanium implants.
Bioactive, for example,
- Hydroxyapatite
- Bioglass (CaO, NaO, P2O5 and SiO2)
- Bioinert, for example, aluminum oxide is used either in the polycrystalline form or as a single crystal (sapphire).
- It is well-tolerated by bone but does not promote bone formation.
- They are available in screw or blade form and are used as abutments in partially edentulous mouths.
Stainless Steel
18-8 or Austenitic steel had been tried as an implant material. It has high strength and ductility. Currently, these materials are rarely used.
Precautions
- Since it contains nickel, it should be avoided in nickel-sensitive patients.
- It is most susceptible to pit and crevice corrosion so the passivating layer must be preserved.
- Direct contact of the implant with a dissimilar metal crown is avoided to prevent galvanism.
Polymers And Composites
- Polymers have been fabricated in porous and solid forms for tissue attachment and replacement augmentation.
- However, in some implants, they are mainly used within the implants as connectors for stress distribution (shock absorption).
Other Materials
- In the past, gold, palladium, tantalum, platinum, and alloys of these metals have been used.
- More recently, zirconium and tungsten have been tried.
- Titanium has replaced most of these materials.
- Carbon compounds were used for root replacement in the 1970s.
- They are also marketed as coatings for metallic and ceramic devices.
Implant Parts
Basic Implant Design
Since endosseous cylindrical root-form implants are the most widely used design, subsequent discussions will focus on these. Implants can range from complex, having multiple components to more simple designs. Most endosseous implants can be divided into two basic parts.
- Fixture—embedded in bone
- Abutment—supports the crown
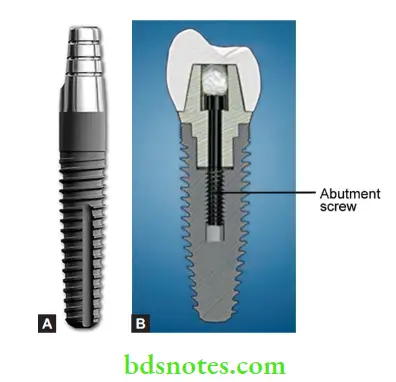
The implant may be
- One piece–Implant and abutment are joined together
- The Two-piece–Implant and abutment are separate. The abutment is secured to the implant by means of an abutment screw
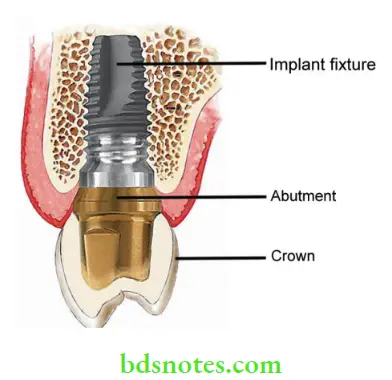
Implant Fixture
- Over the years various implant designs have been developed and used.
- Currently, the most favored form is the cylindrical screw or the tapered screw.
- The implant is inserted through a surgical procedure.
- The abutment is usually screwed onto the implant at a later date.
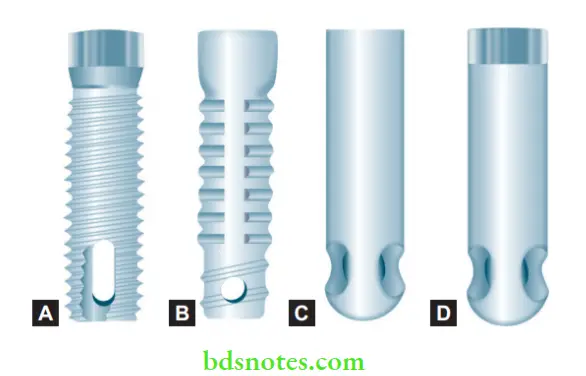
- (A) Titanium screw.
- (B) Hydroxyapatite screw.
- (C) Hydroxyapatite.
- (d) Titanium plasma sprayed.
- The crown is then constructed and either screwed on or cemented onto the abutment thus completing the restoration.
- Implants are usually designed as a system and depending on the company various accessory components are also available.
- The components are usually specific for the particular system and are usually not interchangeable.
- Some of them become part of the implant itself while others aid in the various stages of implant placement and tooth restoration.
- These include drills, healing caps, impression copings, implant analog, laboratory accessories, etc.
Implant Abutments Definition
An implant abutment is that portion of a dental implant that serves to support and/or retain any fixed or removable dental prosthesis (GPT-8).
Classifiation of abutments
1. According to the fabrication procedure
- Stock abutment
- Custom
- CAD/CAM
2. According to the material used
- Titanium
- Zirconia
- Gold
- Steel
3. According to angulation
- Angled
- Nonangled
- Stock abutments: Also known as the preparable, easy, or direct abutments. They are factory produced and provide the most accurate fi to the implant. They can be modified at the chairside or in the laboratory. They come in varying sizes and emergency profiles. Some come with scalloped margins for improved marginal esthetics.
- Stock abutments are of two varieties: Hollow abutments These are abutments with a channel through which the connecting screw attaches it to the implant fixture.
- Solid abutment: The abutment comes with its own built-in screw. The abutment itself is screwed onto the implant.
- Custom Cast: custom abutments have long been a workhorse in implant dentistry. They were first popularized as the “UCLA” abutment design and provided a means for waxing custom emergence profiles of the subgingival portion of the abutment, flexibility in margin level placement, and for correction of angulation problems.
- CAD/CAM: State-of-the-art software and milling machines utilize the scan data from the patient’s dental casts and the computer-generated abutment design to enable the production of an abutment specific to the patient.
- Angled abutments: Angled abutments are used to correct the implant-crown alignment, for example, upper central incisors often need angled abutments.
- Zirconia abutments: Zirconia is a strong tooth-colored ceramic material. These are indicated for patients demanding an increased level of esthetics.
- One-piece implant abutment: Some manufacturers do not provide separate abutments, rather the abutment is combined with the implant and is, therefore, inserted along with the implant.
Equipment And Parts Associated With Implant Surgery
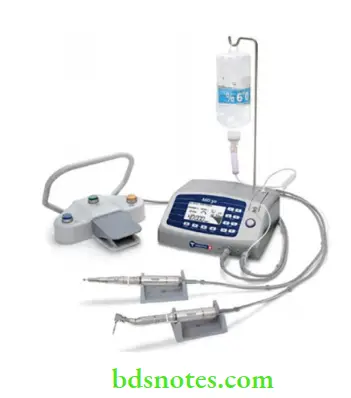
Implant motor
- These are high torque motors with foot control and saline stand.
- The handpiece is contra angled and has a nozzle for saline irrigation.
- Torque ranges from 50–70 Ncm. Speed ranges from 300 to 40,000 rpm.
- Having low speed but high torque is important for implant drilling.
Implant drills
- The pilot drill is the first drill used. It helps to establish the direction of the subsequent drilling and implant placement.
- Subsequent drills are introduced in series of increasing sizes. Drills are usually made of stainless steel.

Cover screw
- Implant surgery is usually done in two stages.
- In the first stage the implant is inserted in the bone and left to integrate for a period of 2 months.
- After the implant is placed, a cover screw is used to cover the coronal end of the abutment.
- The cover screw prevents bony ingrowth and keeps the abutment chamber patent while the implant is integrating.

Healing abutment
- The healing abutment is usually placed 2–3 months later at the second stage.
- The cover screw of the buried implant is exposed.
- The cover screw is removed and a healing abutment is placed instead.
- The healing abutment exposes the implant to the oral cavity and prepares the space for future abutment.
- The healing abutment may be cylindrical or anatomic in design.

The function of the healing abutment
- Allows the punched-out tissue to heal.
- Promotes the development of sulcus epithelium.
- Helps to develop papilla and marginal gingiva, thus improving the soft tissue esthetics.
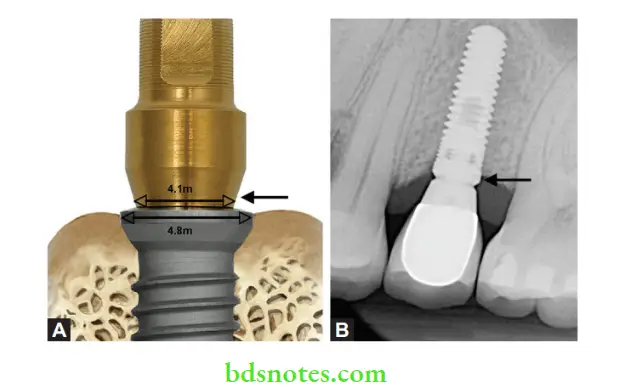
- Helps to develop a proper emergence profile from the implant platform to the crown, thus improving the restoration esthetics (transition from the narrower implant to the broader artificial tooth).
Implant Abutment Connection
- The implant abutment connection is an important part of the implant design.
- It is one of the factors which help in the proper functioning, stability, and longevity of the implant.
- The abutment is secured to the implant with the help of a screw.
- During the occlusal function, considerable stress may be transferred to the screw and can lead to its early loosening or even fracture.
- Manufacturers have, therefore, incorporated certain design features to reduce the stress on the abutment screw.
The function of the implant abutment connection
The implant/abutment interface determines joint strength, stability, and lateral and rotational stability. It also reduces stress on the abutment screw.
Types of implant-abutment connections
There are two ways the implant and abutment connect or interface
- External
- Internal
External Hex
The original Brånemark protocol required several externally hexed implants to restore fully edentulous arches.

Internal Hex
- One of the first internally connected implants was designed with a 1.7-mm-deep hex below a 0.5 mm wide, 45° bevel.
- Its features were intended to distribute intraoral forces deeper within the implant to protect the retention screw from excess loading and to reduce the potential of microleakage.
- Internally connected implants also provide superior strength for the implant/ abutment connection.
- Since the introduction of the internal connection concept, further design enhancements have been made in an attempt to enhance the implant/abutment connection.
- Included in such efforts is the “Morse” taper, wherein a tapered abutment post is inserted into the nonthreaded shaft of a dental implant with the same taper.
- Other internal connection designs have followed, frequently with variations in the number of hexes, connection length, angulation, etc.
Some of the internal implant-abutment connections are
- 3-point internal tripod — Replace select (Noble Biocare)
- 5-point internal pentagon — Tiologic (Dentaurum)
- 6-point internal hex — Frialit 2 (Friadent)
- 8-point internal morse taper — (ITI) Straumann
- 12-point conical seal — Astra (Astra Tech)
Platform Switching
- Platform switching is a method used to preserve alveolar bone levels around dental implants.
- The concept refers to placing an abutment of narrower diameter on implants of wider diameter, rather than placing abutments of similar diameters (referred to as platform matching.

Biointegration And Osseointegration
- For an implant to function, it must integrate with the oral tissues.
- The term osseointegration was first described by Per Ingvar Branemark and refers to the fusion of the bone with the implant.
- Defined as An apparent direct connection of an implant surface and host bone without intervening connective tissue.
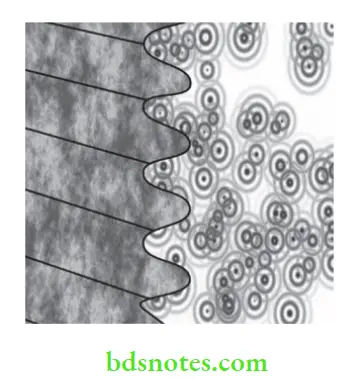
- Thus a direct structural and functional connection between the bone and the implant allows the implant to transmit functional stresses directly to the bone.
- To achieve osseointegration, the bone must be viable, the space between the implant and bone should be less than 10 nm, and contain no fibrous tissue.
- The presence of fibrous tissue usually signifies failure.
Factors favoring osseointegration
- Proper treatment planning
- Atraumatic drilling of bone
- Selection of proper implant material
- Implant design
- Favorable occlusal forces
- Bone quality
- Good oral hygiene
- No contraindicating local or systemic factors
Other factors include the nature of the surface coating and surface configuration.
- Recently there has been interest in coating titanium with certain materials that actively promote a favorable bone response. These are referred to as ‘bioactive’.
- Examples of bioactive materials are hydroxyapatite, tricalcium phosphate, and bioactive glasses. Commercially available bioactive glasses include Bioglass, Ceravital, Biogran, and glass ceramic A.
- These materials are generally too weak and brittle to stand alone.
- However, when used as a coating (50 to 75 µm) on the surface of titanium, it combines the strength of titanium with its bioactive qualities.
- If successful, the ceramic coating becomes completely fused with the surrounding bone.
- In this case, the interphase is termed ‘biointegration’ because there is no intervening space between the bone and the implant.
- Implant material and design is continually evolving. With every passing year the failure rates are gradually reducing.
- Current implants enjoy a 95 to 98% clinical success rate. More advances in both design, material, and technique may be expected in the future.
Titanium Allergy
- In the last couple of years, the question if titanium allergy really exists has been raised in scientific literature.
- The reactions are not necessarily local but appear in other parts of the body.
- One of the reasons why the existence of titanium allergy has been debated might be that the golden standard for metal allergy testing, patch testing, has not been properly developed for titanium.
- The patch test is a skin test, where salts of the metals tested are placed on the skin of the back under occlusion.
- 24–72 hours later a dermatologist evaluates the reaction and the presence of a rash is taken as evidence of a positive reaction.
- Unfortunately, titanium dioxide, a salt of titanium used for patch testing, does not penetrate the skin under the conditions of the patch test.
- This is one of the reasons why patch test in its current form often gives false negative results in patients with titanium-induced inflmmation in the body.
- The latest available research from Europe and Japan shows that between 2–4% of all patients with titanium implants develop an allergic reaction to either titanium or to one or more of the metals used in the titanium alloy.
- The symptoms most often observed after implantation with titanium-containing implants are varied, so they will be different in different patients.
- In addition to symptoms shown adjacent to implants on the mucosa in the mouth, or on the skin on the body, there may be other systemic symptoms.
- These symptoms are akin as those described after exposure to other allergens, like nickel or mercury, in sensitized individuals.
- Symptoms arise because stimulated lymphocytes produce cytokines, which in turn, affect the HPA axis.
- The result is multiple nonspecific symptoms such as profound fatigue, pain, cognitive dysfunction, headache, sleep problems, etc.
- Allergy due to titanium might be accountable for the failure of implants in some cases (known as cluster patients).
- It has been documented that the risk of titanium allergy is more prevalent in patients having sensitivity to other metals.
- In such types of cases, an allergy assessment is suggested to exclude problems related with titanium implants.
Zirconia Implants
- Although titanium is the preferred choice for dental implants as it is an inert material, in rare circumstances, it may encourage toxic or allergic-type 1 or 4 reactions.
- Its high strength, fracture toughness, and its white color make zirconia an interesting material for the construction of implant abutments and superstructures especially in the anterior zone.
Indications for zirconia implant
- Esthetic considerations
- Sensitivity or allergy to titanium
Zirconia implants should be considered in patients with known allergies to titanium. (See the chapter on Dental ceramics for more information on Zirconia implants)

Zirconia Anatomic Root-Form Implants
- Synonyms Root analog implants, anatomic implants, custom implants, bioimplant Zirconia-based anatomic root-form implants were introduced into dental implantology as an alternative to conventional cylindrical implants.
- Owing to its ability to be milled into the shape of the natural tooth root and be placed immediately following extraction, its excellent biomechanical characteristics, biocompatibility, and bright tooth-like color, zirconia has the potential to become a substitute for titanium as dental implant material.

- Immediate placement of an implant similar in shape and size to the extracted root has its own advantages.
- By adapting the root to the extraction socket instead of adapting the bone to a preformed standardized implant they reduced the bone and soft tissue trauma.
- Immediate custom-made root analog implants were possible because of advances in material and CAD/CAM technology. (See the chapter on Dental Ceramics for more information on Zirconia anatomic root-form implants).
Zirconia Anatomic Root Advantages
- Esthetic
- Biocompatible
- Immediate placement
- No additional drilling or surgery required
- No complications of implant surgery
- Shorter waiting period
- Fits into the original socket
- Immediate placement preserves bone and soft tissue (less resorption)
- Preserves root eminences of the alveolar bone
- Sinus lift not required
- Bone graft not required
- Little or no swelling or pain
- Faster recovery time
Implant Surfaces And Coatings
- The implant surface is critical to the proper biointegration of the implant.
- For this purpose, various techniques have been used to modify the implant surfaces to improve its integration to the surrounding tissues.
- The techniques may be classified as
1. Ablative procedures Ablation is the removal of material from the surface of an object by blasting, vaporization, chipping, or other erosive processes.
- Grit blasting
- Acid etching
- Anodizing
- Shot/ laser peening
2. Additive procedures It is a process of creating a layer by the addition of material.
- Plasma spraying
- Electrophoretic deposition
- Sputter deposition
- Soluble gel coating
- Soluble blast media
- Pulsed laser deposition
- Biomimetic precipitation
Grit Blasting
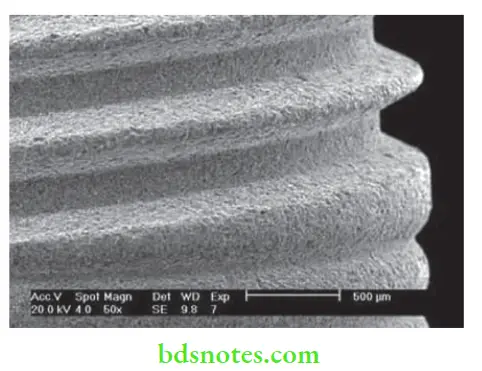
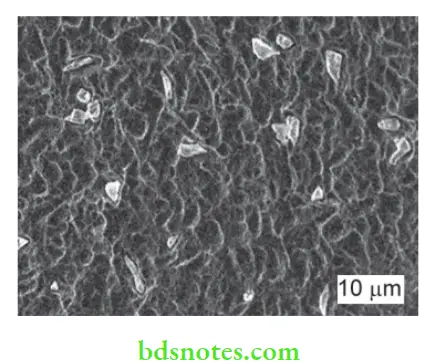
- A rough surface is created by grit-blasting the machined titanium implant surface with hard particles.
- The particles are projected through a nozzle at high velocity by means of compressed air.
- This is followed by washing in non etching acid and distilled water to remove residual blasting material.
- The microtextured surfaces has been shown to allow for increased bone apposition compared to machined surfaces by increasing the surface area.
- Some manufacturers combine both blasting and etching.
Grit blasting materials
- Calcium phosphates like hydroxyapatite (HA) and beta-tricalcium phosphate
- Titanium oxide
- Zirconia
- Alumina
Grit Blasting Disadvantages
In the case of alumina, residual blasting media is often embedded into the implant surface and can interfere with integration.
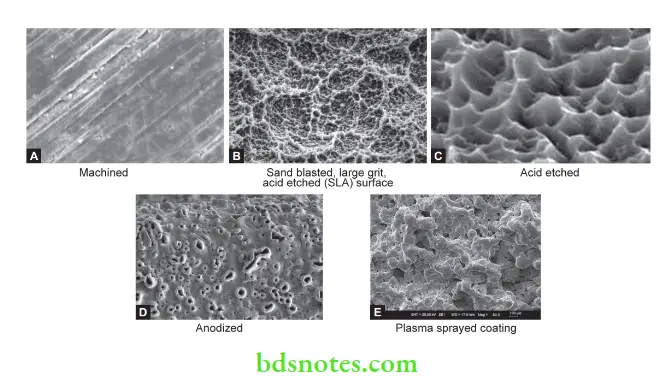
Acid Etching
The implant surface can be roughened through acid etching with sulphuric or hydrochloric acids.
Advantages of acid etching
- Produces a cleaner surface as there is no possibility of an external agent embedding onto the implant surface.
- No possibility of a loss of the layer through debonding, dissolution or wear thus avoiding concerns of long-term fiction.
Anodization
- Anodizing is an electrochemical process used to increase the thickness of the natural oxide layer on the surface of the titanium (to more than 1000 nm). Anodization modifies the microstructure and crystallinity of the titanium oxide layer.
- Anodization is done with the help of strong acids (for example, sulphuric, phosphoric, nitric acids, etc.) at high current density and voltage (200 A/m 2 at 100 V).
Shot/Laser Peening
- Shot peening is similar to sandblasting, where the surface is bombarded with small spherical particles causing small indentations to form.
- Laser peening involves the use of high-intensity pulses of laser to create a regular honeycomb pattern with small pores.
Hydroxyapatite Coated Implants
- Hydroxyapatite (HA) (also called hydroxylapatite or calcium hydroxide phosphate), is a naturally occurring mineral form of calcium apatite with the formula Ca 10(PO4) 6(OH)2.
- Bone is a specialized mineralized connective tissue consisting by a weight of 33% organic matrix, permeated by HA, which makes up the remaining 67% of bone.
- For this reason, HA is being investigated as a possible material for coatings or composites.
Rationale
- The use of hydroxyapatite implants have been reported to stimulate bone healing, resulting in an improvement in the rate and strength of initial implant integration.
- Hence, the dense HA layer on the top of the titanium substrate is mainly for biointegration to bone tissue and enhanced implant stability.
- Thus, it is believed that the use of HA coatings on metallic implants would speed the rehabilitation of patients by decreasing the time from implant insertion to final reconstruction.
Plasma Sprayed Hydroxyapatite
- Numerous methods of depositing HA on metallic implants have been reported.
- The current deposition process is plasma spraying or arc plasma spraying.
- A gas stream (pure argon or a mix of argon/hydrogen) is used to carry HA powder, which is then passed through an electrical plasma produced by a low-voltage, high-current electrical discharge.
- The plasma heats the hydroxyapatite, partially melting it. The semi-molten HA powder is sprayed onto the titanium where it solidifies.
- It has been reported that plasma spraying of HA results in coatings with a thickness greater than 30 µm.
- The bonding of the plasma-sprayed HA coatings appears to be entirely mechanical in nature.
- Besides HA, other materials like titanium can also be plasma sprayed onto the titanium surface.
Problems with plasma-sprayed coatings
Problems cited with the plasma-sprayed coatings include
- Variation in bond strength between the coatings and the metallic substrates
- Alterations in HA structure due to the coating process
- Poor adhesion between the coatings and metallic substrates
Electrophoretic Deposition (EPD) Of HA
- EPD is a process in which colloidal particles of HA suspended in a liquid medium is deposited onto the implant under the influence of an electric field.
- EPD can produce coatings ranging from 1,500.
- Post-deposition heat treatment is required to densify the coating.
- A major disadvantage is the possibility of delamination of the layer in clinical use.
Biomimetic Coating Technique
- Biomimetic coating technique for nucleation and growth of bone-like crystals on a pretreated substrate by immersing it in a supersaturated solution of calcium phosphate under physiological conditions (37 °C and pH = 7.4).
- This method can be modified for the incorporation of drugs or growth factors onto the implant surface thereby making the implants osteoinductive and osteoconductive.
The various brands and their implant surface types are outlined in Table.


Leave a Reply