Clostridium
Question 1. Write a note on tetanus.
Or
Write in brief on tetanus infection.
Answer:
Tetanus is also called lockjaw and is an acute infection of the nervous system that is characterized by an intense activity of motor neurons which results in severe muscle spasms.
Types of Tetanus There are many clinical types of tetanus which are as follows:
- Tetanus neonatorum: It occurs from the contamination of the cut surface of the umbilical cord in infants.
- Postabortal and puerperal tetanus: It results from infection of the genital tract with unsterilized instruments and dressing.
- Puerperal tetanus is rare but most dangerous.
- Splanchnic tetanus: There is the involvement of muscle degeneration and respiration with dysphasia.
- Cephalic tetanus: It occurs from the wound of the head. There is a unilateral and bilateral contraction of the muscles of the face.
Read And Learn More: Microbiology Question And Answers
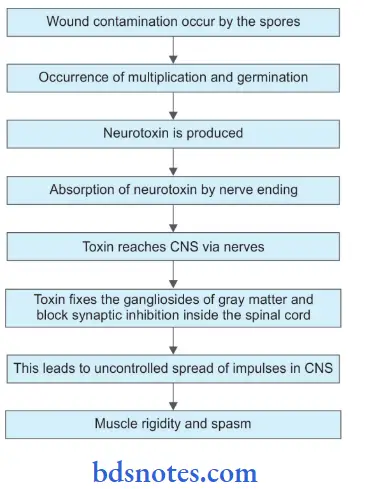
Etiology Tetanus is caused by the exotoxin of Clostridium tetani which acts to the synapse of interneurons of inhibitory pathways and motor neurons to produce blockade of the spinal inhibition.
Pathogenesis
Tetanus Clinical Features: Its incubation period is from 6 to 20 days.
Tetanus Prodromal Symptoms
- Malaise
- Fever
- Sweating
- Headache
- Irritability.
Tetanus Presenting Symptoms
- Trismus and dysphagia due to painful rigidity of masseter and muscles of deglutition lead to lockjaw.
- Pain and stiffness in neck and back.
Tetanus Symptoms of Established Disease
- Rigidity: Lumber lordosis, neck retraction, and abdominal rigidity.
Muscle Spasms
- Spasms of facial muscles appear with the raised eyebrows, tightly closed eyes, and drawing back of lips to exposed clenched teeth.
- Spasms of the larynx and respiratory muscle cause asphyxiation or respiratory arrest.
- Contractions of muscles of the back produce an arched back known as opisthotonus.
- Extension of lower limbs
- Flexed upper limbs
- Spinal convulsions
- Urine retention is frequent.
Signs due to Sympathetic Overactivity
- Cardiac arrhythmias
- Fluctuating blood pressure
- Marked variation in pulse rates.
- Peripheral vasoconstriction or vasodilatation.
Laboratory Diagnosis
- Microscopy: Gram staining may show gram-positive bacilli with a drumstick appearance.
- Culture:
- The specimen is inoculated on freshly prepared blood agar and incubated at 37°C for 24-48 hours under anaerobic conditions.
- Cl. tetani produces a swarming growth.
- The specimen is also inoculated in three tubes of cooked meat broth (CMB).
- One of these tubes is heated at 80°C for 15 minutes, the second tube for 5 minutes and the third left unheated.
- Heating for different periods is to kill vegetative bacteria while leaving tetanus spores undamaged.
- These cooked meat broths are incubated at 37°C and subcultured on blood agar plates daily for up to 4 days.
- Gram-stained smear from culture shows typical gram-positive bacilli with drumstick appearance.
- Agar stab culture shows a Fir tree-like appearance.
- Toxigenecity test:
- Pathogenicity of the isolated organism is established with a demonstration of toxin production. It is best tested in animals. 0.2 mL of 2 to 4 days old cooked meat culture is injected into the root of the tail of a mouse, the same amount is injected into another animal (control).
- That has received tetanus antitoxin (1000 units) an hour earlier. In a positive case, the test animal develops symptoms within 12-24 hours, beginning with stiffness of the tail.
- Rigidity proceeds to the leg on the inoculated side, the other leg, trunk, and forelimbs in that particular order. Death occurs within 2 days.
Tetanus Treatment
- Treat the patient in a special isolation unit.
- Cardiopulmonary monitoring should be done.
- Sedation, airway, and nutrition are maintained.
- Antibiotics, i.e. penicillin or metronidazole should be given.
- Injection of antitoxin serum should be given. Human tetanus immunoglobulin (TIG) 3000 to 6000 units IM. individual doses are given.
- Wound debridement should be done properly.
Prophylaxis of Tetanus
Question 2. Name the organisms responsible for pus formation and write about the colony characteristics of each of them.
Answer:
Pus-forming organisms are as follows:
- Streptococcus pyogenes
- Staphylococcus pyogenes
- Clostridium.
- Clostridium perfringens (C. welchii)
- Clostridium septicum
- Clostridium novyi.
Colony Characteristics
- Streptococcus pyogenes: It is an aerobe and facultative anaerobe.
- In fluid media, it shows granular growth with powdery deposits.
- In blood agar colony is small (pinpoint colonies) circular, transparent, and low convex with an area of hemolysis.
- It ferments lactose, glucose, sorbitol, maltose, etc.
- Staphylococcus pyogenes: It is an aerobe and grows readily on simple media.
- In fluid media, it produces uniform turbidity. No pigment is produced.
- In nutrient agar colony is pigmented, golden yellow, pin head sized, circular, convex, smooth, shiny, opaque with entire edge, and emulsifies easily.
- In blood agar, a wide zone of hemolysis is produced around colonies.
- Clostridium perfringens: It is an anaerobe, growing rapidly at 37°C.
- On blood agar, it produces target hemolysis. There are two zones present, i.e. the narrow zone of complete hemolysis because of theta-toxin and a wider incomplete
hemolysis because of alpha toxin. - On Robert’s cooked meat media, it grows very rapidly turning meat particles pink in color but there is no digestion of meat.
- On blood agar, it produces target hemolysis. There are two zones present, i.e. the narrow zone of complete hemolysis because of theta-toxin and a wider incomplete
Question 3. Mention the symptoms produced by Cl. Tetani. Write about its morphology and mention the names and actions of its toxins.
Answer:
Toxins Prodromal Symptoms
- Malaise
- Fever
- Sweating
- Headache
- Irritability.
Toxins Presenting Symptoms Trismus and dysphagia are due to painful rigidity of the masseter and muscles of deglutition leading to lockjaw. Pain and stiffness in neck and back.
Toxin Symptoms of Established Disease
- Rigidity: Lumber lordosis, neck retraction, and abdominal rigidity.
Muscle Spasms
- Spasms of facial muscles appear with the raised eyebrows, tightly closed eyes, and drawing back of lips to exposed clenched teeth.
- Spasms of the larynx and respiratory muscle cause asphyxiation or respiratory arrest.
- Contractions of muscles of the back produce an arched back known as opisthotonus
- Extension of lower limbs
- Flexed upper limbs
- Spinal convulsions
- Urine retention is frequent.
Signs due to sympathetic overactivity
- Cardiac arrhythmias
- Fluctuating blood pressure
- Marked variation in pulse rates.
- Peripheral vasoconstriction or vasodilatation.
Morphology of Clostridium Tetani
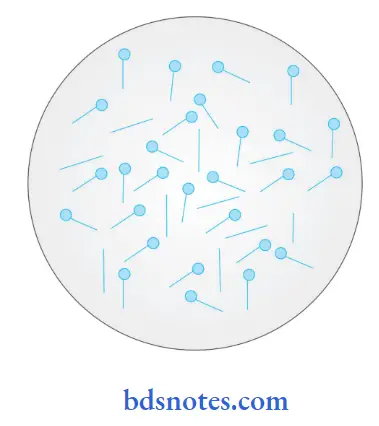
- It is slender, long, slightly curved, gram-positive bacilli
- Its size is 4 to 8 µm × 0.4 to 0.5 µm
- It can occur in the form of large filaments.
- It shows considerable variation in length.
- It is non-capsulated.
- It is motile by peritrichous flagella except Clostridium tetani type VI
- Spores formed are spherical, terminal, and bulging,
- Spores give a bacilli drumstick appearance.
Toxins and Action
- Toxins:
- Clostridium tetani produces two distinct toxins:
- Hemolysin (Tetanolysin)
- Neurotoxin (Tetanospasmin)
- A third toxin, i.e. non-spasmogenic peripherally active neurotoxin is identified. Its action in the pathogenesis of tetanus is unknown.
- Actions:
- Tetanolysin: It is heat-labile and oxygen-labile and is active against the RBCs of rabbits and horses.
- Tetanospasmin: It is neurotoxic. It reaches the CNS along the axons of motor nerve trunks. The toxin gets fied to the motor cell of anterior horn cells.
- It inhibits the release of cholinesterase which causes the accumulation of acetylcholine at the motor end plate which is responsible for the tonic rigidity of the muscles.
Question 4. Write notes on laboratory diagnosis of tetanus.
Or
Write a short note on the laboratory diagnosis of Cl. tetani.
The diagnosis of tetanus should always be made clinically and laboratory tests are done to confirm it. Specimens generally collected are wound, swabs, exudates, or tissue from the wound.
- Microscopy: Gram staining may show gram-positive bacilli with a drumstick appearance.
- Culture:
- The specimen is inoculated on freshly prepared blood agar and incubated at 37°C for 24-48 hours under anaerobic conditions. Cl. tetani produces a swarming growth.
- The specimen is also inoculated in three tubes of cooked meat broth (CMB). One of these tubes is heated at 80°C for 15 minutes, the second tube for 5 minutes and the third left unheated.
- Heating for different periods is to kill vegetative bacteria while leaving tetanus spores undamaged. These cooked meat broths are incubated at 37°C and subcultured on blood agar plates daily for up to 4 days.
- Gram-stained smear from culture shows typical gram-positive bacilli with drumstick appearance. Agar stab culture shows Fir tree appearance
- Toxigenecity test:
- Pathogenicity of the isolated organism is established with a demonstration of toxin production. It is best tested in animals. 0.2 mL of 2 to 4 days old cooked meat culture is injected into the root of the tail of a mouse, the same amount is injected into another animal (control) that has received tetanus antitoxin (1000 units) an hour earlier.
- In a positive case, the test animal develops symptoms within 12-24 hours, beginning with stiffness of the tail. Rigidity proceeds to the leg on the inoculated side, the other leg, the trunk, and the forelimbs, in that particular order. Death occurs within 2 days.
Question 5. Enumerate anaerobes causing wound infection.
Or
Describe in detail the laboratory diagnosis of gas gangrene.
Answer:
Following are the anaerobes that lead to wound infection:
- Gram-negative bacilli:
- Bacteroides
- Prevotella
- Porphyromonas
- Fusobacterium
- Bilophila Wadsworth
- Suttrella.
- Gram-positive cocci: Peptostreptococcus spp.
- Gram-positive:
- Spore-forming
- Clostridium spp.
- Non-spore-forming bacilli
- Actinomyces
- Propionibacterium
- Eubacterium
- Lactobacillus
- Bifidobacterium spp.
- Gram-negative cocci: Veillonella spp
Laboratory Diagnosis of Gas Gangrene
- Direct microscopy: Gram-stained smears show a large number of gram-positive bacilli without spores is indicative of Cl. perfringens.
- Culture: Specimens are inoculated on fresh and heated blood agar as well as cooked meat broth. Growth in cooked meat broth is subcultured on blood agar plate after 24-48 hours. Blood agar is incubated for 42-78 hours. It produces beta-hemolysis.
- Nagler reaction: Cl. perfringens is grown on a medium having 6% agar, 5% Fildes, a peptic digest of sheep blood, and 20% human serum or 5% egg yolk in a plate. Neomycin sulfate is added to this combination to make it more selective. To one-half of the plate, anti-toxin is spread over the surface. The inoculated culture plate is incubated at 37°C for 24 hours. Colonies on half of the plate without anti-toxin are surrounded by opacity, while colonies on the other half show no opacity due to the neutralization of alpha toxin.
- Animal pathogenicity: 0.1 mL of 24-hour growth in cooked meat broth is injected in healthy guinea pigs by IM route. The animal dies within 24 hours. A control animal protected with anti-serum survives. On autopsy bacteria from the heart and spleen of the test animal is collected.
- Biochemical test:
- Lecithinase C activity is positive.
- Lipase hydrolysis is negative
- Lactose fermentation is positive
- Proteinase activity is negative
- In litmus milk, lactose fermentation leads to the formation of acid which changes the color of litmus from blue to red.
- Acid coagulates the casein and clotted milk is disrupted due to vigorous gas production.
Question 6. Write a short note on tetanus prophylaxis.
Answer:
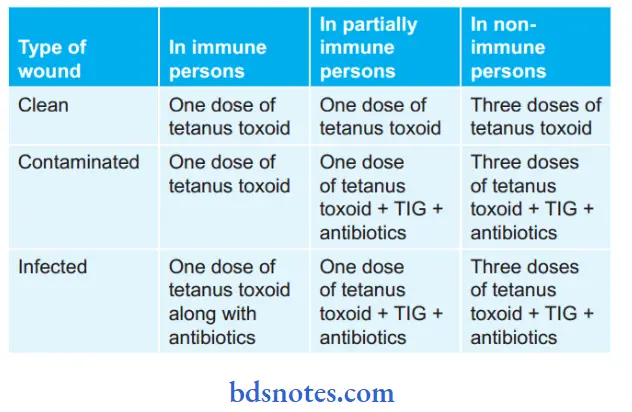
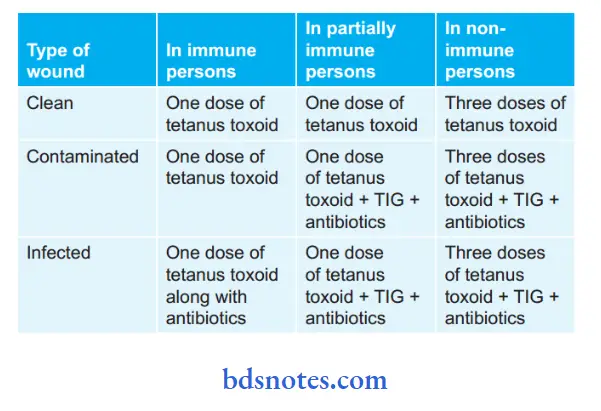
Tetanus prophylaxis depends on the type of wound and the immune status of the patient.
Methods of tetanus prophylaxis are:
- Surgical prophylaxis
- Antibiotic prophylaxis
- Immunization
- Active
- Passive
- Combined
- Surgical Prophylaxis: In these foreign bodies, necrotic tissues and blood clots are removed to prevent an anaerobic environment which is favorable for Clostridium tetani. Depending on the extent of the wound surgical treatment varies from cleaning to excision.
- Antibiotic Prophylaxis: In this tetanus bacilli and pyogenic bacteria are destroyed or inhibited in wounds. This leads to the prevention of the production of toxins. Here long-acting penicillin injection is the drug of choice. Commencement of antibiotics should be before the toilet of the wound. Local application of neomycin or bacitracin should be done Antibiotics produce no action on toxin so that is why they cannot replace immunization and are used as a helpful aid.
Immunization is of three types, i.e. active, passive, and combined.
- Active Immunization:
- This is gained by spaced injections of formal toxins. It is available as a plain toxoid or is adsorbed on aluminum hydroxide or phosphate. Adsorbed toxoid antigen is bettr.
- Tetanus toxoid can be given alone or with diphtheria toxoid and pertussis vaccine as a triple vaccine.
- The course of immunization consists of three doses of tetanus toxoid IM with an interval of 4–6 weeks between the first two injections and the third dose is 6 months later according to the National Immunization Programme.
- The full course provides immunity for 10 years. A booster dose should be taken after 10 years.
- Passive Immunization:
- Passive immunization is gained by injection of tetanus antitoxin. Antitetanus serum or tetanus antitoxin is derived from hyperimmune horses.
- It should be given in the dosage of 1500 IU given subcutaneously or intramuscularly in non-immune persons soon after receiving any tetanus-prone injury.
- Antitetanus serum carries two disadvantages, i.e. it leads to elevation of the immune system and hypersensitivity.
- The half-life of antitetanus serum in humans is 7 days, but in persons who have prior injections of horse serum, it is eliminated readily by combination with preexisting antibodies.
- This is also known as immune elevation.
- It is an emergency procedure that is to be used once.
- Combined Immunization: In this TIG (human antitetanus immunoglobulin) in one hand and toxoid on another hand is administered. This is followed by a second and third dose of toxoid at appropriate monthly intervals.
Summary of Tetanus Prophylaxis

Leave a Reply