Question 1. Discuss the composition and functions of blood.
Answer:
Compsotion of blood:
- Formed elements – blood cells – 45%.
- Erythrocytes or red blood corpuslces (RBC’s)
- Normal count -5 million/ul
- Leucocytes or white blood corpuscles (WBC’s)
- Normal count – 4,000 – 11,000/μl
- Platelets or thrombocytes.
- Normal count – 1.5-4 lacs/ul
- Erythrocytes or red blood corpuslces (RBC’s)
- Plasma-55%.
- It is a clear, straw colored fluid portion of the blood.
- It contains.
- 91-92%-water.
- 8-9% solids.
- 1% inorganic molecules.
\(-\mathrm{Na}^{+}, \mathrm{Ca}^{2+}, \mathrm{K}^{+}, \mathrm{Mg}^{2+}, \mathrm{Cl}^{-}, \mathrm{HCO}_3^{-}, \mathrm{PO}_4^{3-}, \mathrm{Fe}^{2+}, \mathrm{Cu}^{2+}\) - 8% organic molecules.
- Plasma proteins – albumin, globulin, fibrinogen. Amino acids- essential and non-essential.
- Carbohydrates – glucose.
- Fats – triglycerides, cholesterol, phospholipids. Internal secretions – esterase
- Nonprotein nitrogenous substances – ammonia. Antibodies.
- 1% inorganic molecules.
- Gases:
- Oxygen, carbon dioxide, nitrogen.
Read And Learn More: BDS Previous Examination Question And Answers
Functions of blood:
- Nutritive.
- Blood carries the food absorbed from the digestive system to tissues for growth and production of energy.
- Respiratory.
- Blood transport oxygen from lungs to the tissues and carbon dioxide from the tissues to the lungs.
- Excretory.
- Waste products are carried through blood to excretory organs like kidney, skin and intestine.
- Transport of hormones and enzymes.
- Blood transports the hormones secreted from the endocrine glands to their target organs/tissues.
- Blood also transports enzymes.
- Regulation of water balance.
- Water balance is regulated as the water content of the blood gets interchangeable with interstitial fluid.
- Regulation of acid base balance – pH.
- Blood maintains pH through the buffering system of plasma proteins and haemoglobin.
- This mechanism is called homeostasis.
- Regulation of body temperature.
- Blood regulates body temperature due to its high specific heat.
- It regulates through thermoregulatory mechanism due to which balance occurs between heat loss and heat gain in the body.
- Storage function.
- Blood stores substances like proteins, glucose, sodium and potassium so that these substances can be used during starvation, fluid loss, etc.
- Defensive function
- White blood cells help in the defense of the body.
Read And Learn More: BDS Previous Examination Question And Answers
Question 2. Give the composition of blood and write about the importance of plasma.
Answer:
Plasma:

Question 3. Enumerate plasma proteins giving normal values. Explain any five functions of plasma protein. (or) Mention the functions of plasma proteins.
Answer:

Plasma Functions:
1. Coagulation – fibrinogen, prothrombin and antihemophilic globulin are involved in coagulation of blood.
2. Immunity they – globulins known as immunoglobulins produces antibodies which provide immunity to the body.
- There are 5 types of immunoglobulins IgA, IgG, IgD, IgE and IgA.
- The antibodies produced react with antigens of various micro-organisms which causes disease like diphtheria, typhoid, measles.
3. Colloidal osmotic pressure.
- It is inversely proportional to the molecular size and shape and is directly related to the concentration of molecules.
- Therefore, as albumin concentration is more in blood, it exerts maximum pressure, next is globulin and least is fibrinogen.
4. Transport media.
- Plasma proteins help in the transport of certain substances like hormones, enzymes, metals, drugs, dyes, CO2 etc.
- Albumin, alpha globulin and beta globulin help in the transport of the hormones, enzymes, etc.
- While alpha and beta globulin help in the transport of metals in the body.
5. Erythrocyte sedimentation rate.
- Globulin and fibrinogen accelerates rouleaux formation which is responsible for erythrocyte sedimentation rate of the blood.
6. Viscosity.
- Viscosity of blood is important to maintain the normal blood pressure.
- Albumin provides maximum viscosity than the other plasma proteins.
7. Buffer mechanism.
- Plasma proteins especially albumin act as buffers and regulate acid base balance in the blood.
8. Reservior function.
- Plasma proteins stores proteins and break them into amino acids when needed by the body.
- So, they are called “reserve proteins”.
9. Suspension stability of the blood.
- Globulin and fibrinogen helps in the suspension stability of the blood.
Question 6. What is haemoglobin? Describe the types, functions and fate of haemoglobin.
Answer:
Hemoglobin:
- The red, oxygen carrying pigment in the RBCs of vertebrates is haemoglobin.
- It consists of the protein (globin) united with the pigment ‘heme’.
Types of Hemoglobin:
- Adult haemoglobin (HbA).
- Adult haemoglobin (HbA).
- Subtypes:
- (Haemoglobin A (α2 B2).
- Hemoglobin A2 (α2 B2)
- It appears in foetus, after 5 months of intra-uterine life.
- Its life span is 120 days.
- Foetal haemoglobin (HbF).
- It has 2 a chains and 2 y (gammchains.
- It has greater affinity for oxygen.
- It is 70% saturate at 20 mm Hg of pO2 pressure.
- Its life span is 80 days.
- Hemoglobin S (HbS).
- In each ẞ- polypeptide chain of HbA at position 6, one glutamic acid is replaced by valine.
- It is inherited as mendelian dominant.
Hemoglobin Functions:
- To carry respiratory gases – oxygen and carbon dioxide.
- Helps in acid base regulation.
- Transport of nitric oxide from lungs the tissue causing vasodilation.
Hemoglobin Normal values:
- Adult:
- Males – 14-18 gm/dL
- Females 12-15.5 gm/dL
- Children 18 – 22 gm/dL
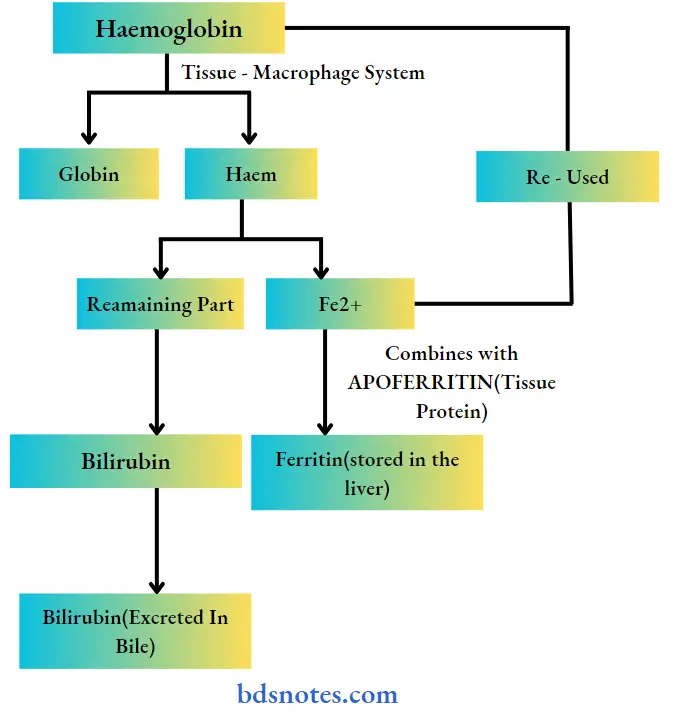
- Fate of Hemoglobin:
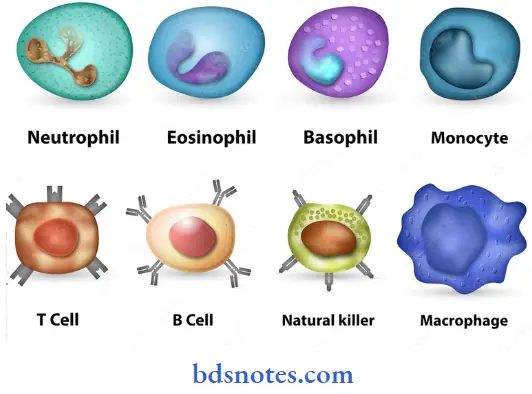
Question 7. Classify WBCs and describe their function with diagrams.
Answer:
WBC [White Blood Corpulscles]:
- Synoym – leukocytes.
- They are the colorless and nucleated formed elements of blood.
- They play an important role in defense mechanism.
White Blood Corpulscles Classification:
- WBC are classified on the basis on the presence or absence of granules in the cytoplasm.
- Granulocytes – with granules
- Neutrophils
- Eosinophils
- Basophils.
- Agranulocytes – without granules.
- Monocytes.
- Lymphocytes.
- Granulocytes – with granules
White Blood Corpulscles Neutrophils 60-70%:
- Size-10-12 μ diameter
- Nucleus is multilobed [2-5 lobes].
- Young nucleus have single “horse shoe shape’ nucleus.
- Cytoplasm contains fine granules containing many enzymes like myeloperoxidase and proteases.
White Blood Corpulscles Eosinophils – 2-5%:
- Size-10-14 μ diameter.
- Nucleus is bilobed.
- Cytoplasm is granular, acidophilic.
- Granules contains peroxidise and lysozomes.
White Blood Corpulscles Basophils 0-1%:
- Basophils Size: 8-10 m diameter
- Nucleus is bilobed.
- Cytoplams contains basophilic coarse granules.
White Blood Corpulscles Monocytes: 3-8%:
- Nucleus is round, oval, horse shoe or kidney shaped.
- Monocytes Size: largest, 14-18 μ diameter.
- Cytoplasm is clear.
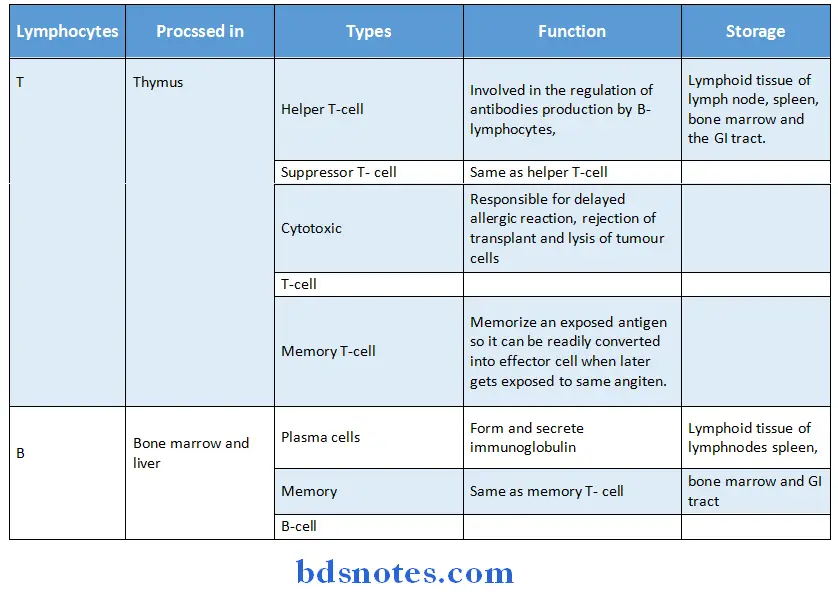
White Blood Corpulscles Lymphocytes – 20-30%:
Lymphocytes Size:
- Large lymphocytes – 10-12 μ diameter and
- Small lymphocytes-7-10 μ diameter.
- Nucleus is large, oval or kidney shaped.
- Functional types are
- T lymphocytes
- B lymphocytes.

Question 8. Describe the mechanism of coagulation of blood mention different anticoagulants and mechanism of action. (or) Anticoagulants. (or) Coagulation of blood.
Answer:
Coagulation:
Coagulation or clotting is the process in which blood losses its fluidity and becomes a jelly like mass few minutes after it is shed out or collected in a container.
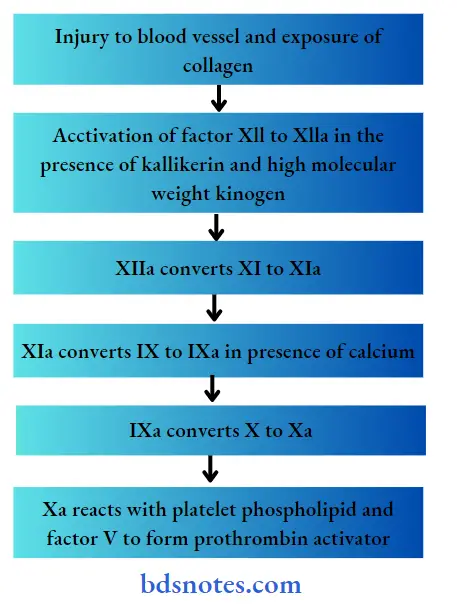
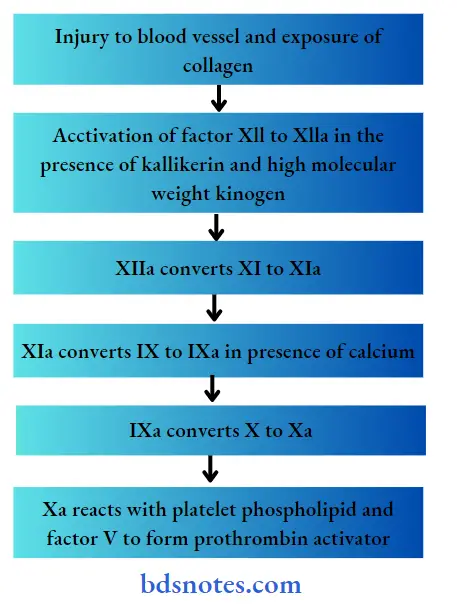
- Coagulation Mechanism:
- The coagulation of blood involves a ‘complex series’ or ‘cascade’ of reactions.
- The clotting of blood occurs in three stages.
1. Formation of Prothrombin activator:
- Prothrombin activator is formed in two ways.
- Extrinsic pathway:
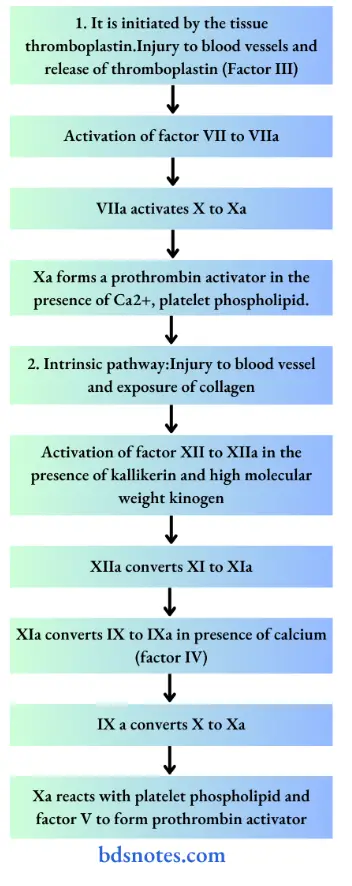
2. Conversion of prothrombin into thrombin:
- Prothrombin activator converts prothrombin into thrombin in the presence of calcium.
- The thrombin thus formed initiates the formation of further molecules of thrombin.
- This activates factor V which accelerates both extrinsic and intrinsic pathway for the formation of prothrombin activator.
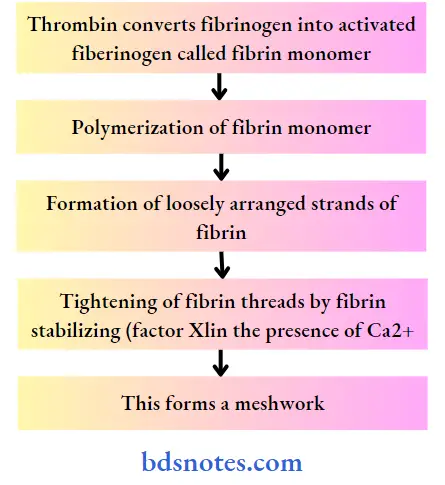
3. Conversion of Fibrinogen into fibrin:
Anticoagulants and its mechamism:
1. Heparin:
- It is naturally occurring anticoagulant.
- It is produced by mast cells and circulating basophils.
- It is present in liver and lungs.
Heparin Mechanism:
- Suppresses the activity of thrombin.
- Combines with heparin cofactor and shows anticoagulant action.
- Activates antithrombin III
- Combines with antithrombin III and removes thrombin from circulation.
- Inactivates the active form of clotting factors IX, X, XI and XII
2. Coumarin dervicaties [Dicoumoral and warfarin]:
- It inhibits the action of vitamin K.
- As vitamin K is essential for the formation of various clotting factors like VII, IX and X, it inhibits coagulation.
3. EDTA (Ethylenediaminetetra acetic acid):
- It prevents blood clotting by removing calcium from blood
4. Oxalate compounds and citrates:
- These combines with calcium and forms insoluble calcium oxalate and calcium citrate respectively,.
- This reduces the calcium level of blood which prevents blood clot.
Question 9. Why does blood not normally clot in the circulating blood? Give three main steps in the clotting of blood. What is the role of aspirin in blood coagulation?
Answer:
- Blood does not normally clot in the circulating blood because of the following.
-
- Smoothness of endothelial lining prevents platelets adhesion and extension of clot into blood vessel.
- Negatively charged particles present over endothelial lining repel the clotting factors.
- All the clotting factors are in inactive form.
- Continuous movement of blood.
- Presence of natural anticoagulants like heparin in the blood.
- Activation of fibrinolytic system.
- Removal of activated clotting factors from the circulation by the liver.
- Steps in the clotting of blood:
-
- Formation of prothrombin activator.
- Conversion of prothrombin into thrombin.
- Conversion of fibrinogen into fibrin.
- Role of aspirin in blood coagulation:
- Thromboxane A2 promotes platelet aggregation.
- Aspirin irreversibly inhibits platelet cyclocygenase and thereby inhibits the synthesis of thromboxane A2.
- It therefore interferes with platelet aggregation and prolongs bleeding time.
Question 10. What is the basis of classification of blood groups and what are the uses of blood grouping? Add a note on Rh+ blood. (or) Rh incompatibility. (or) Rh group.
Answer:
Classification of blood groups:
- It is based on the presence or absence of a specific agglutinogen or antigen on the surface of the red cell membrane.
- The most important blood groups are:
1. ABO system.
- It is based on the presence of absence of antigen A and antigen B blood is divided into 4 groups.

2. Rh Blood group.
- Rh factor is an antigen present in RBC.
- It was first discovered by Landsteiner and Weiner in rhesus monkey.
- The persons having D antigen are called Rh positive and those without D antigen are called Rh negative.
- Rh antibodies are of the IgG type and the antigen – antibody reaction occurs best at the body temperature.
Principles of blood grouping:
- Blood grouping is done on the basis of agglutination which means clumping of RBCs
- Agglutination occurs when a specific antigen called iso aggulatinin.
- Thus, agglutination occurs when antigen A is mixed with Anti-A or when antigen B is mixed with Anti-B.
Uses of blood grouping:
- In blood transfusion to avoid blood transfusion reactions.
- For matching tissues during organ transplantation.
- Investing cases of paternity disputes.
- If one knows his/her blood group, it may be helpful in emergency conditions.
- In pregnancy to prevent the complications due to Rh incompatibility.
- For research purposes.
- Anthropological purposes.
Rh blood:
- Rh blood group system is not detected in tissues other than RBCs.
Rh blood Inheritance:
- Rh factor is an inherited dominant factor.
- It is inherited from both the parent.
- It may be homozygous positive DD, heterozygous negative Dd, or homozygous negative dd.
Rh antibody:
- It is not usually present in the plasma.
- But, its production can be evoked in Rh negative individuals by.
- Transfusion with Rh positive blood.
- Entrance of Rh-positive blood from foetus into the circulation of Rh negative mother.
Rh Complication:
- When Rh negative person receives Rh positive blood for the first time, he is not much effect but antibodies are produced within one month.
- These are lysed by macrophages and a mild delayed transfusion reaction occurs.
- But when the received Rh positive blood for the second time, severe transfusion reaction occurs immediately which may lead to jaundice, cardiac shock or renal shutdown.
- When a Rh negative mother carries a Rh positive fetus, usually the first child escapes the complications of Rh incompatibility.
- At the time of delivery the Rh antigen from foetal blood leaks into mother’s blood.
- When the mother conceives for the second time and if the fetus happens to be Rh positive again, the Rh antibody from mother’s blood enters the fetal blood.
- This causes agglutination of fetal RBCs resulting in hemolysis.
Rh Prevention:
- Anti D should be administered to the mother at 28th and 34th weeks of gestation.
- Anti D should be administered to the mother within 48 hours after delivery.
Question 11. Name different blood group systems. What is the importance of determination of blood groups? What are effects of mismatched blood transfusion. (or) Blood groups. (or) Mismatched blood transfusion reaction. (or) Blood groups.
Answer:
Blood groups systems:
1. ABO system.
- It is based on the presence or absence of antigen A and antigen B.
2. Rh system.
- Rh factor is an antigen present in RBC, also called D antigen.
- The persons having D antigen are called Rh positive and those without it are called Rh negative.
3. Lewis blood group.
- Found by Mrs. Lewis.
- The antibodies found in her reacted with the antigens found in RBCs and in body fluids.
4. MNS blood groups.
- These are determined by their reactions with anti-M, anti-N and anti-S.
5. Other blood groups.
- Auberger groups, diego group, Bombay group, I group, Kell group, kidd group, etc..
Importance of blood groups:
- Blood groups are important for its various uses.
Effects of mismatched blood transfusion:
- If the donor’s plasma contains antibodies against recipient’s RBC, they get diluted in recipient’s blood and thus agglutination does not occur.
- But if the receipient’s plasma contains antibodies against donor’s RBC, the donor’s RBCs are agglutinated and destroyed.
- This leads to release of large amount of free haemoglobin which further results into.
- Jaundice.
- The released free haemoglobin gets degraded and forms bilirubin.
- When the serum bilirubin level is increased above 2 mg% jaundice occurs.
- Cardiac shock.
- Released haemoglobin.
- This free haemoglobin is released into plasma and increases its viscocity.
- This increases the cardiac work load leading to cardiac failure.
- Hemolyzed cells.
- The toxic substances released from hemolysed and develop circulatory shock.
- Renal sutdown.
- The toxic substances from hemolysed cells cause.
- Constriction of renal blood vessel.
- They enter renal tubules, gets precipitated and obstruct these tubules.
- This suddenly stops urine formation.
- This is called renal shutdown.
- Released haemoglobin.
- Jaundice.
Question 12. What is the normal blood volume? What are the methods used for determining blood volume? Describe the various causes of hypovolemia.
Answer:
Normal blood volume:
- The total amount of blood that is present in the circulatory system, blood reservoirs, tissues and organs constitute blood volume.
Value:
- 7% (6-8%) of total body weight.
- 2.8-3.1 liters per square.
Methods for determining blood volume:
1. Direct method:
- Employed by Welcker in 1854 in animals.
- In this method, first the animal is killed and its blood is collected.
- Next, the blood vessels and tissues are washed thoroughly with known amount of water/saline. This is added to the blood collected.
- The total volume is measured.
- The amount of water/saline used is deducted from it to obtain volume of blood.
2. Indirect method:
- It is used to measure the blood volume in human beings.
- It includes 2 steps.
- Determination of plasma volume.
- It is determined by 2 methods.
- Indicator/dye dilution technique.
- 10 ml of blood is collected from the subject and is divided into 2 equal parts.
- A known amount of dye is added to one part and this is used as control.
- Now, a known amount of dye is injected intravenously.
- After 10 minutes, blood sample is collected.
- Similary another 4 samples are collected at the interval of 10 minutes.
- These 5 samples are then centrifuged and plasma is separated.
- From each plasma sample, concentration of dye is measured and average concentration of dye is found.
- Subject’s urine is also collected and the amount of dye excreted is urine is measured.
- Now, the plasma volume is determined by the formula.
- \(\text { Volume }=\frac{\text { Amount of dye injected }- \text { Amount of dye excreted }}{\text { Average concentration of dye in plasma }}\)
- Radioisotope method:
- Radioactive iodine is injected and after sometime blood sample is collected.
- Radioactivity is determined by using appropriate counter and from it plasma volume is determined.
- Indicator/dye dilution technique.
- Determination of blood volume-hematocrit value.
- Blood is collected and mixed with anticoagulant.
- It is then collected in hematocrit tube and centrifuged.
- As a result, red blood cells gets collected at the bottom of the tube.
- This gives packed cell volume (PCV).
- If this is deducted from 100, the percentage of plasma is known.
- Now, blood volume is calculated by blood volume = \(\frac{100 \times \text { Amount of plasma }}{100-\mathrm{PCV}}\)
- It is determined by 2 methods.
Causes of hypovolemia:
- Hemorrhage – acute or chronic.
- Fluid loss.
- Hemolysis.
- Anaemia.
- Obesity blood volume is less compared to body weight.
- Hypothyroidism – blood volume decreses due to reduction in plasma volume and RBC count.
Question 13. Mention the clotting factors in proper order. Explain the intrinsic mechanism of blood clotting. Add note on haemophilia.
Answer:
Clotting factors:
- Factor I – Fibrinogen
- Factor II – Prothombin
- Factor III – Thromboplastin
- Factor IV Calcium
- Factor V – Labile factor
- Factor VI – Not present
- Factor VII – Stable factor
- Factor VIII- Antihaemophilic factor
- Factor IX – Christmas factor
- Factor X-Stuart Prower factor
- Factor XI – Plasma thromboplastin antecedent
- Factor XII-Hegman factor
- Factor XIII – Fibrin stabilizing factor
Intrinsic mechanism of clotting:
Haemophilia:
- It is a sex linked inherited disease characterized by prolonged clotting time
Causes:
- Haemophilia occurs due to lack of formation of prothrombin activator
- Causes differ according to the type
- Haemophilia A
- It is caused due to deficiency of factor VIII of coagulation.
- Haemophilia B
- It is caused due to deficiency of factor IX of coagulation.
- Haemophilia A
Question 14. Dehydration.
Answer:
Dehydration Definition:
- Significant decrease in water content of the body is known as dehydration.
Dehydration Classification:
1. Based on amount of fluid loss.
- Mild dehydration – fluid loss is about 5%.
- Moderate dehydration – fluid loss is about 10%.
- Severe dehydration – fluid loss is about 15%
2. Based on ratio between water loss to sodium loss.
- Isotonic dehydration – balanced loss of water and sodium
- Hypertonic dehydration – more of water loss than sodium
- Hypotonic dehydration – more of sodium loss than water.
Dehydration Causes:
- Severe diarrhoea and vomiting.
- Excessive urinary output due to
- Renal disorders.
- Endocrine disorders.
- Excessive sweating
- Insufficient intake of water.
- Use of diuretics.
Dehydration Features:
- Mild to moderate dehydration lead to
- Dryness of mouth.
- Decrease in sweating
- Decrease in urine formation.
- Excessive thirst
- Decrease in elasticity of skin.
- Severe dehydration lead to
- Decrese in blood volume and cardiac output.
- This leads to hypovolemic shock.
- Very severe dehydration leads to
- Damage to vital structures.
- Coma
- Renal failure.
Question 15. Composition and functions of blood.
Answer:
1. Formed elements – blood cells – 45%.
- Erythrocytes or red blood corpuscles.
- Leucocytes or white blood corpuscles.
- Thrombocytes or platelets.
2. Plasma 55%
- It contains.
- 91-92% – water.
- 8-9% – solids.
- 1% inorganic molecule.
- \(\mathrm{Na}^{+}, \mathrm{Ca}^{2+}, \mathrm{Mg}^{2+}, \mathrm{K}^{+}, \mathrm{Cl}^{-}, \mathrm{HCo}_3^{-}, \mathrm{PO}_4^{3-}, \mathrm{Fe}^{2+}, \mathrm{Cu}^{2+},\)
- 8% organic molecules.
- Plasma proteins.
- Amino acids
- Carbohydrates
- Fats
- Internal secretions.
- Enzymes
- Nonprotein nitrogenous substances
- Antibodies.
- 1% inorganic molecule.
- Gases.
- Oxygen, carbon dioxide, nitrogen.
Question 16. Name three chief plasma proteins. Give the function of each.
Answer:
Plasma Proteins and their function:
1. Albumin 55%:
- It forms the major bulk of plasma proteins.
- It has molecular weight of 69,000.
Albumin Functions:
- It helps in transport of anions, cations, dyes, drugs, hormones, enzymes, fatty acids, amino acids and bilirubin.
- It controls colloidal osmotic pressure.
- It regulates the pH balance in the blood.
- It provides the maximum viscosity to the blood to maintain blood pressure.
2. Globulin-38%:
- It has high molecular weight of about 1,30,000.
- It has various types like alpha, beta and gamma globulin,
Globulin Function:
- Globulin accelerates the tendency of rouleaux formation which is responsible for ESR.
- Globulin help in the suspension stability of blood.
- Transferrin-α2-ẞ globulin.
- Regulates and controls iron absorption from GIT.
- Haptoglobulin – α2 globulin.
- Prevents urinary loss of iron.
- Prevents kidney from damage caused by haemoglobin.
- Regulates renal threshold for haemoglobin.
- Ceruloplasmin – α2 – ẞ globulin.
- Binds with copper and helps in its transport and storage.
- Gamma globulin.
- Helps in defense mechanism of the body in the form of immunoglobulin.
- Transferrin-α2-ẞ globulin.
3. Fibrinogen -7%:
- It has molecular weight of 3,50,000
Fibrinogen Functions:
- It helps in coagulation of blood.
- The chemical nature of clot is fibrin, which is formed from fibrinogen.
- It increases rouleaux formation of RBC which helps to determine ESR.
- It helps in suspension stability of the RBC.
Question 17. Mention the functions of serum proteins.
Answer:
- Serum is plasma minus fibrinogen.
- Thus, serum proteins includes only albumin and globulin.
Serum proteins:
- Albumin: Refer previous question.
- Globulin: Refer previous question.
Question 18. Mention the methods for separation of plasma proteins.
Answer:
Separation of plasma proteins:
1. Precipitation method.
- It is used to separate albumin and globulin from serum.
- Serum is treated with 22% sodium sulphate solution.
- As a result, globulin gets precipitated and albumin remains in the solution.
2. Salting out methods.
- It is used to separate serum globulin into englobulin and pseudoglobulin.
- Englobulin is salted out by.
- Full saturation with sodium chloride solution.
- Half saturation with magnesium sulphate solution.
- One third saturation with ammonium sulphate solution.
- Pseudoglobulin is salted out by.
- Full saturation with magnesium sulphate solution.
- Half saturation with ammonium sulphate solution.
3. Electrophoretic method.
- This method is used to separate the plasma proteins depending on their electric charge and their rate of migration.
4. Cohn’s fractional precipitation method.
- This method separates the plasma proteins depending on their solubility.
5. Ultra centrifugation method.
- This method separates the plasma proteins depending on their density.
- Thus, it also determines molecular weight of these proteins.
Question 19. Describe the morphology of red blood cells.
Answer:
Morphology of red blood cells:
- Morphology of red blood cells Shape:
- It has disk-shaped and biconcave structure.
- This structure has following advantages.
- Helps in easy and quick exchanges of gases.
- Allows easy folding of RBC on itself when it passes through capillaries.
- Allows consideration alteration in cell volume to withstand considerable changes in pressure.
- Provides large surface area for absorption or removal of different substances.
- Morphology of red blood cells Size:
- Diameter -7.2 μ
- thickness-2.2 μ at periphery, 1 μ at center.
- Surface area – 120 sqm.
- Volume-85-90 cu.m.
- Morphology of red blood cells Structure:
- RBC is a non-nucleated cell.
- DNA and mitochondria are absent.
- Golgi apparatus is also absent.
- Energy is produced from glycolytic process.
- RBC contains cytoskeleton made up of actin and spectrin.
- Both these proteins are anchored to transmembrane protein by ankyrin.
- RBC cell membrane contains circular pores below which contractile protein spectrin lies.
- Spectrin maintains shape and flexibility of RBC and contains antigen.
- Morphology of red blood cells Count:
- At birth-6-7 million/μL
- Adult: Male – 5-6 million/μL, female – 4.5-5.5 million/μL.
- Life span 120 days after which it is destroyed by tissue macrhophage system.
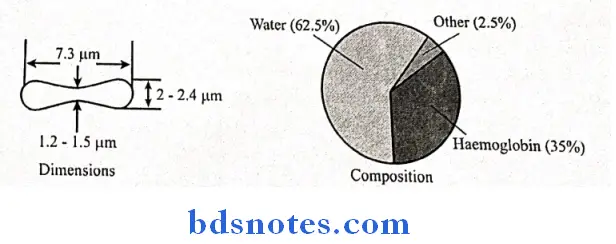
Morphology of red blood cells Composition:
- Water 62.5%
- Hemoglobin – 35%
- Organic substances – 2.5%
- This includes sugar, lipids, protein and enzymes.
Question 20. Mention the factors effecting erythropoeisis.
Answer:
1. Erythropoeisis General factors:
- Hypoxia:
- Inadequate supply of O2 to tissues causes stimulation of bone marrow to increase RBC production
- Nutrients:
- Carbohydrates required for energy supply.
- Fats required for cell membrane.
- Proteins – good quality of protein are required for the formation of haemoglobin.
- Minerals:
- Iron, manganese, copper, cobalt, nickel-help in ‘haem” formation.
- Vitamins:
- Vit. C-Help in synthesis of nucleic acid.
- Vit B, D and E are also required and its deficiency leads to anaemia.
- Hormones:
- Erythropoietin:
- It is most important general factor
- It stimulates RBC production.
- It is a glycoproteins.
- Hypoxia stimulates its production and is secreted in kidney.
- Actions:
- Promotes production of proerythroblasts from stem cells.
- Develops proerythroblast into matured RBCS
- Releases matured erythrocytes into blood.
- Increases ‘haem’ synthesis.
- Thyroxine:
- Required for maintaining metabolism and maturation
- Sex hormones:
- Androgens stimulates whereas oestrogens depress the formation and release of erythropoietin.
- It is most important general factor
2. Maturation factors:
- Vitamin B12:
- It is essential for maturation of erythrocytes and for synthesis of DNA.
- Intrinsic factor of castle:
- It is essential for the absorption of vitamin B12 from intestine into the blood.
- Folic acid:
- It is essential for maturation and for the synthesis of DNA.
- Its deficiency may lead to megaloblastic anaemia.
Question 21. Describe about abnormal haemoglobin.
Answer:
Abnormal haemoglobin:
- It is producted because of genetic mutation.
- This result is structural variations of polypeptide chains (α and β)

Question 22. Describe about abnormal haemoglobin derivatives.
Answer:
Abnormal haemoglobin derivaties:
- The abnormal haemoglobin derivaties in blood prevent the oxygen transport in tissues which results in severe hypoxia which may be fatal.

Question 23. Erythrocyte sedimentation rate.
Answer:
Erythrocyte sedimentation rate:
- It was first demonstrated by Edmund Biernacki in 1897.
Erythrocyte sedimentation rate Definition:
- The rate at which the erythrocytes gets settle down in a vertical tube is called erythrocyte sedimentation rate.
Erythrocyte sedimentation rate Determination:
1. By Westergren’s method:
- 1.6 ml of blood is mixed with 0.4ml of 3.8% sodium citrate.
- This is loaded is westergren’s tube which is kept vertically undisturbed for 1 hour.
- Reading is taken at the end of 1 hour.
2. By Wintrob’es method:
- About 1 ml of blood is mixed with EDTA O mark and kept undisturbed for 1 hour.
- Reading is taken after 1 hour.
Erythrocyte sedimentation rate Normal values:
- According to Westergren’s method:
- Males 3-7 mm in 1 hour
- Females59 mm in 1 hour
- Infants 0-2 mm in 1 hour.
Erythrocyte sedimentation rate Significance:
- ESR helps to confirm the diagnosis.
- It is helpful in assessing the patients response treated for certain chronic inflammatory disease.
Factors effecting ESR:
- Specific gravity of RBC.
- Rouleaux formation.
- Size of RBC
- Viscosity of blood.
- RBC count.
Question 24. Reticulocyte.
Answer:
Reticulocyte Synonym:
- Immature RBC.
- Size: 7-8 mm
Reticulocyte Structure:
- Nucleus is not present
- It contains remnants of RNA.
- Cytoplasm contains reticular network of disintegrated organelles.
- It is basophilic due to the presence of remnants of golgi apparatus, mitochondria and other organelles.
Reticulocyte Count:
- 2-6% in newobron.
- Decreases after first week.
- Remains constant at or below 1% – later.
- Increases when RBC production increases.
Question 25. Types of immunity.
Answer:
1. Innate immunity:
- It is inborn capacity of body to resist against diseases caused by pathogens.
- It is present at birth.
- Whenever any pathogens enters the body, it eliminates them before they cause any disease.
2. Acquired immunity:
- It is the resistance development by the body against any specific foreign body.
- It is also called specific immunity.
- Lymphocyte plays an important role in it.
- This is again of two types.
- Cellular immunity:
- It is responsible for delayed allergic reaction and rejection of transplants.
- It is mediated by T-lymphocytes.
- It is the major defence against infections caused by fungi, virus and bacteria.
- It also helps in defense against tumours.
- Humoral immunity:
- It is mediated by B-lymphocytes.
- It activates the complement system to neutralize antigens.
- It is major defense against bacterial infection
- Cellular immunity:
Question 26. Lymphocytes.
Answer:
Question 27. Platelets (or) Functions of platelets.
Answer:
Platelets are smallest, colourless, non-nucleated, spherical, oval or rounded granulated bodies.
platelets Size:
- 2.5 m in diameter.
- 7.5 cubic microns in volume.
platelets Structure:
- It is non-nucleated
- Cell membrane contains lipids, carbohydrates, proteins and glycoproteins.
- Microtubules form a ring around its cytoplasm.
- The cytoplasm includes golgi apparatus, endoplasmic reticulum, mitochondria, microtubule, microfilaments and granules.
- Cell membrane contains various receptors for combining with specific substances like collagen, fibrinogen and von-Willebrand’s factor.
platelets Normal count:
- 2,50,000/cu mm of blood (2,00,000 to 4,00,000).
platelets Life-span:
- 8-12 days after which it is destroyed is spleen.
platelets Properties: 3A’s
1. Adhesiveness:
- When a blood vessel is injured, platelets adhere to the exposed collagen present on the endothelium cell of the vessel wall.
2. Aggregration:
- It means grouping of platelets.
- The activated platelets become stick to each other.
- This stickiness is due to ADP and thromboxane A2.
3. Agglutination:
- It is the clumping of platelets.
- This property is due to platelet agglutinin and platelet activating factor.
Platelets Functions:
1. Role in hemostasis:
- Platelets prevents blood loss by.
- Secreting 5 HT- this causes the vasoconstriction.
- Platelets adhesiveness seal the damage blood vessels by forming temporary plugs.
- Platelets gets bind to the exposed collagen present on the endothelium of injured blood vessel.
2. Role in blood clotting:
- Platelet play a role in the formation of prothrombin activator of intrinsic pathway of blood coagulation.
3. Role in clot retraction:
- Within 5-30 min of fibrin clot formation, clot retracts to 40% of its original due to contractile proteins like actin, myosin, thrombosthenin in platelets.
4. Role in repair of rupture blood vessel:
- The cytoplasm of platelets contains platelet growth factor which helps in repair of blood vessel.
5. Role in defense mechanism:
- Platelets undergoes phagocytosis of carbon particles, viruses and immune complexes.
6. Storage and transport:
- Platelets stores 5-HT and histamine and release them when needed.
Question 28. Name two bleeding disease how are they caused?
Answer:
Bleeding disease:
1. Hemophilia:
- It is a sex linked inherited diseases characterized by prolonged clotting time.
Hemophilia Causes:
- Hemophilia occurs due to lack of formation of prothrombin activator.
- Causes differs according to its type.
Hemophilia A:
- It is caused due to deficiency of factor VIII of coagulation.
Hemophilia B:
- It is caused due to deficiency of factor IX of coagulation.
2. Purpura:
- It is a bleeding disorder characterized by prolonged bleeding.
- Types and Its causes:

3. Von villebrand Disease:
- It is a bleeding disorder characterized by excessive bleeding even after a mild injury.
Von villebrand Disease Causes:
- It occurs due to deficiency of von wilebrand factor.
- This suppresses platelet adhesion.
- It also causes deficiency of factor VIII.
Question 29. Hemostasis:
Answer:
Hemostasis Definition:
- Arrest of bleeding is called hemostasis.
Hemostasis Stages:
1. Vasoconstriction:
- It includes the constriction of blood vessels to decrease the blood flow and prevent its loss.
- When blood vessel is cut, collagen gets exposed from the damaged endothelium of the vessel.
- The platets adhere to this collagen and gets activated and secrete contractile substances to cause vasoconstriction.
- This adherence of platelets is facilitated by von Willebrand factor and platelet activating factor.
2. Formation of Platelet plug:
- The platelet that are adhere to the exposed collagen secrete ADP and thromboxane A2.
- These attract more and more platelets which aggregate to form and temporary loose platelet plug.
- This closes the vessel and prevents further blood loss.
3. Coagulation of blood:
- Fibrinogen gets converted into fibrin.
- This fibrin gets attached to the loosely formed platelet plug.
This is then modified by fibrin stabilizing factor and calcium ions to form a meshwork. - Thus, this is how blood loss in prevented after formation of blood clot.
Question 30. Describe intrinsic pathway of blood coagulation.
Answer:
Intrinsic mechanism of clotting:
Question 31. Give the normal percent of lymphocytes in differential leucocyte count. Explain the role of lymphocytes in immunity.
Answer:
Normal percent of lymphocytes in differential leucocyte count
- 20-30%
Functions of lymphocytes:

Question 32. In a tabular column indicate the agglutinogen and agglutinin in each of the blood groups of ABO & Rh system of blood grouping.
Answer:
ABO system:
- It is based on the presence and absence of antigen A and antigen B

Rh blood group:
- Rh factor is an antigen present in RBC
- It was first discovered by Landsteiner and Weiner in rhesus monkey
- The persons having D antigen are Rh positive
- Persons without D antigen are Rh negative
- Rh antibodies are of IgG type
Question 34. lassify and name the different leucocytes. Give two physiological variations in their number.
Answer:
Classification of WBC:

Question 35. Outline the origin, circulation and functions of lymph.
Answer:
Origin of lymph:
- Lymph is formed from interstitial fluid
Circulation:
Lymph node receives lymph by afferent vessels
- Afferent vessels divides into small channels
- Passing through afferent vessels and small channels lymph reaches the cortex
- Lymph then circulates through cortex, paracortex and medulla of the lymph node Finally lymph leaves the lymph node through efferent vessels.
Functions:
Lymph helps in transport of fluid from tissue spaces to blood
- It helps in removal of bacteria, toxins and other substances from various organs
- It helps in maintenance of structural and functional integrity of tissues
- It helps in defence due to formation of lymphocytes
- Transports absorbed long chain fatty acids and cholesterol from
the intestine via lymphatics into blood - Transports antibiotics
- Helps in the formation of maximally concentrated urine
- Supplies nutrition and oxygen to those parts where blood cannot reach
Question 36. Plasma.
Answer:
- It is a straw color clear liquid.
- It is the fluid portion of the blood.
- It represents 25% of the extracellular fluid.
- 55% of the total blood volume and about.
- 5% of body weight.
- Composition:
- Water-92-93%
- Solids 7-8%
- Plasma substances – 7%.
- Plasma proteins
- Amino acids
- Carbohydrate
- Fats
- Hormones and enzymes. Nonprotein nitrogenous substances Antibodies.
- Inorganic substances – 1%.
- \(\mathrm{Na}^{+}, \mathrm{Ca}^{2+}, \mathrm{K}^{+}, \mathrm{Mg}^{2+}, \mathrm{Cu}^{2+}, \mathrm{Fe}^{2+}\)
- \(\mathrm{HCO}_3^{-}, \mathrm{Cl}^{-}, \mathrm{PO}_4^{3-}, \mathrm{I}^{-} .\)
- Plasma substances – 7%.
- Gases.
- Oxygen
- Carbon dioxide
- Nitrogen.
Question 37. Plasma proteins.
Answer:
1. Albumin:
- It forms the major bulk of plasma proteins 55%.
- It, has molecular weight of 69,000.
- It helps in transport of essential substances.
- It regulates osmotic pressure, pH balance.
- It provides the maximum viscosity to the blood.
2. Globulin-38%:
- It has molecular weight of about 1,30,000.
- It accelerates the rouleaux formation and hels in suspension stability of blood.
Types:
- Alpha, beta and gamma globulin.
3. Fibrinogen -7%:
- It has molecular weight of 3,50,000.
- It is mainly involved in the coagulation of blood.
Question 38. Four functions of plasma proteins.
Answer:
Functions of plasma proteins:
1. Coagulation:
- Fibrinogen, prothrombin and haemophilic globulin are involved in coagulation.
2. Immunity:
- The gamma globulin produce antibodies which provide immunity to the body.
3. Transport:
- Plasma proteins helps in transport of certain substances like hormones, enzymes etc.
4. Erythrocyte sedimentation Rate (ESR):
- Globulin and fibrinogen accelerate rouleaux formation which is responsible for ESR.
5. Reserve Function:
- Plasma proteins stores proteins and break them into amino acids when needed by the body.
Question 39. Serum.
Answer:
If blood is allowed to clot in a test tube, then the clot retracts and gives out serum.
- On formation of clot, fibrinogen is utilized.
- Thus, serum contains only albumin and globulin and not fibrinogen.
- It has higher serotonin 5HT content as due to clotting platelets have been breakdown.
Question 40. Starling’s Hypothesis.
Answer:
- It is to determine the net filtration pressure.
- According to the Starling’s hypothesis, the net filtration through capillary membrane is proportional to the hydrostatic pressure difference across the membrane minus the oncotic pressure differences.
- These pressure are called Starlings forces.
Question 41. Properties of red blood cells.
Answer:
1. Rouleaux formation:
- On collection of blood, the RBCs pile up one above another.
- This is called rouleaux formation.
- This helps in determination of ESR.
2. Specific gravity:
- The specific gravity of RBC is 1.092 to 1.101.
3. Packed cell volume:
- When the blood is centrifuged with a proper anticoagulant, the RBCs settle at the proper anticoagulant, the RBCs settle at the bottom of the tube.
- This is called packed cell volume.
4. Suspension stability:
- During circulation, the RBCs remain uniformly suspended in the blood.
Question 42. Functions of RBC.
Answer:
1. Transport of oxygen from the lungs to the tissues.
- Oxygen combines with haemoglobin in RBC and is transported in blood.
2. Transport carbon dioxide from the tissues to the lungs.
- RBCs contains carbonic anhydrase which forms bicarbonate from water and carbon dioxide.
- Thus it helps to transport of carbon dioxide in the form of bicarbonate.
3. Buffering action.
- Hemoglobin in RBC regulates hydrogen ion concentration and hence maintains the pH balance of blood.
4. In determination of blood groups.
- RBC contains antigens which determine blood group.
Question 43. Fate of Red Blood Cells.
Answer:
Life span of red blood cells in 120 days.
- After 120 days, their cell membrane becomes more fragile.
- Because of this fragility they fail to pass through the capillaries whose diameter is less or equal to that of RBC.
- Even if they try to squeeze out through these capillaries, they are destroyed.
- This destruction mainly occurs in spleen.
- This destroyed RBC is fragmented and haemoglobin is released.
- This haemoglobin is degraded into.
- Iron – combines with apoferritin, form ferritin and is stored in the body.
- Globin enters protein depot.
- Porphyrin- degrade to form bilirubin which is excreted by liver.
Question 44. Functions of haemoglobin.
Answer:
1. Transport oxygen from lungs to tissues.
2. Transport carbon dioxide from tissues to lungs.
3. Buffer action.
Question 45. State difference between foetal haemoglobin and adult haemoglobin.
Answer:

Question 46. Iron.
Answer:
It helps in the formation of heme portion of haemoglobin.
- It helps in the formation of.
- Hemoblobin.
- Myoblogin.
- Enzymes.
Normal value:
- The total quantity of iron in the body is about 4 grams.
Absorption:
- Iron is absorbed from the small intestine and transported into the plasma.
Storage:
- Iron is stored in the reticuloendothelial cells and liver hepatocytes.
Daily loss of iron:
- In males – 1 mg of iron excreted every day.
- In famales- very high due to menstruation.
Question 47. Iron deficiency anaemia.
Answer:
Definition:
- Any anaemia which responds to adequate dosage of iron is called iron deficiency anaemia.
Causes:
- Loss of blood
- Decreased intake of iron.
- Increased demand of iron in conditions like growth and pregnancy.
- Poor absorption of iron from intestine.
Features:
- Brittle nails, spoon shaped nails.
- Brittle hair.
- Atrophy of papilla in tongue.
- Dysphagia.
- Early breathlessness.
- Headache, irritability.
- Generalized body ache.
Investigation:
- Microcytic, hypochromic RBC.
- Normoblastic, hyperplastic bone marrow.
- Normal WBC and platelet count.
- Serum billirubin < 0.4 mgl dl.
- Serum iron decreases.
- Total iron binding capacity increases.
Question 48. Pernicious anaemia.
Answer:
Synonym:
- Addison’s anaemia.
Cause:
- Lack of intrinsic factor which helps in absorption of Vit. B12.
Features:
- Generalised weakness.
- Loss of appetite, diarrhoea.
- Soreness and inflammation of tongue.
- Numbness/tingling of extremities.
- Pale yellowish discoloration of skin.
- Progressive ataxia.
- Subacute combined degeneration of spinal cord.
Investigations:
- RBCs macrocyotic and hypochromic.
- RBC count decrease.
- Hb- decreases < 12 gm/dl.
- Reticulocyte count increases.
- WBC and platelets decreases
- Atrophy of gastric mucosa.
Question 49. Megaloblastic anaemia.
Answer:
Definition:
- An anaemia that occurs due to deficiency of folic acid is called megaloblastic anaemia.
Causes:
- Less dietary intake.
- Poor absorption from GIT.
- Increased demand.
- Antifolate drugs.
Features:
- Soreness of tongue.
- Generalized weakness
- Loss of apatite
- Diarrhoea.
- Pale yellow skin.
Investigations:
- Defective DNA synthesis.
- RBCs – megaloblastic and hypochromic.
- RBCs are immature.
Question 50. Aplastic anaemia.
Answer:
- It occurs due to total suppression of bone marrow. The bone marrow is replaced by fatty tissues.
- It occurs in conditions like.
- Repeated radiation exposure.
- Presence of bacterial toxins.
- Excessive use of certain drugs like sulphur drugs.
- Malignancy of bone marrow.
- RBCs in this are normocytic and normochromic.
Question 51. Anaemia.
Answer:
Definition:
- Anaemia is a clinical condition characterized by reduction in the number of RBCs less than 4 million/μL or their content of haemoglobin less than 12 gm/dL or both.
Classification:
1. Etiological classification:
- Hemorrhagic – due to blood loss.
- Hemolytic – due to excessive destruction of RBCs
- Nutritional deficiency – due to deficiency of iron, vitamins and protein, etc.
- Aplastic anaemia – due to suppression of bone marrow.
- Anaemia of chronic diseases.
2. Morphological classification:
- It is based on the size of RBC and its haemoglobin concentration
-
- Normocytic normochromic anaemia.
- Size of RBC – normal.
- Haemoglobin content – normal.
- RBC count decreases.
- Macrocytic normochromic anaemia.
- Size of RBC – increases.
- Haemoglobinc content – normal
- RBC count – decreases.
- Macrocytic Hypochromic anaemia.
- Size of RBC – increases.
- Haemoglobin content – decreases. RBC count – less.
- Microcytic hypochromic anaemia.
- Size of RBC – decreases.
- Haemoglobin content – decreases.
- Normocytic normochromic anaemia.
Features:
- Pallor skin
- Breathlessness, tachycardia.
- GIT disturbances.
- Nail changes
- Increased basal metabolic rate.
- Disturbed menstrual cycle.
- Easy fatigue.
Question 52. Packed cell volume (PCV).
Answer:
Definition:
- It is the volume of RBCs packed at the bottom of a haemotocrit tube when the blood is centrifuged.
- It is expressed as the percentage of cellular elements with that of whole blood.
Significance:
- PCV helps in.
- Diagnosis and treatment of anaemia and polycythemia.
- Determine the extent of dehydration.
- Determine the need for blood transfusion.
Normal values:
- In males – 40-45%.
- In females – 38-42%.
Question 53. Define Hemolysis and fragility. (or) Himophilia. (or) Purpura.
Answer:
Hemolysis:
- It is the process which involves the breakdown of RBC and liberation of haemoglobin.
Fragility:
- The susceptibility of RBC to hemolysis or tendency to break easily is called fragility.
- It has two types.
- Osmotic fragility due to exposure to hypotonic saline.
- Mechanical fragility – due to mechanical trauma.
Question 54. Leukocytes.
Answer:
- They are the colourless and nucleated formed elements of blood.
- They are large than RBC
Classification:
1. Granulocytes:
- Neutrophils.
- Eosinophils.
- Basophils.
2. Agronulocytes:
- Monocytes.
- Lymphocytes.
Normal count:
- At birth -20,000/mL.
- In adults – 4,000-11,000/mL
Life-span:
- It is varies from half a day to 3-6 months.
Properties:
1. Diapedesis – squeezing of WBC through blood vessels.
2. Ameboid movement.
- WBC change their shape by protruding into the cytoplasm.
3. Chemotaxis.
- Attracted by the chemical substances present in the tissues.
4. Phagocytosis.
- Engulf foreign body and destroy them.
Functions:
- They play an important role in defence mechanism.
Question 55. Neutrophils.
Answer:
It constitute 50-70% of the total leucocyte count.
- Size: 10-14 μ in diameter.
- Structure:
- Nucleus is multilobed.
- Cytoplasm is granular, slight bluish in colour
- Granules are fine,
- pin-point.
Functions:
- Phagocytosis.
- Contains fever producing substances, endogenous pyrogen.
- Variations: causes.

Question 56. Lymphocytes.
Answer:
- It constitutes 20-30% of the total leucocyte count.
Structure:
- Nucleus – oval, large and kidney shaped.
- Nuclear chromatin is coarse and shapeless.
- Cytoplasm is scanty, pale blue and agranular.
Types:
1. Depending on the size.
- Large lymphocytes – 10-12 μ in diameter.
- Small lymphocyte – 7-10 m in diameter.
2. Depending on function.
- T lymphocytes – provide cellular immunity.
- B lymphocytes – provide humoral immunity.
Life-span:
Functions:
- They are responsible for defence mechanism by providing immunity to the body.
Question 57. Autoimmune diseases.
Answer:
Definition:
- It is the diseases produced when body’s normal tolerance decreases and the immune system fails to recognize the body’s own tissues as “self” and attacks them.
Types:
1. Organ specific disease – affects only one organ.
2. Organ nonspecific disease – affects many organs.
Cause:
- Deficiency of suppressor – T-cell.

Question 58. Platelets.
Answer:
- They are small, colourless, non-nucleated spherical, oval or rounded granular bodies.
- Size: 2.5 m in diameter.
- Normal count:
- 2,50,000 (2,00,000 to 4,00,000)/cu mm of blood.
- Properties: 3A’s
- Adhesiveness
- Aggregation Agglutination
Functions:
- Prevents blood looss
- Helps in blood coagulation by forming prothrombin activator.
- Helps in clot retraction as it contains contractile proteins.
- Contribute in repair of ruptured blood vessel.
- Stores 5-HT and histamine and release when needed.
- Life-span: 10 days.
Question 59. Prothrombin time.
Answer:
Definition:
- The time taken by blood to clot after adding tissue thromboplastin is called prothrombin times.
- It indicates the total quantity of prothrombin present in the blood.
Normal time-12 seconds:
Prolonged in:
- Deficiency of prothrombin.
- Deficiency of clotting factors I, V, VII and X
Question 60. Pro-coagulants.
Answer:
- They are hemostatic agents which accelerate the process of blood coagulation.
- They are:

Question 61. Anticoagulants.
Answer:

Question 62. Hazards of mismatched blood transfusion.
Answer:
- Agglutination.
- Haemolysis.
- Fever and chills.
- Jaundice
- Renal failure.
- Uraemia.
- Coma and death.
Question 63. Causes of hypervolemia and hypovolemia.
Answer:
Causes of Hypervolemia – 2H, 2C.
- Hyperthyroidism.
- Hyperaldosteronism.
- Cirrhosis of liver.
- Congestive cardiac failure.
Causes of Hypovolemia.
- Blood loss
- Fluid loss
- Hemolysis.
- Anaemia
- Obesity
- Hypothryoidism.
Question 64. Physiology of clotting.
Answer:
- Coagulation is the process in which blood losses its fluidity and becomes a jelly like mass few minutes after it is shed out or collected in a container.
- In clotting the following steps are involved.
1. Prothrombin activator is formed by
- Extrinsic pathway-by tissue thromboplastin.
- Intrinsic pathway – by platelets.
2. Next prothrombin is converted into thrombin by prothrombin activator in the presence of calcium.
3. This thrombin converts fibrinogen into activated fibrinogen called fibrin monomer.
- This monomer gets polymerize and form loose strands of fibrin.
- These loose strands are modified into dense and tight strands by fibrin stabilizing factor.
- All strands aggregate and form a meshwork.
- Red cells and serum are trapped in this meshwork
- The red colour of clot is due to these trapped red cells.
Question 65. Test for bleeding disorders.
Answer:
1. Bleeding time:
- It is the time interval from oozing of blood after a cut or injury till arrest of bleeding.
- Normal duration: 3-6 min.
- Prolonged in: Purpura.
2. Clotting time:
- It is the time interval from oozing of blood after a cut or injury till the formation of clot.
- Normal duration: 3-8 min.
- Prolonged in: Hemophilia.
3. Prothrombin time:
- The time taken by blood to clot after adding tissue thromboplastin is called prothrombin time.
- Normal duration: 12 sec.
- Prolonged in: Deficiency of prothrombin and clotting factors I, V, VII, X
Question 66. Why blood does not clot in circulation?
Answer:
Normally, blood does not clot in the blood vessel because of the following reasons.
- Presence of inactive form of all clotting factors.
- Continuous movement of blood.
- Smooth endothelial lining of the blood vessel.
- Presence of negatively charged particles over endothelial lining which repel anions of clotting factors.
- Presence of natural anticoagulant like heparin in blood.
- Simultaneous activation of fibrinolytic system alongwith clotting mechanism.
Question 67. Erythroblastosis fetalis.
Answer:
It is a Rh incompatibility reaction in newborn.
- When Rh negative mother carries Rh positive foetus for the first time, the mother’s plasma is sentizied and the first child is usually normal.
- But at the time of delivery Rh antigen from fetal blood leaks into mother blood and mother develops Rh antibody against it.
- In later pregnancies, this Rh antibody crosses the placental barrier and enters the fetal blood.
- This Rh antibody now causes destruction of fetal RBC.
- Severe destruction of RBC causes jaundice.
- To compensate this destruction, more and more RBC are formed.
- As a result, excessive immature erythrocytes are released in circulation.
- Thus, this condition is called erythroblastis fetalis.
Prevention:
- Mother should be immunized with anti-Rh antibodies after 1st delivery within 48 hours.
Treatment:
- The baby is treated with exchange transfusion which replaces infant’s own Rh positive blood into Rh negative blood.
Question 68. Functions of spleen.
Answer:
1. Formation:
- Spleen forms RBC in 2nd trimester of uterine life and after destruction of red bone marrow in adults.
- Spleen contains lymphoid tissues, which forms lymphocytes and plasma cells.
2. Destruction:
- Spleen destroys aged RBCs, WBCs and platelets.
3. Defense:
- Spleen phagocytose the micro-organisms and other foreign bodies.
- It forms antibodies due to the presence of T and B lymphocytes in it.
4. Reservoir:
- Spleen stores large number of RBCs which is released in emergency conditions.
Question 69. Spleenomegaly:
Answer:
Enlargement of spleen is called spleenomegaly.
Causes:
- Infectious diseases
- Inflammatory diseases
- Haematological disorders.
- Liver diseases
- Pernicious anaemia.
- Cysts in spleen.
- Hodgkin’s disease
- Glandular fever.
Effects:
- Hemolysis.
- Anaemia – low RBC count
- Leukopenia – low WBC count
- Thrombocytopenia – low platelet count.
- Increase in plasma volume as the volume of formed elements decreases.
Question 70. Properties of blood.
Answer:
1. Color:
- Blood is red in color.
- Arterial blood-scarlet red due to more oxygen.
- Venous blood-purple red due to more carbon dioxide.
2. Volume:
- Average volume – 5 litres
- In newborn – 450 ml.
- In females 4.5 litres
3. pH:
- Blood is alkaline with pH-7.4.
4. Specific gravity:
- Total blood -1.052 -1.061
- Blood cells – 10.92-1.101
- Plasma-1.022 -1.026
5. Viscocity:
- Blood is 5 times more viscous than water.
Question 71. Significances of body fluids.
Answer:
1. In hemostasis:
- Water not only form internal environment but also play a role in hemostasis.
2. Transport:
- Water transports essential nutrients to the cells and removes unwanted substances.
3. Metabolic reaction:
- Water acts as a medium for many necessary metabolic reactions.
4. In texture of tissue:
- Presence of water in tissue maintains its form and texture.
5. Temperature regulation:
- Water maintain normal body temperature.
Question 72. Thrombosis.
Answer:
Thrombosis Definition:
Thrombosis Complication:
- Formation of thrombus.
- Embolism.
- Infraction.
Question 73. Landsteiner’s law
Answer:
Landsteiner’s law states that
- If particular antigen is present in the RBCs, corresponding antibody must be absent in the serum
- If particular antigen is absent in the RBCs, corresponding antibody must be present in the serum
Question 74. Agranulocytes
Answer:
- Agranulocytes are leucocytes without granules
- They are
- Monocytes
- Lymphocytes

Question 75. List two features of RBC in iron deficiency anaemia.
Answer:
RBC features in Iron deficiency anaemia
- Microcytic, hypochromic
- Count decreases or normal
- Life span is normal
- Peripheral smear shows anisocytosis and poikilocytosis
Question 76. Give examples of positive and negative feedback mechanism.
Answer:
Positive feedback mechanism:
- It is one in which the system reacts in such a way as to increase the intensity of change in same direction
- Example: Blood clotting mechanism, milk ejection reflex
Negative feedback mechanism:
- It is one in which the system reacts in such a way as to stop the change or reverse the direction of change
- Example: TSH released from pituitary gland stimulates thyroid gland to release thyroxin
- When thyroxin level increases, it inhibits the secretion of TSH from pituitary gland
Question 78. Classify anaemia. Give example for each.
Answer:

Question 79. Functions of blood
Answer:
- Nutritive
- Blood carries the food absorbed from the digestive system to tissues for growth and production of energy
- Respiratory
- Blood transport oxygen from lungs to the tissues and carbon dioxide from the tissues to the lungs
- Excretory
- Waste products are carried through blood to excretory organs like kidney, skin and intestine
- Transport of hormones and enzymes
- Blood transports the hormones secreted from the endocrine glands to their target organs/ tissues
- Blood also transports enzymes
- Regulation of water balance
- Water balance is regulated as the water content of the blood gets interchangable with interstitial fluid
- Regulation of acid base balance
- Blood maintains pH through the buffering system of plasma proteins and haemoglobin
- This mechanism is called homeostasis
- Regulation of body temperature
- Blood regulates body temperature due to its high specific heat
- It regulates through thermoregulatory mechanism due to which balance occurs between heat loss and heat gain in the body
- Storage function
- Blood stores substances like proteins, glucose, sodium and potassium so that these substances can be used during starvation, fluid loss, etc
- Defensive function
- White blood cells help in the defence of the body
Question 80. Functions of lymph
Answer:
- Lymph helps in transport of fluid from tissue spaces to blood
- It helps in removal of bacteria, toxins and other substances from various organs
- It helps in maintenance of structural and functional integrity of tissues
- It helps in defence due to formation of lymphocytes
- Transports absorbed long chain fatty acids and cholesterol from the intestine via lymphatics into blood Transports antibiotics
- Helps in the formation of maximally concentrated urine
- Supplies nutrition and oxygen to those parts where blood cannot reach
Question 81. State the various stages in the development of red blood corpuscles.
Answer:
Stages in the development of red blood corpuscles:
- Pro erythroblast
- Early normoblast
- Intermediate normoblast
- Late normoblast
- Reticulocyte
- Matured erythrocyte
Question 82. What is the normal value of PCV, MCH.
Answer:
Normal values:
- Packed Cell Volume, PCV
- In males-40-45%
- In females-38-42%
- Mean corpuscles haemoglobin (MCH) – 30 pg
Question 83. What is cross matching? What are the types?
Answer:
Cross-matching refers to the test that is performed prior to a blood transfusion in order to determine if the donor’s blood is compatible with the blood of an intended recipient.
Cross-matching is also used to determine compatibility between a donor and recipient in organ transplantation.
Cross-matching Types:
1.
- Immediate-spin cross-matching (ISCM):
- Immediate-spin cross-matching is an abbreviated form of cross-matching that is faster, less expensive but also less sensitive.
- It is an immediate test that combines the patient’s serum and donor’s red blood cells at room temperature.
- No agglutination indicates a negative test reaction, or compatible match.
- Electronic cross-matching:
- Electronic cross-matching is a computer-assisted analysis using data, from the donor unit and testing done on blood samples from the intended recipient.
- This includes ABO/Rh typing of the unit and of the recipient, and an antibody screen of the recipient.
2.
- Major cross-match:
- Recipient serum is tested against donor packed cells to determine if the recipient has preformed antibodies against any antigens on the donor’s cells
- Minor cross-match:
- Recipient red cells are tested against donor serum to detect donor antibodies directed against a patient’s antigens.

Leave a Reply