Cranial Nerves
Question 1: Enumerate the various Cranial Nerves.
Answer. There are 12 pairs of cranial nerves. They are serially numbered from 1 to 12 in craniocaudal order of their attachment on the surface of the brain and designated by Roman numerals as follows:
- Olfactory (1)
- Optic (2)
- Oculomotor (3)
- Trochlear (4)
- Trigeminal (5)
- Abducent (6)
- Facial (7)
- Vestibulocochlear (8)
- Glossopharyngeal (9)
- Vagus (10)
- Accessory (11)
- Hypoglossal (12)
Question 2: Describe the olfactory nerve in brief.
Answer. The olfactory nerve consists of about a dozen filaments, which represent the central processes of the bipolar neurons present in the olfactory epithelium. It is a sensory nerve and carries a sense of smell.
Functional Component Of Olfactory Nerve Special somatic afferent fibres
Origin And Course Of Olfactory Nerve The cell bodies of the olfactory nerves are located in the olfactory epithelium of nasal mucosa. The olfactory nerve begins as a dozen of filaments representing axons of bipolar neurons from the olfactory mucosa of the nasal cavity. These filaments pass through the cribriform plate of the ethmoid to synapse within the olfactory bulb in the anterior cranial fossa.
Applied Anatomy Of Olfactory Nerve The lesions of the olfactory nerve result in loss of smell, which is called anosmia. The sense of smell is also responsible for the finer appreciation of the taste of the food.
Question 3: Describe the optic nerve in brief and mention its unique features.
Answer. The optic nerve is the nerve of sight, i.e. vision.
Functional Components Of Optic Nerve Special somatic afferent fibres for the special sense of sight.
Read And Learn More: Selective Anatomy Notes And Question And Answers
Optic Nerve Origin And Course The optic nerve extends from eyeball to the optic chiasma, which lies above the pituitary fossa containing the pituitary gland. Its fibres arise from the retina and leave the eyeball at the optic disc.
The fibres arising from the nasal half of the retina decussate in the optic chiasma with that of the opposite side and then course along the optic tract of the opposite side, whereas those arising from the temporal half of the retina do not decussate in the optic chiasma and thus run in the optic tract of the same side. The fibres of the optic tract relay in the lateral geniculate body.
Unique Features Of Optic Nerve
- It is not a true peripheral nerve, rather it is a tract of the forebrain.
- It is surrounded by meninges, i.e. dura mater, arachnoid mater and pia mater, and thus by a subarachnoid space containing CSF.
- Its fibres are myelinated by oligodendrocytes and not by Schwann cells. (cf. The fibres of peripheral nerves are myelinated by the Schwann cells.)
- It cannot regenerate if damaged.
Applied Anatomy Of Optic Nerve – The damage of the optic nerve leads to complete blindness on the side of the lesion.
Question 3. Describe the trochlear nerve in brief.
Answer. The trochlear nerve is the smallest cranial nerve.
Trochlear Nerve Functional Components
- General somatic efferent (GSE) fibres supply the superior oblique muscle of the eyeball.
- General somatic afferent (GSA) fibres carry proprioceptive fibres from the superior oblique to the mesencephalic nucleus of CN 5.
Trochlear Nerve Origin, course and Distribution The trochlear nerve arises from the 4th nerve nucleus located in the lower part of the midbrain. Before emerging on the dorsal aspect of the midbrain, its fibres decussate with the fibres of the nerve on the opposite side.
After emerging, it passes forward in the subarachnoid space and pierces the dura mater to run into the lateral wall of the cavernous sinus. The nerve enters the orbit through the superior orbital fissure and supplies the superior oblique muscle of the eyeball.
Trochlear Nerve Applied Anatomy The damage to the trochlear nerve causes diplopia on looking downwards and laterally.
Question 5: Describe the abducent nerve under the following headings: (a) functional components, (b) origin, course and distribution and (c) applied anatomy.
Answer. The abducent is CN 6. It is purely a motor nerve and supplies only one muscle – the lateral rectus of the eyeball.
Abducent Nerve Functional components
- General somatic efferent (GSE) fibres to supply lateral rectus. They arise from the abducent nucleus in the lower part of the pons.
- General somatic afferent (GSA) fibres carry proprioceptive sensation from the lateral rectus to the mesencephalic nucleus of the trigeminal nerve.
Abducent Nerve Origin, course and distribution The abducent nerve arises from the abducent nucleus in the lower part of the pons and emerges from the anterior surface of the brainstem at the junction of the pons and medulla oblongata. After emerging from the brain, it runs at first upwards, forwards and laterally in the posterior cranial fossa and pierces the dura mater over the clivus.
It then turns sharply forward, crossing the sharp superior border of the petrous temporal bone before entering the cavernous sinus. It traverses the cavernous sinus, lying at first lateral and then inferolateral to the internal carotid artery. The nerve enters the orbital cavity through the superior orbital fissure and supplies the lateral rectus muscle.
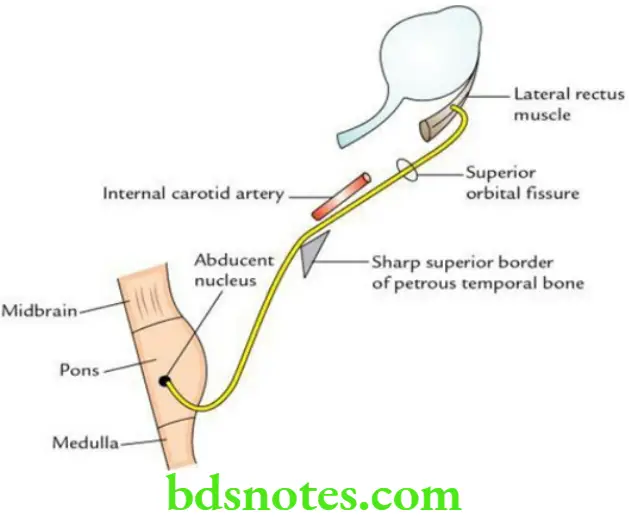
Abducent Nerve Applied anatomy The abducent nerve is a thin motor nerve that takes the longest intracranial course, and hence it is often damaged in increased intracranial pressure associated with coning of the brainstem.
The paralysis of the abducent nerve results in:
- Medial squint
- Diplopia
Question 6: Describe the facial nerve under the following headings: (a) functional components, (b) origin and course, (c) branches and distribution and (d) applied anatomy.
Answer. The facial nerve is the CN 7. It is a mixed cranial nerve (i.e. motor and sensory) but predominantly motor.
Facial Nerve Functional components
- Special visceral event (SVE) fibres supply the muscles of facial expression, etc.
- General visceral event (GVE) fibres supply the lacrimal, submandibular and sublingual salivary glands.
- Special visceral of event (SVA) fibres, which carry taste sensations from the anterior two-thirds of the tongue, except those from vallate papillae.
- General somatic of event (GSA) fibres, which carry general sensation from the concha of the external ear.
Facial Nerve Origin and Course The facial nerve has two roots:
- A large medial motor root and
- A small lateral, sensory root – the nervus intermedius.
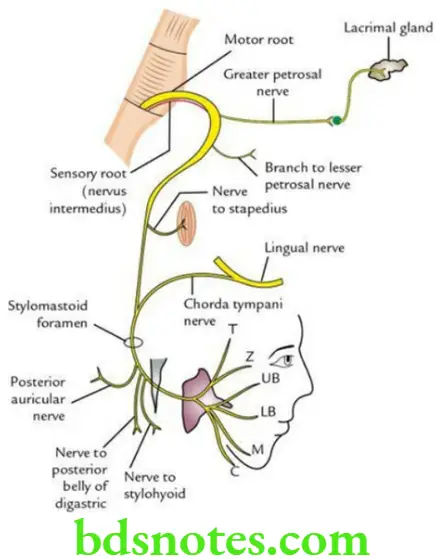
The motor root arises from the motor nucleus of the facial nerve in the pons. The sensory root (nervus intermedius) arises from the nucleus tractus solitaries and superior salivatory and lacrimatory nuclei in the pons.
The two roots of the facial nerve emerge on the anterior surface of the brainstem at the lower border of the pons. They pass forwards and laterally in the posterior cranial fossa along with the vestibulocochlear nerve and enter the internal acoustic meatus.
At the distal end of the internal acoustic meatus, the two roots join to form a single nerve. At the bottom of the meatus, the nerve enters the facial canal. Now, it takes a dubious course in the facial canal through the temporal bone and comes out of the skull through the stylomastoid foramen.
Now it winds around the lateral aspect of the styloid process to enter the parotid gland, where it divides into five terminal branches.
Facial Nerve Branches and distribution
In the facial canal:
- Greater petrosal nerve, which joins the deep petrosal nerve to form the nerve of the pterygoid canal (Vidian’s nerve). This nerve carries parasympathetic secretomotor fibres to the lacrimal, nasal and palatine glands.
- Nerve to stapedius.
- Chorda tympani nerve: It arises about 5 cm above the stylomastoid foramen and joins the lingual nerve in the infratemporal fossa. The chorda tympani nerve serves the following functions:
- Carries taste sensations from the anterior two-thirds of the tongue, except from vallate papillae.
- Supplies secretomotor fibres to the submandibular and sublingual salivary glands.
At the stylomastoid foramen (after emerging from the facial canal):
- Nerve to the posterior belly of digastric
- Nerve to stylohyoid
- Posterior auricular nerve to supply occipital belly of occipitofrontalis
The parotid gland, gives rise to five terminal branches to supply muscles of facial expression:
- Temporal
- Zygomatic
- Buccal (upper and lower buccal)
- Mandibular
- Cervical
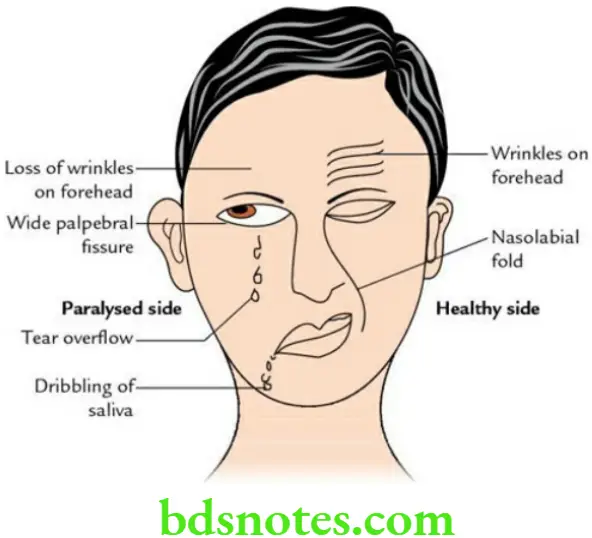
Facial Nerve Applied anatomy
- Facial nerve paralysis:
The effects of paralysis of CN VII depend on the site of the lesion. The complete paralysis of the facial nerve manifests as follows:- Loss of lacrimation due to involvement of lacrimal nerve and inability to close the eye to paralysis of orbicularis oculi. This leads to:
- Inability to close the eye on the affected side due to paralysis of orbicularis oculi.
- Exposing the cornea to the air and loss of lacrimation due to the involvement of secretomotor fibres to this gland leads to corneal dryness and keratitis.
- The angle of the mouth goes down and the dribbling of saliva due to paralysis of orbicularis oris.
- Accumulation of food bolus in the vestibule of the mouth on the affected side due to paralysis of the buccinator muscle.
- Speech becomes defective due to paralysis of lip muscles.
- Hyperacusis is a result of loss of control of movements of the stapes following paralysis of the stapedius.
- Loss of taste sensations in the anterior two-third of the tongue, due to paralysis of the chorda tympani nerve.
- Loss of lacrimation due to involvement of lacrimal nerve and inability to close the eye to paralysis of orbicularis oculi. This leads to:
- Bell palsy: It is a lower motor neuron type of facial palsy, which occurs due to compression of the facial nerve into the facial canal just above the stylomastoid foramen following its inflammation and swelling, probably due to viral infection.
Facial Nerve Clinical features
Facial asymmetry, i.e. face of the paralysed side is pulled to the opposite/healthy side
- Loss of wrinkles on the forehead
- The inability to close the eye causes a wide palpebral fissure
- The inability of the angle of the mouth to move up while laughing
- Loss of nasolabial furrow
- Accumulation of food in the vestibule mouth
- Dribbling of saliva from the angle of the mouth
- Inability to inflate/blow the cheek properly
Question 7: Briefly describe the vestibulocochlear nerve.
Answer: It is the nerve of hearing and balance (i.e. special sense).
It consists of two parts: vestibular and cochlear. Both are purely sensory.
- The vestibular nerve helps in maintaining balance, whereas the cochlear nerve carries a sense of hearing.
- The cochlear nerve carries sensations from the spiral organ of Corti within the cochlear duct of the internal ear. It is formed by the central processes of nerve cells of the spiral ganglion of the cochlea. It comes out of the temporal bone through the internal acoustic meatus and reaches the lower border of the pons. Here, it enters the pons to end in ventral and dorsal cochlear nuclei situated on the ventral and dorsal aspects of the inferior cerebellar peduncle, respectively.
- The vestibular nerve carries sensations from the maculae of utricle and saccule, and cristae ampullaris of semicircular ducts of the internal ear. It is formed by the central processes of nerve cells of the vestibular ganglion in the distal part of the external acoustic meatus.
- It passes into the cranial cavity through the internal acoustic meatus and reaches the lower border of the pons, where it enters the pons to end in the vestibular nuclei located in the floor of the 4th ventricle.
Question 8: Describe the glossopharyngeal nerve under the following headings:
- Functional components,
- Origin and course,
- Branches and distribution and
- Applied anatomy.
Answer:
The glossopharyngeal nerve is CN IX. It is a mixed nerve (motor and sensory) but predominantly sensory.
Vestibulocochlear Nerve Functional components
- Special visceral of erent (SVE) fibres supply the stylopharyngeus muscle.
- General visceral of erent (GVE) fibres, which supply the secretomotor fibres to the parotid gland.
- Special visceral of erent (SVA) fibres, which carry taste sensations from the posterior one-third of the tongue including vallate papillae.
- General visceral of erent (GVA) fibres, which carry general sensations from the skin of the auricle.
Vestibulocochlear Nerve Origin and Course The glossopharyngeal nerve arises from its nuclei in the brainstem and emerges on the surface from the lateral aspect of the medulla in the groove between the olive and inferior cerebellar peduncle and enters the jugular foramen.
After emerging from the jugular foramen, it descends vertically between the internal jugular vein and internal carotid artery for some distance, then curves around the lateral surface of the stylopharyngeus, and passes forward into the tongue.

Vestibulocochlear Nerve Branches and distribution
- Tympanic nerve (Jacobson’s nerve), carrying secretomotor fibres to the parotid gland
- Nerve to stylopharyngeus
- The pharyngeal branch to the pharyngeal plexus
- Sinus nerve to carotid sinus and carotid body
- Terminal branches to the posterior one-third of the tongue including vallate papillae, tonsil, soft palate and epiglottis
Vestibulocochlear Nerve Applied anatomy
- The paralysis of the glossopharyngeal nerve leads to loss of gag reflex and loss of general and taste sensations in the posterior one-third of the tongue.
- The glossopharyngeal nerve is tested clinically by:
- Eliciting gag reflex: The tickling of the posterior wall of the oropharynx/soft palate/tonsillar region causes reflex contraction of pharyngeal muscles leading to gagging and retching.
- Note: The afferent limb of the gag reflex is formed by the glossopharyngeal nerve, while its efferent limb is formed by the vagus nerve.
- Testing sensations (general and taste) in the posterior one-third of the tongue including vallate papillae.
Question 9: Describe the origin, course and branches of the vagus nerve in the neck.
Answer:
The vagus nerve is CN 10. It is the longest cranial nerve and has a vague course.
Vagus Nerve Origin and course
- The vagus nerve arises from nuclei within the brainstem and emerges on the surface from the lateral aspect of the medulla in the groove between the olive and inferior cerebellar peduncle, and comes out of the cranial cavity through the jugular foramen.
- After emerging from the cranial cavity, it descends vertically between the internal jugular vein and the internal carotid artery. At the root of the neck, the nerve enters the thorax. The right vagus nerve enters the thorax by crossing in front of the right subclavian artery, while the left vagus nerve does so by passing between the left common carotid and left subclavian arteries.
Vestibulocochlear Nerve Branches of the vagus nerve in the neck
- Meningeal branch to dura mater of posterior cranial fossa
- Auricular branch (Aldermen’s nerve/Arnold’s nerve) to the skin of external acoustic meatus
- Pharyngeal branch to pharyngeal plexus
- Superior laryngeal nerve
- Recurrent laryngeal nerve (on the right side only)
- Cardiac branches (cervical)
Question 10: Describe the origin, course, distribution and applied anatomy of the accessory nerve.
Answer:
The accessory nerve is the CN 11. It is purely a motor nerve and consists of two roots – cranial and spinal.
Accessory Nerve Origin and Course
- The cranial root arises from the nucleus ambiguus in the medulla oblongata. It emerges on the surface of the medulla between the olive and inferior cerebellar peduncle.
- The spinal root arises from the upper five cervical spinal segments.
- The spinal root ascends to enter the cranial cavity through the foramen magnum. It then turns laterally to join the cranial root. The united roots leave the skull through the jugular foramen, but just outside the foramen, they separate again.
Accessory Nerve Distribution The spinal root descends in the neck to supply the sternocleidomastoid and trapezius muscles. The cranial root joins the vagus and is distributed through its branches. The distribution of the cranial root of the accessory nerve is as follows:
- It supplies all the muscles of the palate through the pharyngeal plexus except the tensor tympani, which is supplied by the mandibular nerve.
- It supplies all the muscles of the pharynx through the pharyngeal plexus except the stylopharyngeus, which is supplied by the glossopharyngeal nerve.
- It supplies all the intrinsic muscles of the larynx through superior and recurrent laryngeal nerves (branches of the vagus nerve).
Accessory Nerve Applied anatomy The lesion of the accessory nerve leads to paralysis of the sternocleidomastoid and trapezius. It is tested clinically:
- By asking the patient to shrug his/her shoulder (trapezius) against the resistance.
- By asking the patient to turn his/her face to the opposite side (sternocleidomastoid) against the resistance.
Question 11: Describe the hypoglossal nerve under the following headings:
- Hypoglossal Nerve Functional components,
- Hypoglossal Nerve Course and relations,
- Hypoglossal Nerve Branches and distribution and
- Hypoglossal Nerve Applied anatomy.
Answer:
The hypoglossal nerve is CN 11. It is purely a motor nerve.
Hypoglossal Nerve Functional components General somatic efferent (GSE) fibres supply the muscles of the tongue.
Hypoglossal Nerve Course and Relations The hypoglossal nerve arises from the hypoglossal nucleus located in the upper part of the medulla oblongata. It emerges from the anterior surface of the medulla between the olive and pyramid as 10–15 rootlets.
The fibres run anterolaterally and leave the posterior cranial fossa through the hypoglossal canal (anterior condylar canal). After emerging from the skull, it runs vertically downwards between the internal jugular vein and the internal carotid artery.
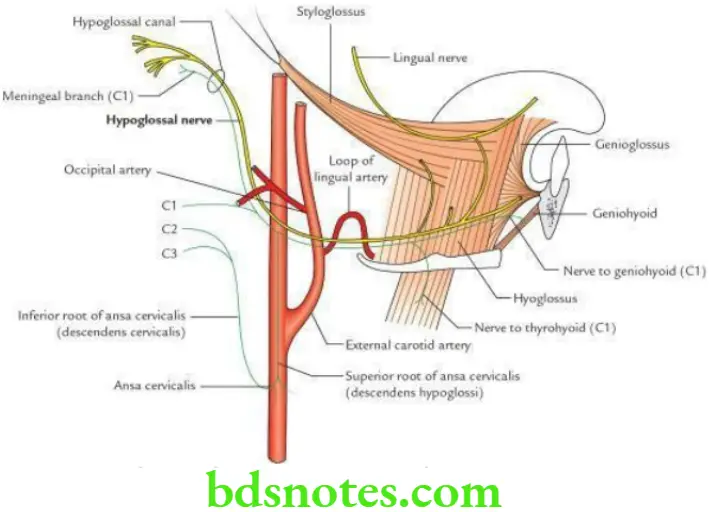
At the lower border of the digastric (i.e. at the level of the angle of the mandible), the nerve curves forward horizontally, crossing in front of internal and external carotid arteries, hooking around the origin of the occipital artery, crossing in front of the loop of lingual artery, and then runs on the superficial surface of hyoglossus. At the anterior border of the hyoglossus muscle, it enters the genioglossus and breaks up into terminal branches.
Hypoglossal Nerve Branches and distribution
- Branches of the hypoglossal nerve proper: They supply all the muscles of the tongue (intrinsic and extrinsic) except palatoglossus, which is supplied by the cranial root of the accessory via the pharyngeal plexus.
- Branches of hypoglossal nerve containing C1 fibres:
- The ventral ramus of the 1st cervical nerve, C1 joins the hypoglossal nerve below the skull. The fibres of C1 are distributed through the following branches of the hypoglossal nerve as follows:
- Meningeal branch
- Descendants hypoglossal/superior root of ansa cervical
- Nerve to thyrohyoid
- Nerve to geniohyoid
Hypoglossal Nerve Applied anatomy The lesion of the hypoglossal nerve leads to paralysis of all the muscles of the tongue on the side of the lesion. This leads to deviation of the tongue on the side of the lesion protruding the tongue.
Hypoglossal Nerve Clinical Testing: The hypoglossal nerve is tested clinically by asking the patient to protrude his/her tongue.
In the lesion of the hypoglossal nerve, the protruded tongue deviates to the same side, i.e. side of the lesion. Thus, the deviated position of the protruded tongue indicates the side of the lesion.

Leave a Reply