Coagulants And Anticoagulants
Question 1. Describe Hemostatic Drugs.
Or
Write Short Note On Local Hemostatics.
Or
Give A Brief Account Of Styptics Hemostatics.
Or
Write A Short Note On Styptics.
Answer:
Hemostatic drugs are substances that are used to stop bleeding from a site of vasospasm.
- Hemostatic drugs mainly used are local and are known as local hemostatic or styptics.
- They are particularly effective on the oozing surface.
- They can never be injected.
Read And Learn More: Pharmacology Question And Answers
- Hemostatic drugs are:
- Thrombin: It is obtained from bovine plasma. It is applied as a dry powder or freshly prepared solution on the bleeding surface. It is used in neurosurgery, skin grafting, etc.
- Fibrin: It is used as sheets or foam for covering or packing bleeding surfaces.
- Gelatin foam: It is moistened with a thrombin solution and is used for packing wounds.
- Vasoconstrictors: Like 1% solution of adrenaline may be soaked in sterile cotton gauze and packed to stop epistaxis or other similar bleeding.
- Astringent: Like tannic acid, it is used for bleeding gums, bleeding piles, etc.
- Russell’s viper snake venom: This consists of proteolytic enzymes. The venom acts as thromboplastin when it is applied locally and this stops external bleeding in hemophiliacs.
- Collagen: It leads to the aggregation of platelets and enhances the coagulation cascade.
- Calcium alginate: This is an absorbable hemostatic and leads to wound healing.
- Oxidized cellulose: It is also an absorbable hemostatic. Applied over the bleeding site in dry form it swells and causes clotting. This control bleeding from capillaries and arteries.
- Tranexamic acid: It is applied topically and acts as a hemostatic agent due to its fibrinolytic activity.
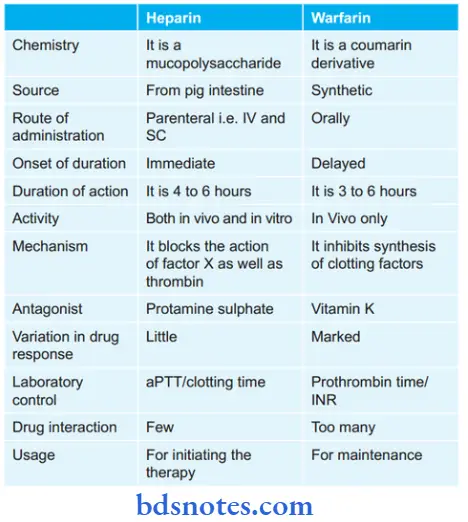
Question 2. Difference Between Heparin And Warfarin.
Or
State The Differences Between Heparin And Warfarin.
Or
Compare Heparin With Warfarin.
Answer:
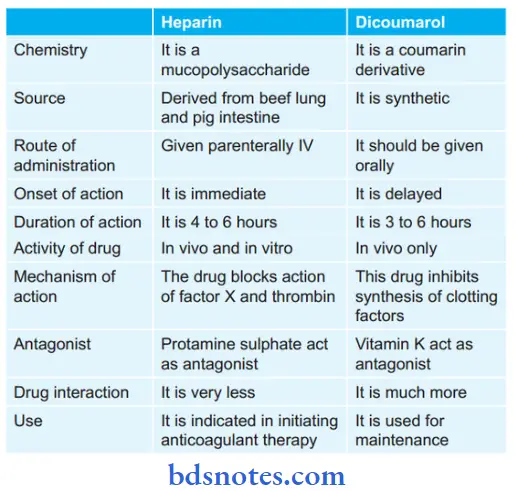
Question 3. Compare And Contrast Heparin And Dicoumarol.
Answer:
Question 4. Compare And Contrast Low Molecular Weight Heparin With Conventional Heparin.
Answer:
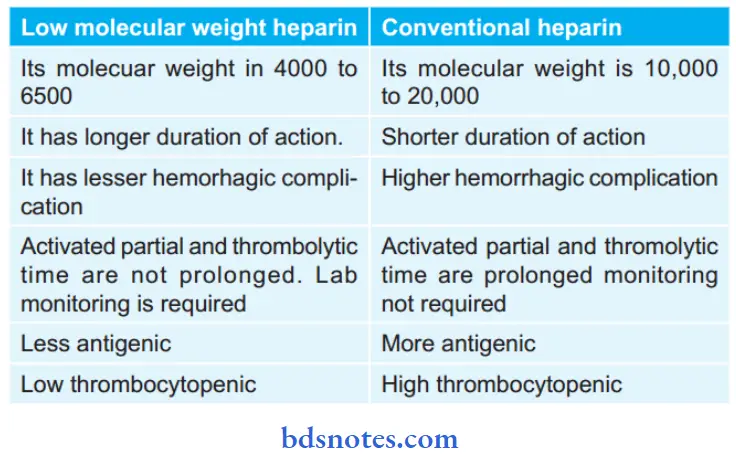
Question 5. Write A Short Note On Low Molecular Weight Heparin.
Or
Write In Brief On Lmwh (LowMolecular Weight Heparin).
Answer:
Low molecular weight heparins are enoxaparin, dalteparin, tinzaparin, ardeparin, reviparin, etc.
- Low molecular weight heparins are extracted from standard heparin by various techniques.
- These drugs produce anticoagulant effects by inhibition of factor Xa via antithrombin.
- These drugs have a small effect on partial prothrombin time and whole blood clotting time as compared to unfractionated heparin relative to anti-factor Xa activity.
- These drugs have less antiplatelet action and less interference with hemostasis.
- Effects of low molecular weight heparins are not completely reversed by protamine sulfate.
- These drugs are given subcutaneously.
Low Molecular Weight Heparin Advantages
- They have high subcutaneous bioavailability.
- They have longer half-lives so can be given once a day.
- These drugs do not need aPTT monitoring.
- The incidence of thrombocytopenia, bleeding, and osteoporosis is less.
Low Molecular Weight Heparin Uses
- Prophylaxis of deep vein thrombosis and pulmonary embolism in high-risk patients undergoing surgery.
- Treatment of established deep vein thrombosis.
- Unstable angina.
- In atrial firillation.
- In patients with prosthetic heart valves.
- It is preferred during pregnancy.
Question 6. Write In Brief About Oral Anticoagulants.
Answer:
- Oral anticoagulants are the drugs that prevent coagulation, i.e. it stops blood from clotting.
- The following are the oral anticoagulants:
- Coumarin derivatives: Warfarin, Dicoumarol
- Indandione derivatives: Phenindione
- Oral direct thrombin inhibitor: Dabigatran etexilate
- Oral anticoagulants are used only in vivo.
- These drugs act indirectly by interfering with the synthesis of vitamin K-dependent clotting factors in the liver.
- They act as a competitive antagonist of vitamin K and decrease plasma levels of active clotting factors in their dose-dependent manner.
- Oral anticoagulants should not be given with barbiturates or carbamazepine or rifampicin or griseofulvin as these drugs decrease the anti-coagulant effect of oral anticoagulants.
- In oral anticoagulants, coumarin derivatives are most commonly used.
- Dabigatran etexilate remains a prodrug and gets converted to dabigatran. This drug leads to the reversible inhibition of thrombin. It is indicated in the prevention and treatment of venous thromboembolism.
Question 7. Describe the Mechanism Of Action And Adverse Effects Of Heparin.
Answer:
Mechanism Of Action Of Heparin
- It acts indirectly by activating plasma antithrombin III and maybe other similar cofactors. The heparin antithrombin III complex then binds to clotting
factors of the intrinsic and common pathways (Xa, lla, lXa, Xla, Xlla, and Xllla) and inactivates them but not factor VIIa operative in the extrinsic pathway. At low concentrations of heparin, factor Xa-mediated conversion of prothrombin to thrombin is selectively affected. The anticoagulant action is exerted mainly by inhibition of factor Xa as well as the thrombin-mediated conversion of fibrinogen to firing. - Low concentrations of heparin prolong aPTT without significantly prolonging PT. High concentrations prolong both. Thus, low concentrations interfere selectively with the intrinsic pathway, affecting amplification and continuation of clotting, while high concentrations affect the common pathway as well.
Adverse Effects Of Heparin
- Bleeding due to overdose is the most serious complication of heparin therapy. Hematuria is generally the first sign.
- Thrombocytopenia is another common problem. Generally, it is mild and transient; occurs due to the aggregation of platelets.
- Transient and reversible alopecia is infrequent. Serum transaminase levels may rise.
- Osteoporosis may develop on long-term use of relatively high doses.
- Hypersensitivity reactions are rare—urticaria, rigor, fever, and anaphylaxis. Patients with allergic diathesis are more liable.
Question 8. Write A Short Note On Vitamin K.
Answer:
Vitamin K promotes coagulation and is used in the hemorrhagic states.
Types Of Vitamin K
- Vitamin K1 (from plants): Phylloquinone
- Vitamin K3 (Synthetic)
- Fat-soluble: Menadione, acetomenaphthone
- Water soluble: Menadione sodium bisulfate, menadione sodium diphosphate.
Vitamin K Action
It acts as a cofactor for γ carboxylation of the glutamic acid residue of clotting factors as well as osteocalcin. Vitamin K participates in the coagulation cascade.
Main Deficiency Disorders
- Hemorrhagic tendencies, i.e. epistaxis, bleeding gums, etc.
- Hypoprothrombinemia.
Vitamin K Therapeutic Doses
- Oral
- Menaclione sodium diphosphate: 5 mg
- Menadione sodium bisulfite: 2–5 mg.
- Parenteral
- Menadione sodium diphosphate: 5–75 mg IM or SC
- Menadione sodium bisulfite: 2–5 mg IM or SC.
Vitamin K Adverse Effects
Adverse reactions are seen on parenteral administration—allergic reactions and jaundice can occur.
Vitamin K Uses
- In the treatment of vitamin K deficiency
- Newborn babies lack intestinal flora and have low levels of prothrombin and other clotting factors. Routine administration of vitamin K 1 mg IM prevents hemorrhagic disease in the newborn.
- In the treatment of oral anticoagulant poisoning.
Question 9. Explain Why Warfarin Is Used As An Anticoagulant.
Answer:
Warfarin acts as an anticoagulant because they act by interfering with the synthesis of vitamin K-dependent clotting factors in the liver by inhibiting the epoxide reductase enzyme.
They block the carboxylation of glutamate residues in prothrombin, factors VIII, IX and X. Carboxylation is necessary for these factors to participate in coagulation. In this way, it acts as an anticoagulant.
Question 10. Write Short Note On Astringents In Dental Practice.
Or
Write Short Note On Uses Of Coagulants In Dentistry.
Answer:
Astringents should be used in the following conditions in dental practice:
- Vitamin C deficiency impairs collagen synthesis and causes bleeding gums and excessive post-extraction blood loss. Scurvy should be corrected before elective dental surgery. In case of emergency surgery, careful packing and pressure can stop the bleeding.
- Long-term corticosteroid therapy can also compromise hemostasis by impairing vessel retraction as well as by reducing platelet count. If dental surgery is implicated astringents should be used.
- Platelet function may be deficient due to thrombocytopenia or the use of drugs that inhibit platelet aggregation. Transfusion of platelet-rich plasma is indicated before dental surgery in patients with low platelet count. Corticosteroid therapy helps to restore platelet count in idiopathic thrombocytopenic purpura.
- Aspirin and other NSAIDs are the most important drugs that inhibit platelet aggregation. A large number of older individuals now receive long-term low-dose aspirin prophylaxis for ischemic heart disease or stroke. Many others receive long-term clopidogrel/ticlopidine for a variety of thromboembolic disorders.
- Several patients with arthritis regularly take NSAIDs. Discontinuation of aspirin for 5 days before dental surgery should be considered. In case this is not possible, proper packing and use of local hemostatics is needed to prevent excess bleeding.
- Even minor dental procedures (like scaling) put the hemophiliac patient at great risk of bleeding. The patient should be covered before and after the procedure with IV infusion of antihemophilic factor along with fibrinogen.
- The antifibrinolytic drug tranexamic acid has adjuvant value by reducing the requirement of an antihemophilic factor. Desmopressin injected IV also helps in checking dental bleeding in hemophiliacs as well as in von Willebrand’s disease by releasing factor VIII and von Willebrand’s factor from the vascular endothelium.
- Any oral surgery in patients on anticoagulant medication requires due care to avoid excessive bleeding. Since the action of IV heparin lasts for only 4–6 hours, the extraction can be scheduled at a time when anticoagulation is minimal.
- Low-dose SC heparin and LMW heparin therapy ordinarily do not increase dental surgery-associated bleeding. The heparin antagonist protamine may be given IV in case of an emergency bleed.
Question 11. Explain Why Heparin Is Used As An Anticoagulant.
Answer:
Heparin acts indirectly by activating plasma antithrombin III. The heparin-AT III complex then binds to clotting factors of the intrinsic and common pathways (Xa, IIa, IXa, XIa, XIIa, and XIIIa) and inactivates them but not factor VIIa operative in the extrinsic pathway.
At low concentrations of heparin, factor Xa-mediated conversion of prothrombin to thrombin is selectively affected.
The anticoagulant action is exerted mainly by inhibition of factor Xa as well as thrombin (IIa) mediated conversion of fibrinogen to firin’.
Question 12. Write Short Note On Antithrombolytics In Clinical Dentistry.
Answer:
Antithrombolytics are also known as antifibrinolytics.
These are the drugs that inhibit plasminogen activation and dissolution of clots.
Drugs used are epsilon amino caproic acid and tranexamic acid.
In clinical dentistry, they are used after tooth extraction in hemophilics.
They are also useful in reducing bleeding after tooth extraction or after dis impaction of the tooth.
In dentistry, tranexamic acid-soaked gauze or mouthwash is used to stop postoperative bleeding in hemophiliacs as well as in patients on anticoagulant therapy.
Question 13. Write Short Note On Anticoagulants.
Answer:
Anticoagulants are drugs that reduce the coagulability of the blood.
Anticoagulants Classifiation
1. Used in vivo
- Parenteral anticoagulant: Heparin, low molecular weight heparin, heparin sulfate
- Oral anticoagulants:
- Coumarin derivatives: Bishydroxycoumarin, Warfarin sodium, Acenocoumarol
- Indandione derivative: Phenindione
2. Used in vitro
- Heparin
- Calcium complexing agents: Sodium citrate, sodium oxalate, sodium edentate
Therapeutic Uses Of Anticoagulants
- In deep vein thrombosis and pulmonary embolism: Since venous thrombi are firing so anticoagulants are highly effective. In cases with pulmonary embolism and deep vein thrombosis treatment for 3 months should be employed.
- Myocardial infarction: In this anticoagulants prevents the extension of the thrombus and prevent the recurrent attack.
- Unstable angina: Short-term use of heparin reduces the occurrence of myocardial infarction in unstable angina patients.
- Rheumatic heart disease, atrial fibrillation: Warfarin or low-dose heparin is effective in preventing stroke. Anticoagulants should be given a month before and after converting atrial fibrillation to sinus rhythm.
- Vascular surgery, prosthetic heart valves, retinal vessel thrombosis, extracorporeal circulation, and hemodialysis: In all these anticoagulants are indicated with antiplatelet drugs for prevention of thromboembolism.
Question 14. Write Short Note On Heparin.
Answer:
Heparin is an anticoagulant drug that is used both in vivo and in vitro.
Heparin Pharmacokinetics
Heparin is given orally due to its high negative charge and large molecular size is not absorbed. It should be given IV or SC On given IV it immediately acts.
It does not cross the blood-brain barrier or placental barrier. It gets inactivated in the liver by the heparinase enzyme and its metabolites get excreted in urine.
Heparin Uses
- In unstable angina.
- In treatment of deep vein thrombosis.
- For maintaining the patency of cannula as well as shunts in dialysis patients.
Heparin Contraindications
Heparin is contraindicated in:
- Hemophiliacs
- In cases with heparin-induced thrombocytopenia
- Severe hypertension
- Bacterial endocarditis
- Intracranial hemorrhage
- Peptic ulcer
- Renal failure.
Question 15. Write A Short Note On Tranexamic Acid.
Answer:
Tranexamic acid is an antifibrinolytic drug.
Tranexamic Acid Mechanism Of Action
Tranexamic acid binds to the lysine binding site on plasminogen and prevents its combination with firing and prevents its lysis.
Tranexamic Acid Indications
It prevents or controls bleeding in the following situations:
- For the counteracting effect of fibrinolytic
- After cardiopulmonary bypass surgery
- In menorrhagia
- After extraction of the tooth, tonsillectomy, and prostatic surgery in hemophiliac
- In recurrent epistaxis, ocular trauma, bleeding peptic ulcer
- In dentistry, the drug is used with soaked gauze or mouthwash which reduces postoperative bleeding in hemophiliacs and patients on anticoagulant therapy.
Tranexamic Acid Side Effects
- Nausea and diarrhea
- Headache and giddiness
- Thrombophlebitis of injected vein.
Question 16. Name Three Antiplatelet Agents.
Answer:
The following are three antiplatelet agents:
- Aspirin
- Dipyridamole
- Clopidogrel.
Question 17. Classify And Enumerate Anticoagulants.
Answer:
Classifiation and Enumeration of Anticoagulants
1. Used in Vivo
- Parenteral anticoagulant:
- Indirect thrombin inhibitors: Heparin (unfractionated), low molecular weight heparins (enoxaparin, reviparin, nadroparin, dalteparin, parnaparin, ardeparin), fondaparinux, danaparoid
- Direct thrombin inhibitors: L lepirudin, bivalirudin, and argatroban.
- Oral anticoagulants:
- Coumarin derivatives: Bishydroxycoumarin, Warfarin sodium, Acenocoumarol, Ethyl biscoumacetate
- Direct factor Xa inhibitor: Rivaroxaban
- Oral direct thrombin inhibitor: Dabigatran etexilate
2. Used in vitro
- Heparin
- Calcium complexing agents: Sodium citrate, sodium oxalate, sodium edentate.
Question 18. Write The Basis Of Heparin Is Given Initially Before Warfarin.
Answer:
Warfarin works by being an antagonist to vitamin K. Vitamin K is the cofactor in the production of vitamin K-dependent clotting factors (factors II, VII, IX, and X).
However, the anticoagulant enzymes Protein C and S are also dependent on vitamin K and have shorter half-lives than the clotting factors II, IX, and X leading to paradoxical hypercoagulability at the initiation of therapy.
Thus, when warfarin is started first, there is a paradoxical initial prothrombotic effect. Heparin act by activating antithrombin III in plasma.
Normally antithrombin III inactivates several clotting factors, most importantly factor Xa and IIa (thrombin) but the reaction is very slow.
Heparin accelerates this inactivation process by binding to antithrombin III.
Only conformational change is required for the inactivation of factor Xa whereas the inactivation of thrombin is also dependent on the formation of scaffolding by HEPA- rin (that binds both antithrombin III and thrombin).
Heparin provides this scaffolding and thus inhibits both factors IIa and Xa. As heparin is inhibiting already activated factors, there is no time lag between the administration and action of this drug.
Therefore it can be used for the initiation of anticoagulant therapy before warfarin.

Leave a Reply