Coagulants And Anticoagulants
A theory of blood clotting introduced in 1905 was based on the existence of four factors: thromboplastin (thrombokinase), prothrombin, fibrinogen, and ionized calcium.
- The clotting sequence proposed was that when tissue damage occurred, thromboplastin entered the blood from the platelets and reacted with prothrombin in the presence of calcium to form thrombin.
- Thrombin then reacted with fibrinogen to form insoluble fibrin, which enmeshed red blood cells (RBCs) to create a clot.
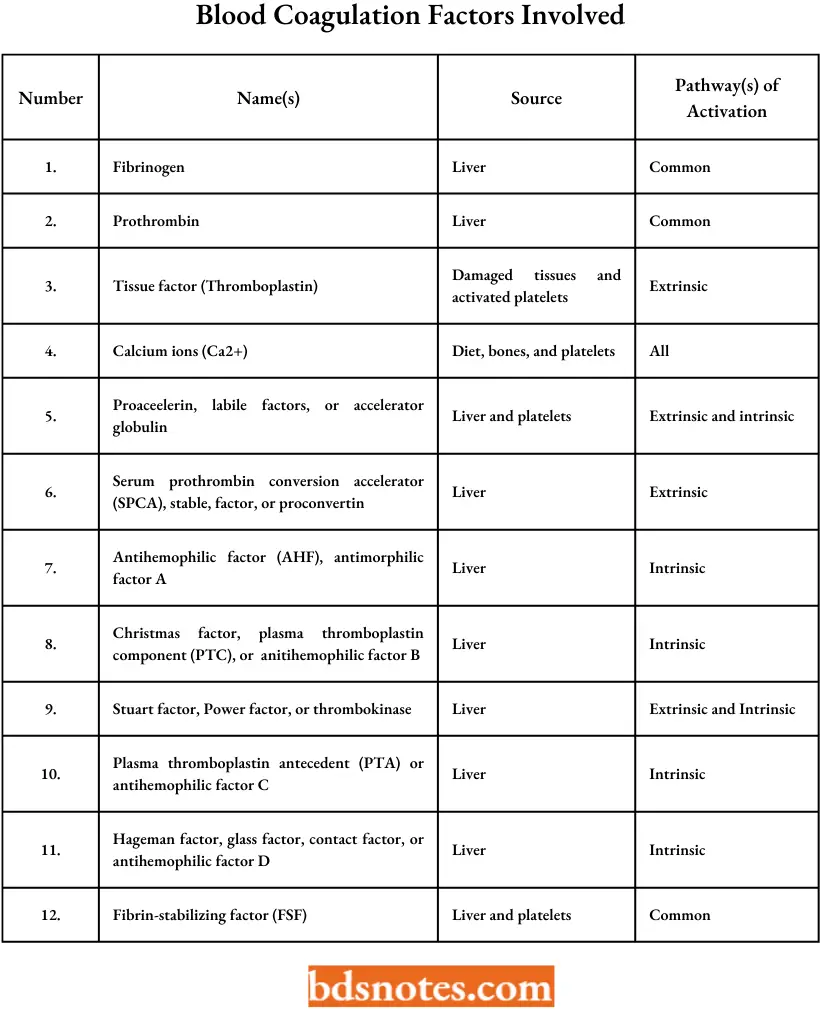
Blood coagulation: factors involved
Mechanism Of Blood Coagulation
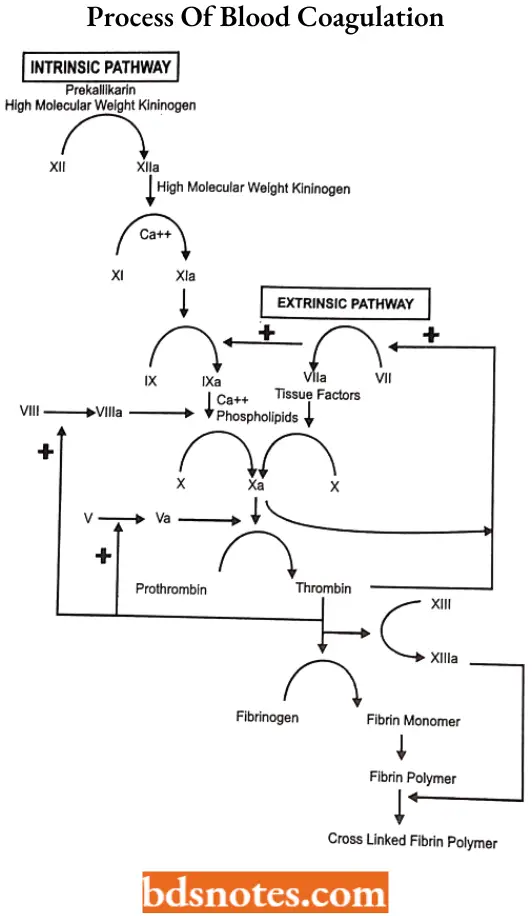
The process of blood coagulation involves a series of steps that occur in a cascade and terminate in the formation of a fibrin clot.
- Blood coagulation occurs by activation of either an intrinsic pathway, a relatively slow process of clot formation, or an extrinsic pathway, which has a much faster rate of fibrin formation.
- Both pathways merge into a common pathway for the conversion of prothrombin to thrombin and the subsequent transformation of fibrinogen to the insoluble strands of fibrin.
- Lysis of intravascular clots occurs through a plasminogen plasmin system, which consists of plasminogen, plasmin, urokinase, kallikrein, plasminogen activators, and some undefined inhibitors.
- The intrinsic pathway refers to the system for coagulation that occurs from the interaction of factors circulating in the blood. It is activated when blood comes into contact with a damaged vessel wall or a foreign substance.
- Each of the plasma coagulation factors, except factor 3 (tissue thromboplastin), circulates as an inactive proenzyme.
Read and Learn More Medicinal Chemistry II Notes
Except for fibrinogen, which precipitates as fibrin, these factors are usually activated by enzymatic removal of a small peptide in the cascade of reactions that make up the clotting sequence.
- The extrinsic clotting system refers to the mechanism by which thrombin is generated in plasma after the addition of tissue extracts.
- When various tissues, such as the brain or lungs (containing thromboplastin), are added to blood, a complex between thromboplastin and factor 7 in the presence of calcium ions activates factor 10, bypassing the time-consuming steps of the intrinsic pathway that form factor 10.
- The intrinsic and extrinsic pathways interact in vivo. Small amounts of thrombin formed early after stimulation of the extrinsic pathway accelerate clotting by the intrinsic pathway by activating factor 8.
- Thrombin also speeds up the clotting rate by activating factor V, located in the common pathway. Thrombin then converts the soluble protein fibrinogen into a soluble fibrin gel by acting on GlyArg bonds to remove small fibrinopeptides from the N-terminus, enabling the remaining fibrinogen molecule to polymerize.
It also activates factor XHI, which stabilizes the fibrin gel in the presence of calcium by cross-linking between the chains of the fibrin monomer through intermolecular y-glutamyl- lysine
Coagulant drugs: Coagulant drugs, also called anti-inhibitor coagulant complexes, also help regulate blood coagulation. Some diseases, such as hemophilia, lead to defects in blood bleed uncontrollably in response to coagulation and patients suffering from the disorder can have relatively minor injuries.
Anticoagulant drugs: Although anticoagulants are called blood thinners, these medicines do not thin your blood. Instead, they decrease the blood’s ability to clot. Decreased clotting keeps fewer harmful blood clots from forming and from blocking blood vessels.
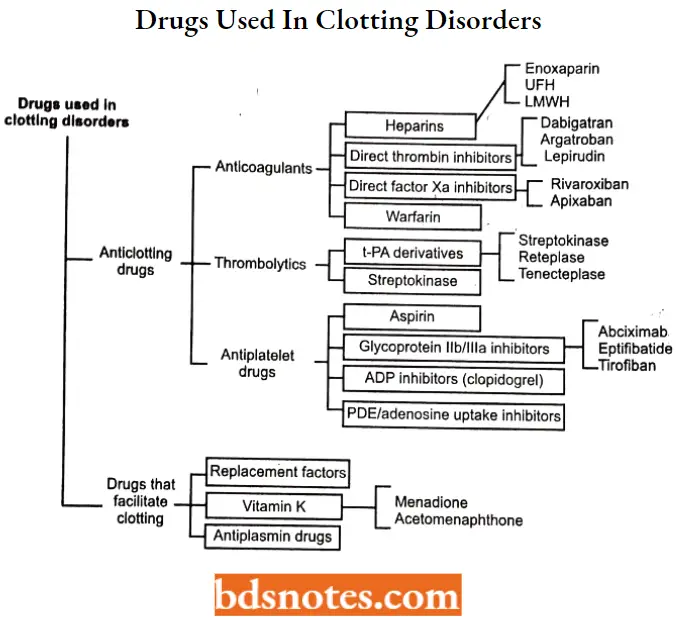
Classification Of Drugs Used In Clotting Disorders
Menadione
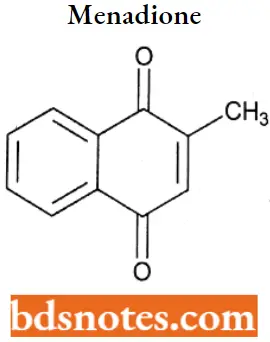
Menadione IUPAC name: 2-methyl-1,4-dihydronaphthalene-l,4-dione.
Menadione MOA: Menadione (vitamin K3) is involved as a cofactor in the posttranslational gamma-carboxylation of glutamic acid residues of certain proteins in the body.
- These proteins include the vitamin K-dependent coagulation factors 2 (prothrombin), 7 (proconvertin), 9 (Christmas factor), 10 (Stuart factor), protein C, protein S, protein Zv, and a growth-arrest-specific factor (Gas6).
- In contrast to the other vitamin K-dependent proteins in the blood coagulation cascade, protein C and protein S serve anticoagulant roles. The two vitamin K-dependent proteins found in bone are osteocalcin, also known as bone Gla (gamma-carboxyglutamate) protein or BGP, and the matrix Gla protein or MGP.
- Gamma-carboxylation is catalyzed by the vitamin K-dependent gamma-carboxylases. The reduced form of vitamin K, vitamin K hydroquinone, is the actual cofactor for the gamma carboxylases
Menadione Uses: The primary known function of vitamin K is to assist in the normal clotting of blood, but it may also play a role in normal bone calcification.
Menadione Adverse effect: Menadione (vitamin K3), which is not used as a nutritional supplemental form of vitamin K for humans, has been reported to cause adverse reactions, including hemolytic anemia. Large doses have also been reported to cause brain damage.
Acetomenaphthone
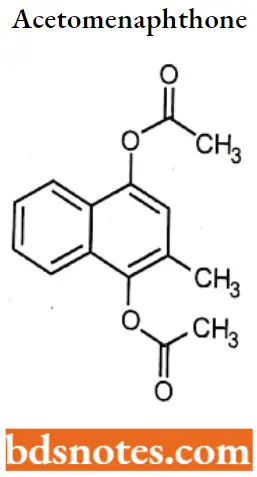
Acetomenaphthone IUPAC name: (4-acetyloxy-3-methylnaphthalen-1-yl) acetate.
Acetomenaphthone MOA: Acetomenaphthone (Vitamin K3) is a synthetic analogue, involved as a cofactor in the posttranslational gamma-carboxylation of glutamic acid residues of certain proteins in the body.
- These proteins include the vitamin K-dependent coagulation factors 2 (Prothrombin), 7 (proconvertin), 9 (Christmas factor), 10 (Stuart factor), protein C, Protein S, protein Zv, and a growth-arrest-specific factor (Gas6).
- In contrast to the other vitamin K-dependent proteins in the blood coagulation cascade, protein C and protein S serve anticoagulation roles. The two vitamin K-dependent proteins found in bone are osteocalcin, also known as bone G1a (gamma-carboxyglutamate) protein or BGP, and the matrix G1a protein or MGP.
- gamma-carboxylation is catalyzed by the vitamin K-dependent gamma-carboxylases. The reduced form of vitamin K, vitamin K hydroquinone, is the actual cofactor for the gamma-carboxylases.
Warfarin
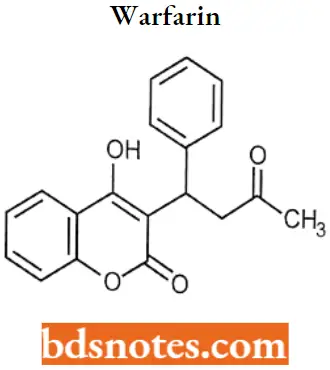
Warfarin IUPAC name: 4-hydroxy-3-(3-oxo-1-phenylbutyl)-2H-chromen-2-one.
Warfarin MOA: Warfarin inhibits vitamin K reductase, resulting in depletion of the reduced form of vitamin K (vitamin KH2).
- As vitamin K is a cofactor for the carboxylation of glutamate residues on the N-terminal regions of vitamin K-dependent proteins, this limits the gamma-carboxylation and subsequent activation of the vitamin K-dependent coagulant proteins.
- The synthesis of vitamin K-dependent coagulation factors 2, 7, 9, and X and anticoagulant proteins C and S is inhibited.
- Depression of three of the four vitamin K-dependent coagulation factors (factors 2, 7, and 10) results in decreased prothrombin levels and a decrease in the amount of thrombin generated and bound to fibrin. This reduces the thrombogenicity of clots.
Warfarin Metabolism: Hepatic CYP2C9 isozyme is responsible for metabolizing (S)-warfarin and other coumarin derivatives to give 6- and 7-hydroxywarfarins as the major inactive metabolites.
- Whereas hepatic CYP3A4, CYP1A2, and CYP2C19 isozymes inactivate (R)-warfarin, the less active enantiomer, to give 4′-, 6-, and 8-hydroxywarfarins, respectively.
- Warfarin also undergoes, to a lesser extent, reductive metabolism of the ketone on the C-3 side chain to a pair of pharmacologically active, diastereomeric 2′-hydroxywarfarins.
Warfarin Uses: For the treatment of retinal vascular occlusion, pulmonary embolism, cardiomyopathy, atrial fibrillation and flutter, cerebral embolism, transient cerebral ischemia, arterial embolism and thrombosis.
The clinically used preparation of warfarin is racemic, but the (S)- and (R)-enantiomers are not equipotent. (S)-warfarin is at least fourfold more potent as an anticoagulant than (R)-warfarin.
Warfarin Adverse Effect: Warfarin can cross the placental barrier during pregnancy which can result in fetal bleeding, spontaneous abortion, preterm birth, stillbirth, and neonatal death.
Additional adverse effects such as necrosis, purple toe syndrome, osteoporosis, valve and artery calcification, and drug interactions have also been documented with warfarin use.
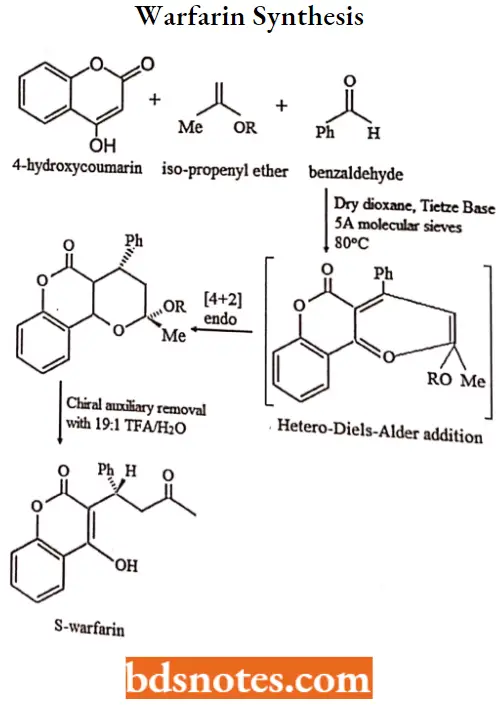
Warfarin Synthesis:
Anisindione
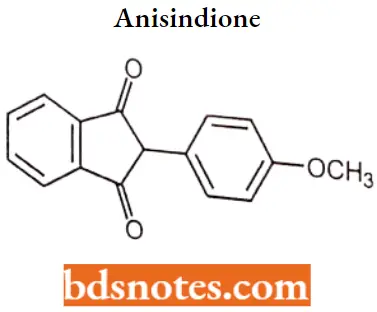
Anisindione IUPAC name: 2-(4-methoxyphenyl)-2/3-dihydro-1H-indene-1/3-dione.
Anisindione MOA: Anisindione exercises its therapeutic action by reducing the prothrombin activity of the blood.
- Anisindione prevents the formation of active pro-coagulation factors 2, 7, 9, and 10, as well as the anticoagulant proteins C and S, in the liver by inhibiting the vitamin K-mediated gamma-carboxylation of precursor proteins.
- Anisindione has no direct thrombolytic effect and does not reverse ischemic tissue damage, although it may limit the extension of existing thrombi and prevent secondary thromboembolic complications.
Anisindione Uses: For the prophylaxis and treatment of venous thrombosis and its extension, the treatment of atrial fibrillation with embolization, the prophylaxis and treatment of pulmonary embolism, and as an adjunct in the treatment of coronary occlusion.
Anisindione Adverse Effect: An overdose is likely to cause abnormal bleeding, for which the symptoms include: bleeding from gums or nose, blood in urine or stools, excessive bleeding from minor cuts, and patches of discoloration or bruises on the skin.
Clopidogrel
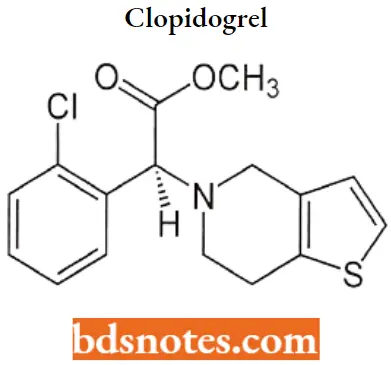
Clopidogrel IUPAC name: methyl (2S)-2-(2-chlorophenyl)-2-{4H,5H,6H,7H-thieno[3,2-c]pyridin-5-yl}acetate.
Clopidogrel MOA: The active metabolite of clopidogrel prevents binding of adenosine diphosphate (ADP) to its platelet receptor, impairing the ADP-mediated activation of the glycoprotein GP 2b/3a complex.
- It is proposed that the inhibition involves a defect in the mobilization from the storage sites of the platelet granules to the outer membrane.
- The drug specifically and irreversibly inhibits the P2Y12 subtype of ADP receptor, which is important in the aggregation of platelets and cross-linking by the protein fibrin.
- No direct interference occurs with the GP 2b/3a receptor. As the glycoprotein GP 2b/3a complex is the major receptor for fibrinogen, its impaired activation prevents fibrinogen binding to platelets and inhibits platelet aggregation.
- By blocking the amplification of platelet activation by released ADP, platelet aggregation induced by agonists other than ADP is also inhibited by the active metabolite of clopidogrel.
Clopidogrel Metabolism: Hepatic, extensive, and rapid, by hydrolysis to the main circulating metabolite, a carboxylic acid derivative, which accounts for approximately 85% of the circulating drug-related compounds.
A glucuronic acid derivative of the carboxylic acid derivative has also been found in plasma and urine. Neither the parent compound nor the carboxylic acid derivative has a platelet-inhibiting effect. The active metabolite of clopidogrel is 2- oxoclopidogrel.
Clopidogrel Uses: For the reduction of atherosclerotic events (myocardial infarction, stroke, and vascular death) in patients with atherosclerosis documented by recent stroke, recent myocardial infarction, or established peripheral arterial disease.
Clopidogrel Adverse Effect: Clopidogrel use is associated with several serious adverse drug reactions such as severe neutropenia, various forms of hemorrhage, and cardiovascular edema.
Coagulants And Anticoagulants Multiple Choice Questions And Answers
Question 1. What are the steps in fibrin formation?
- “Tissue factor” or thromboplastin is released from the endothelial wall.
- Contact of blood with collagen.
- Clots bind thromboxane A2.
- (1) and (2)
Answer: 4. (1) and (2)
Question 2. Proteins C and S are dependent on which vitamin for synthesis?
- Vitamin C
- Vitamin B
- Vitamin E
- Vitamin K
Answer: 4. Vitamin K
Question 3. What might cause a deficiency In Prothrombin (factor 2) or Stuart-Power factor (factor 10)?
- Liver disease
- Vitamin K deficiency
- (1) and (2)
- Renal disease
Answer: 3. (1) and (2)
Question 4. Which drug acts by competitive inhibition of vitamin K reductase?
- Desirudin (Iparavask)
- Warfarin
- Heparin
- Ezetimibe
- Niacin
Answer: 2. Heparin
Question 5. How much time is required for the peak anticoagulant effect of Warfarin?
- 3 hours
- 1 day
- 1 week
- 3 days
Answer: 4. 3 days
Coagulants And Anticoagulants Short Questions And Answers
Question 1. Define coagulant.
Answer:
Coagulant drugs, also called anti-inhibitor coagulant complexes, also help regulate blood coagulation.
Some diseases, such as hemophilia, lead to defects in blood coagulation and patients suffering from the disorder can bleed uncontrollably in response to relatively minor injury.
Question 2. Draw the structure and IUPAC name of Menadione.
Answer:
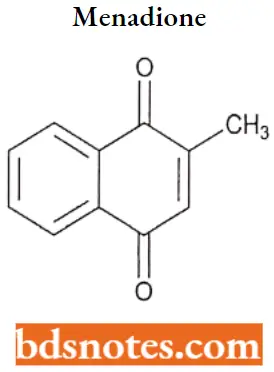
IUPAC name: 2-methyl-1,4-dihydronaphthalene-1,4-dione.
Question 3. Write the MOA of warfarin.
Answer:
Warfarin inhibits vitamin K reductase, resulting in depletion of the reduced form of vitamin K (vitamin KH2).
- As vitamin K is a cofactor for the carboxylation of glutamate residues on the N-terminal regions of vitamin K-dependent proteins, this limits the gamma-carboxylation and subsequent activation of the vitamin K-dependent coagulant proteins.
- The synthesis of vitamin K-dependent coagulation factors 2, 7, 9, and 10 and anticoagulant proteins C and S is inhibited.
- Depression of three of the four vitamin K-dependent coagulation factors (factors 2, 7, and 10) results in decreased prothrombin levels and a decrease in the amount of thrombin generated and bound to fibrin. This reduces the thrombogenicity of clots.

Leave a Reply