Calculus And Other Etiological Factors Including Food Impaction
Question 1. Write short note on dental calculus.
Or
Write short answer on calculus.
Answer. Dental calculus is an adherent, calcified or calcifying mass that forms on the surfaces of teeth and dental appliances:
Types
Depending upon the position of calculus in relation to marginal gingiva it is classified as:
- Supragingival calculus: It is a tightly adherent calcified deposit that forms on the clinical crown of teeth above free gingival margin. It is clinically visible.
- Subgingival calculus: It is that calcific deposit which is formed on root surfaces below free marginal gingiva. It is believed to be formed from gingival exudates and is called seruminal calculus.
Structure
- Deposits of supragingival calculus are whitish yellow in color and get stained by tobacco or food pigments, while the subgingival calculus is dark brown or greenish black in color.
- The consistency is hard and clay like of supragingival plaque and in subgingival it is hard and film.
- The supragingival plaque is most abundant on lingual surfaces of lower anterior teeth, opposite Wharton’s duct, Bartholin’s duct and buccal aspect of maxillary molars opposite the stenson’s duct.
Read And Learn More: Periodontics Question And Answers
Composition
Inorganic Components
Component Dry weight (in%)
Inorganic 70–90
Calcium 27–29
Phosphorus 16–18
Carbonate 2–3
Sodium 1.5–2.5
Magnesium 0.6–0.8
Fluoride 0.003–0.04
Crystal forms
Hydroxyapatite 58
Magnesium whitlockite 21
Octacalcium phosphate 12
Brushite 9
Organic Components
Component Dry weight (in%)
Mixture of protein-polysaccharide 1.9-9.1
complex, desquamated epithelial cells,
leukocytes and various microorganisms
Carbohydrate (consists of glucose, galactose, rhamnose, mannose)
Proteins 5.9-8.2
Lipids 0.2
Formation
- Calculus is formed by precipitation of mineral salts, which can start between 1st and 14th day of plaque formation.
- In two days plaque can be 50% mineralized and 60 to 90% get mineralized in 12 days.
- calcification starts in separate foci on the inner surface of plaque. These foci of mineralization gradually, increase in size and coalesce to form solid mass of calculus.
- Calculus formation continues until it reaches maximum level in about 10 weeks and 6 months, after where there is decline in its formation, due to mechanical wear from food and lips, cheeks and tongue. This decline is called as reversal phenomenon.
Question 2. Write short note on subgingival calculus.
Answer. Subgingival calculus is located below the crest of marginal gingiva and therefore is not visible on routine clinical examination.
It is also known as serumal calculus.
Location
The location and extent of subgingival calculus is evaluated by careful tactile perception with a delicate dental instrument known as explorer.
Composition
In this salivary proteins are absent; more magnesium whitlockite; lesser brushite and octacalcium phosphate; sodium content increases with pocket.
Clinical Features
- Subgingival calculus is typically hard and dense and frequently appears dark brown and greenish black in color.
- It is found inside the gingival sulcus or the periodontal pockets.
- It appears first in interproximal areas where supragingival calculus already exists.
- This is occasionally seen on the dentures when it form in narrow grooves, mainly those at tooth – acrylic interface.
- Its consistency is flint like and it firmly adherent to the surface and is difficult to remove.
- It is not visible on routine oral examination, can be found by tactile exploration.
Diagnosis
Direct vision
The subgingival calculus is seen directly:
- By using gentle stream of air to reflect he gingival margin.
- By following gingival surgery
- During periodontal surgery.
Indirect vision
The subgingival calculus is seen indirectly:
- When gingival margin is dried, dark color of subgingival calculus is seen via the marginal tissue.
- By probing
- A fine calculus probe (WHO 621 probe) is used to detect subgingival calculus.
- Ball end of CPITN probe with light touch determines the location of subgingival calculus, which appears as rough area or catch on the root surface.
- Exploring: Use of subgingival explorer no. TU – 17 can detect the subgingival calculus.
- Radiographs and transillumination.
Question 3. Define calculus. Write in detail about supra-gingival, sub-gingival calculus, its formation, theories, etiologic significance and role of microorganisms in mineralization.
Or
Define dental calculus. Discuss the theories regarding mineralization of calculus.
Or
Write short note on theories of mineralization of calculus.
Or
Define and classify dental calculus. Describe theories of mineralization of dental calculus.
Answer. “Calculus is Defined as the hard deposit that forms by the mineralization of dental plaque and is generally covered by layer of unmineralized plaque.”
Classification of Dental Calculus
According to its relation to gingival margin. The dental calculus is classified as:
- Supragingival
- Subgingival
Supragingival Calculus
- It is tightly adherent calcified deposit that forms on the clinical crowns of the teeth above the free gingival margin. It is clinically visible. It is also called as salivary calculus because it forms from the saliva.
- It is white or yellow in color.
- It hard, clay-like consistency.
- Supragingival calculus is easily detachable from the tooth.
- It is commonly found on the buccal surface of maxillary molars and lingual surfaces of anterior mandibular teeth.
- Supragingival calculus consists of hydroxyapatite and octacalcium phosphate.
Subgingival Calculus
- It lies below the crest of gingiva.
- It is dense dark brown or greenish black in color.
- It has hard or flint-like consistency.
- This is more firmly attached to tooth surface.
- Ratio of calcium to phosphate is high subgingivally and there is increase in sodium content along with depth of pockets.
- Subgingival calculus consists of more magnesium whitlockite and less brushite and octacalcium phosphate when comparison is done between supragingival and subgingival calculus.
Formation of Calculus
- Calculus is the dental plaque which had undergone mineralization.
- Calculus is formed by precipitation of mineral salts which starts between 1st and 14th day of plaque formation.
- Under 2 days plaque can be 50% mineralized and rest 60 to 90% of plaque is mineralized in 12 days.
- calcification starts in separate foci on inner surface of plaque.
- These foci of mineralization increase in size and coalesce to form solid mass of calculus.
- Calculus formation continues till it reaches its maximum level in about 10 weeks and 6 months.
Theories of Calculus Formation
It can be explained mainly under two categories:
Precipitation of minerals can occur from a local rise in the degree of saturation of calcium and phosphate ions, this is explained in:
- Booster mechanism: It is the main mechanism of precipitation which states that precipitation of calcium phosphate salts leads to local rise in degree of saturation of calcium and phosphate ions due to following ways:
- Increase in pH of saliva is because of:
- Loss of carbon dioxide or
- Production of ammonia by dental plaque bacteria or
- Protein degradation during stagnation leads to precipitation of calcium and phosphate salts by lowering the precipitation constant.
- Increase in pH of saliva is because of:
- Colloidal proteins in saliva bind to calcium and phosphate ions and maintain the supersaturated solution. As saliva stagnates in the oral cavity, colloids settle down and supersaturated stage is no longer maintained. This leads to precipitation of calcium and phosphate salts.
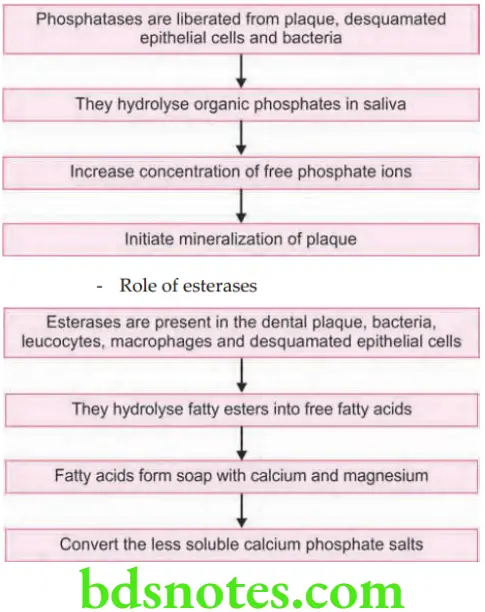
- Role of enzymes in precipitation of calcium and phosphate salts:
Role of phosphatases
Another concept that has been most widely held is “Epitactic Concept” (heterogeneous nucleation).
- According to this, seeding agents induce small foci of calcification. These foci enlarge and coalesce to form calculus. Hence, more appropriately called as heterogeneous nucleation. The seeding agents in calculus is not clearly known, but suspected agents could be, intercellular matrix of plaque, carbohydrate protein complexes and plaque bacteria.
Inhibition theory: This theory considers the possibility of calcification occurring only at specific sites because, there exists an inhibiting mechanism at non-calcifying sites. Wherever calcification occurs, the inhibitor is either altered or removed. One such inhibiting agents could be pyrophosphate which prevents the initial nucleus from growing, by possibly ‘poisoning’ the growth centers of the crystal.
Etiologic Significance
- The non-mineralized plaque on the calculus surface is the principal irritant, but the underlying calcified portion may be a significant contributing factor. It does not irritate the gingiva directly but provides a fixed nidus for the continued accumulation of plaque and retains it close to the gingiva.
- Subgingival calculus may be the product rather than the cause of periodontal pockets.
- Plaque initiates gingival inflammation, which starts pocket formation, and the pocket in turn provides a sheltered area for plaque and bacterial accumulation.
- The increased flow of gingival fluid associated with gingival inflammation provides the minerals that convert the continually accumulating plaque into subgingival calculus.
- Although the bacterial plaque that coats the teeth is the main etiologic factor in the development of periodontal disease, the removal of subgingival plaque and calculus constitutes the cornerstone of periodontal therapy.
- Calculus plays an important role in maintaining and accentuating periodontal disease by keeping plaque in close contact with the ‘gingival tissue and creating areas where plaque removal is impossible.
Role of Microorganisms in Mineralization
- Mineralization of plaque starts extracellularly around both gram-positive organisms and gram-negative organisms. It may also start intracellularly.
- Filamentous organisms, diphtheroids, and Bacterionema and Veillonella species have the ability to form intracellular apatite crystals.
- Calculus formation spreads until the matrix and bacteria are calcified.
- Bacterial plaque may actively participate in the mineralization of calculus by forming phosphatases, which changes the pH of the plaque and induces mineralization, but the prevalent opinion is that these bacteria are only passively involved and are simply calcified with other plaque components.
Question 4. Write short note on food impaction and its sequelae.
Or
Write short note on food impaction.
Answer.
- Food impaction is the forceful wedging of the food into the periodontium by occlusal forces.
- Cusps that tend to forcibly wedge food inter-proximally are known as ‘Plunger cusps’.
Food Impaction Types
- Vertical food impaction: Vertical food impaction results from the forceful wedging of food between the teeth by occlusal pressure.
- Horizontal food impaction: Horizontal food impaction results from the wedging of food debris between the teeth by the action of cheeks and tongue during mastication.
Food Impaction Causes
- Uneven occlusal wear: It can lead to food impaction because deflection of food away from proximal areas does not occur.
- Loss of proximal contact: Most common cause is due to periodontal disease, nonreplaced missing teeth, proximal caries and abnormal biting habits.
- Congenital morphologic abnormalities of teeth.
- Improperly constructed restoration.
- Lateral food impaction: Caused by occlusal forces, lateral pressure from cheeks, lips, tongue may force food interproximally.
Sign and Symptoms Associated with Food Impaction
Feeling of pressure and urge to dig the material between the teeth.
Vague pain that radiate deep in jaw.
- Gingival inflammation with bleeding and foul taste in involved area.
- Gingival recession.
- Periodontal abscess formation.
- Varying degrees of inflammatory involvement of PDL, sensitivity to percussion.
- Destruction of alveolar bone.
- Root caries.
Food Impaction Management
- Removal and correction of the etiological factors.
- Missing tooth to be restored.
- Recontouring of the occlusal and interproximal anatomy.
- If the interproximal contact areas cannot be re-established, then the embrasure should be made self-cleansing.
Sequelae of Food Impaction
- Feeling of pressure and urge to dig the material between the teeth.
- Vague pain that radiates deep in the jaws.
- Gingival inflammation with bleeding and a foul taste in the involved area.
- Gingival recession
- Periodontal abscess formation.
- Varying degrees of inflammatory involvement of periodontal ligament with an associated elevation of the tooth in its socket, prematurity in functional contact and sensitivity to percussion.
- Destruction of the alveolar bone.
- Root caries.
Question 5 Oral cavity contains more than 100 types of microorganisms still oral wounds heal as fast as any other wound in body. Justify.
Answer. The rapid healing in oral mucosa is directly related to intrinsic characteristics of the oral tissue and not to environmental such as microflora.
- Oral epithelium has large amount of palmitic acid (16:0) due to which there is a high energy metabolism in the oral mucosa.
- In the oral cavity, saliva provides many essential growth factors, making macrophage function less critical. Saliva has large amounts of cytokines, growth factors, and protease inhibitors which are the primary factors that account for rapid oral wound healing.
- Microorganisms in the oral cavity stimulate wound healing.
- Wounds of oral mucosa were shown to contain significantly lower levels of macrophages, neutrophils and T-cells when compared with wounds of any other part of body.
Question 6. Write short note on periodontal disease and iatrogenic factors.
Answer. Iatrogenic factors are any dental procedures that contribute to the deterioration of the periodontal tissues, e.g. quality of dental restoration or prosthesis.
Conservative Dentistry Factors
- Use of the rubber dam clamps, copper bands, matrix bands and disks in such a manner as to lacerate the gingiva. This results in varying degree of inflmmation.
- Restorative materials: It remains rough, unpolished the restoration surfaces favor plaque accumulation and contributes to periodontal diseases.
- GIC and porcelain seems to retain less plaque and are more acceptable from the periodontal point of view.
- Highly polished surfaces of porcelain inhibit plaque accumulation and permit its rapid removal.
- Fluoride constantly leaking from GIC prevents the attachment of the bacteria to the pellicle and it also interferes with the metabolism and growth of the bacteria.
- Subgingival restorations are plaque retentive areas that are inaccessible to scaling instruments, hence greater chance of severe gingivitis and deeper pockets.
- Overhanging dental restorations has been considered to be a contributing factor to gingivitis and possible periodontal attachment loss. Overhanging dental restorations not only increase plaque mass but also increases the specific periodontal pathogens in the plaque.
- Over-contoured or improperly contoured restorations tend to accumulate plaque and possibly prevents the selfcleansing mechanisms of adjacent cheek, lips and tongue.
- Poorly constructed restorations will cause occlusal disturbances that may be injurious to the supporting normal periodontal tissues. This type of tissue injury is called as ’primary trauma from occlusion.
Prosthodontic Factors
- Failure to replace the extracted teeth initiates a series of changes that produce various degrees of periodontal diseases.
- Insertion of prosthesis, replacement that creates excessive forces on the abutment or antagonist teeth.
- Excessive forces on the abutment results in increased mobility of abutment with gingival inflammation and periodontal pocket formation.
- Presence of RPD accentuates increased plaque formation and predisposes to gingival inflammation. Presence of RPD not only induces quantitative changes in plaque, but also qualitative changes by promoting development of most pathogenic bacteria.
Orthodontic Factors
Miller has listed 8 possibilities for periodontal breakdown brought about by the orthodontic treatment.
- Too rapid movement
- Too vigorous pressure
- Not allowing sufficient resting time between application of pressure
- Moving the teeth into traumatic occlusion.
- Unusual tissue responses
- Endocrine factors
- Nutritional deficiencies
- Undue displacement of the apex.
Question 7. Write short note on modes of attachment of calculus to tooth surface.
Answer. Following are the modes of attachment of calculus to tooth surface:
- Attachment by means of an organic pellicle or cuticle that seems to predominate on the enamel but occurs infrequently on cementum.
- Mechanical interlocking in surface irregularities such as resorption lacunae and caries
- Penetration of calculus bacteria in cementum.
- Close adaptation of calculus under surface depressions to the gently sloping mounts of unaltered cementum surface.
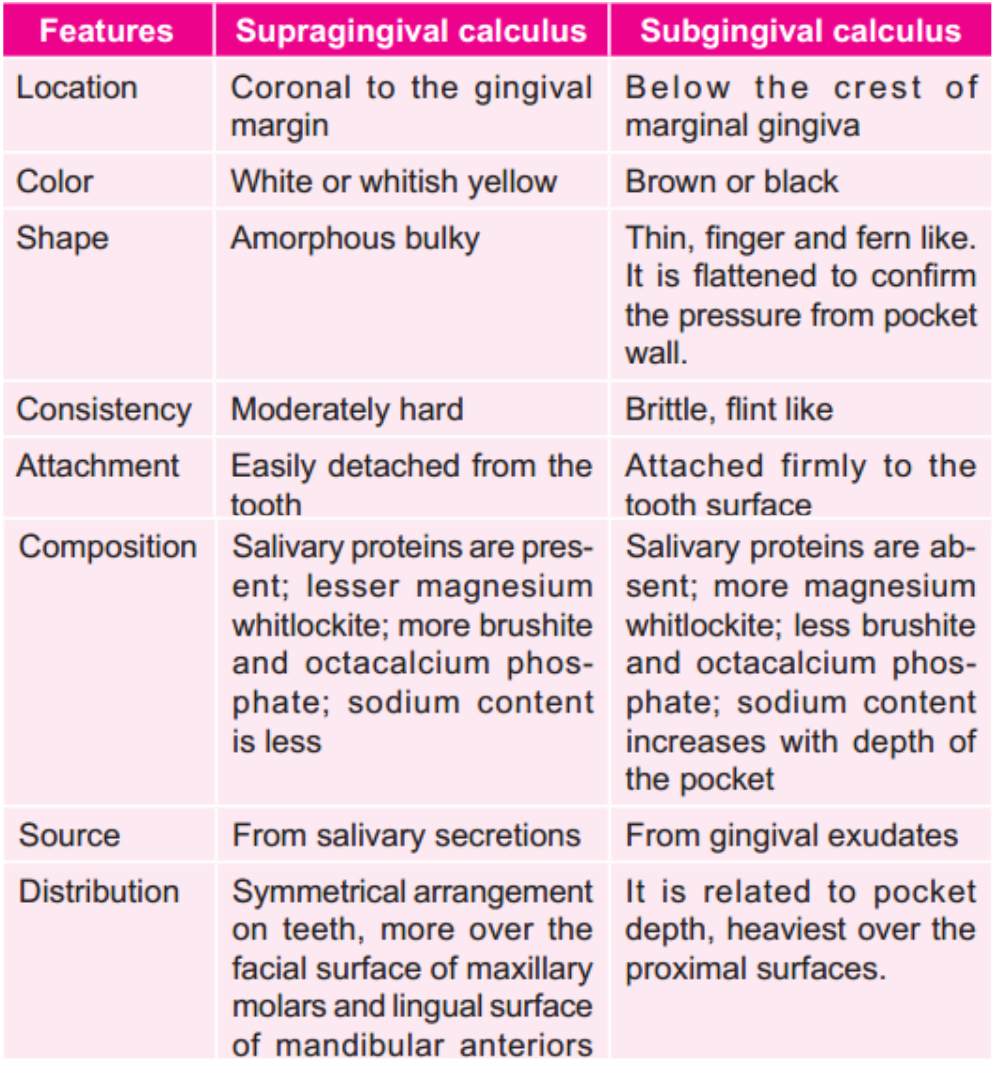
Question 8. Write the differences between supragingival and subgingival calculus.
Answer.
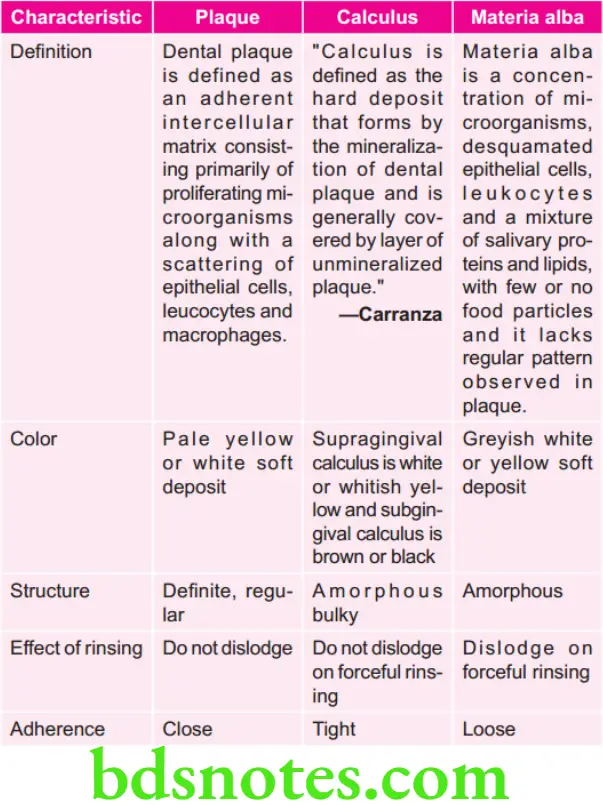
Question 9. Define and differentiate plaque, calculus and materia alba.
Answer.

Leave a Reply