Nursing Management In Common Childhood Diseases
Nutritional Deficiency Disorders Short Answer Questions
Question 1. Diarrhoea-fluid management.
Answer:
Diarrhea Introduction:
- Diarrhea is derived from a Greek word, meaning ‘flowing through’. It is a common cause of infant deaths worldwide. It is the second leading cause of death in children under 5 years of age.
- The loss of fluid through diarrhea can cause dehydration, which if not managed promptly may result in death of the child.
- Diarrhea is both treatable and preventable.
Read And Learn More: Bsc Nursing 3rd Year Child Health Nursing Previous year Question And Answers
Diarrhea Definition:
- According to the World Health Organization, diarrhea is defined as the ‘passage of 3 or more loose stools per day or passing more stools than normal for the age’
- It is the change in consistency of stools rather than the number of stools that is more important.
Diarrhoea Classification:
On the basis of duration: On the basis of duration for which diarrhea lasts, it is of 2 types:
- Acute diarrhea: If an episode of diarrhea lasts for less than 14 days, it is known as acute diarrhea.
- Chronic Diarrhea: If diarrhea lasts for 14 days or more, it is known as chronic diarrhea.
Diarrhoea Management: The management of infants and young children with diarrhea and dehydration focus on:
- Replacement of the fluids
- Administration of prescribed drugs
- Maintenance of nutritional status
- Prevention of Diarrhea
- Educating parents
Fluid replacement:
- Oral rehydration therapy is of prime importance for the replacement of lost fluids in dehydrated patients.
- Oral rehydration refers to drinking of solution which contains clean water, sugar, and mineral salts in order to replace the fluid and electrolytes lost from the body during diarrhea.
Administration of ORS:
Oral rehydration solution (ORS) can be used to prevent the development of dehydration and in many cases is a lifesaver. Homemade solutions that can be used for oral rehydration are salted rice water, salted pulses (daal) water, salted yogurt drinks (lassi, chachh), and vegetable and chicken soups.
At home, ORS can be prepared by mixing in 1 litre of water, three-finger pinch salt (3 grams), and two tablespoons sugar (18 grams). This solution should be given to the child after every loose stool.
WHO and UNICEF recommended and distributed ORS packets as a drug for treatment of clinical dehydration. In 1984, another mixture containing trisodium citrate instead of sodium bicarbonate was developed, with the aim of improving the stability of ORS in hot and humid climates.
The new ORS has lesser glucose and salt concentration which reduces the possible adverse effects of hypertonicity. The contents of readymade ORS packets are to be dissolved in one litre of clean drinking water.
1. Treatment plan A:
- This plan is followed for patients without the physical signs of dehydration or having mild dehydration. For children with mild dehydration, mothers are educated to give increased amount of home-based fluids to the child, like rice water, salted lassi, lemon water, coconut water, soups, fruit juice, daal water etc.
- In addition, homemade ORS can be prepared and given to the child.
- The mother should be told to administer ORS after each loose stool in the amount mentioned in table below.
- WHO recommends that if the child vomits, wait for five to ten minutes and then start giving the solution again, slowly. Also the mother should be asked to take the child to the physician if the child does not get better within 3 days or if he develops any danger signs of dehydration.
2. Plan B:
This treatment plan is followed for patients with signs of moderate dehydration. These Patients need to be treated in a health centre or hospital. The fluid therapy for patients with moderate dehydration has three components
- Correction of existing water and electrolyte defect (Rehydration therapy)
- Replacement of ongoing losses due to continuing diarrhea (Maintenance therapy)
- Provision of normal daily fluid requirement
3. Treatment Plan C:
- This treatment plan is followed for children with severe dehydration. In severe dehydration,
start intravenous fluids immediately. Also, give ORS if the child can drink. The best IV fluid solution that should be given is the Ringer lactate solution. - An ideal preparation is Ringer lactate with 5% dextrose. If ringer lactate is not available, normal saline (0.9%) can be used. Any of these solutions should be given in a dose of 100 ml/kg body weight.
Question 2. Vitamin A deficiency and its prevention
Answer:
Lack of vitamin A is called vitamin A deficiency. It is common in developing countries. Night blindness is the one of the first sign of vitamin A deficiency.
Vitamin A Deficiency:
- Breast milk of mothers with vitamin A deficiency contains little vitamin A which provides the breast fed child with too little vitamin A.
- bInfective absorption of vitamin A in the body can also lead to vitamin A deficiency.
- Malnutrition: Inadequate intake of vitamin A in the diet leads to Vitamin A deficiency.
- Zinc deficiency: Deficiency of zinc can impair the absorption, transport and metabolism of vitamin A because it is essential for synthesis of vitamin transport proteins.
- Iron deficiency: It can affect vitamin A uptake
Clinical Manifestations of Deficiency:
Night blindness: There is difficulty for the eyes to adjust to dim light. The affected individuals are unable to distinguish images in low levels of illumination. They have poor vision in dark but can see normally in adequate light. Night blindness caused by Vitamin A deficiency is associated with loss of goblet cells in the conjunctiva of eye.
- Xerophthalmia: A condition in which eye fails to produce tears.
- Xerosis Conjunctiva: Conjunctiva is dry, thickened, wrinkled and pigmented due to keratinisation of epithelial cells.
- Xerosis Cornea: Dryness spreads to cornea.
- Bitot’s spot: Greyish or white plaques formed of desquamated conjunctival epithelium, adhering to conjunctiva.
- Keratomalacia: Untreated xerosis of conjunctiva and cornea leads to development of keratomalacia. The corneal epithelium becomes opaque and ulcerated. This leads to bacterial invasion of cornea that results in blindness.
- Follicular hyperkeratosis (Phrynoderma): There is hyperkeratinisation of epithelial lining of hair follicles. The skin becomes rough, dry and papules develop on skin.
- Growth retardation
- Impaired immunity (increased risk of ear infection and urinary tract infection): Vitamin A is required for the proliferation of T-killer cells. A deficiency of Vitamin A suppresses the T cells, thereby causing impaired immunity.
Vtamin A Management:
- Supplementation: Mild to moderate cases should be given 10,000µg/daily. Severe cases should get 50,000µg/daily for few weeks
- Dietary consumption: Consumption of yellow or orange fruits and vegetables which contain carotenoid especially B-carotene is beneficial.
Vitamin A Prevention:
- Vitamin A, Palmitate-A, and Aquasol A are the drugs available in the market as Vitamin A supplements. These supplements must be given to the children as per physicians order.
- Maternal high supplementation benefits both mother and breastfed infant. High dose of vitamin A supplementation to lactating mother in first post-partum month can provide breastfed infants with the appropriate amount of vitamin A through breast milk.
- Increased consumption of vitamin A-rich food of animal origin, in addition to fruits and vegetables, is the best way of preventing Vitamin A deficiency.
- Diet which is rich in vitamin A should be given to growing children.
- Reduce frequency and severity of factors contributing to Vitamin A deficiency/ For example, PEM, Diarrhea, and Measles.
- Administration of Vitamin A as a part of the immunization schedule. Fortification of foods with vitamin A is costly but can be done in wheat, sugar, and milk.
Question 3. Protein-energy malnutrition.
Answer:
Protein Energy Malnutrition:
Protein Energy Malnutrition (PEM) is defined as a range of pathological conditions arising from a coincident lack of varying proportions of protein and calorie, occurring most frequently in infants and young children and often associated with infection (WHO,1973) PEM affects children under 5 years of age belonging to the poor underprivileged communities.
Under nutrition is a complex condition with multiple deficiencies such as proteins,energy, and micro nutrient deficiencies often occurring together. According to WHO, malnutrition is an underlying factor in over 50 % of the 10 – 11 million yearly deaths of children under 5 years.
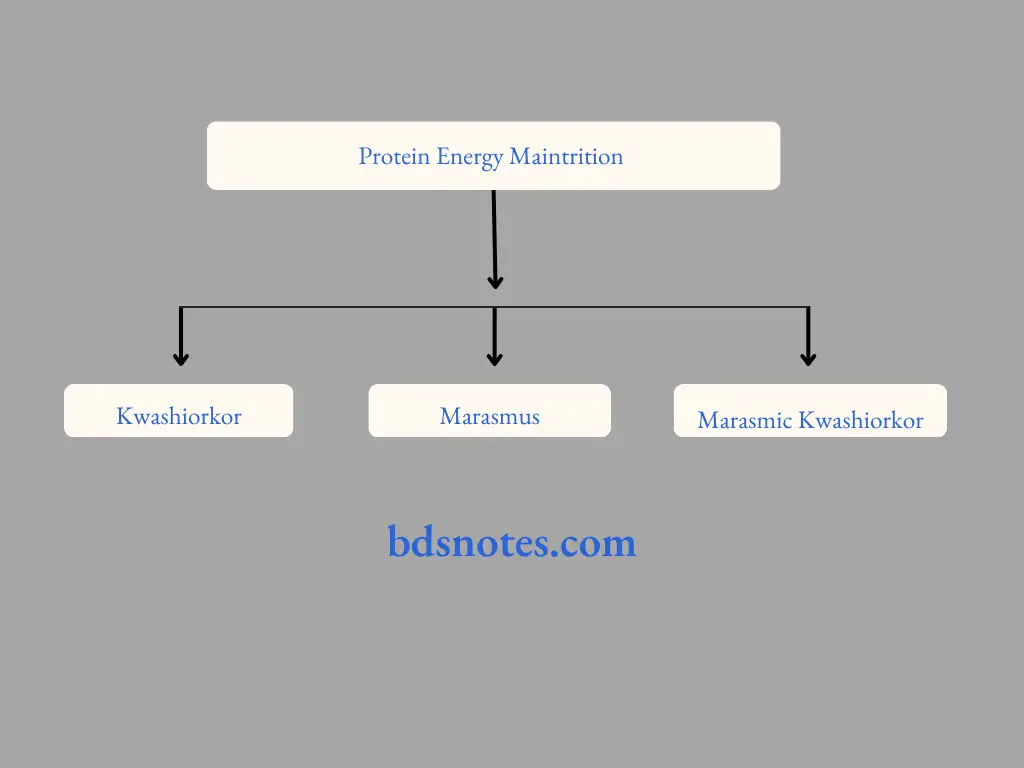
Classification of PEM:
Protein-energy malnutrition may be classified into three types as follows:
1. Kwashiorkor:
- Kwashiorkor is due to inadequate protein in the diet despite an adequate calorie intake
- Children are more affected by kwashiorkor than adult. it typically than adults. It typically starts after the child has breast milk has been replaced by diet with low in protein, although it can occur in infants if the mother is protein deprive.
- Kwashiorkor is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates.
- It cause by sufficient calorie intake but with insufficient protein consumption, which distinguishes it from marasmus.
2. Clinical signs and symptoms:
Growth failure:
- Oedema of the face and lower limbs
- Muscle wasting
- Fatty liver
- Anorexia(loss of appetite)
- Diarrhea
- Change in the color, sparse, soft, and thin hair.
- Change in the color of the skin(hypo and hyperpigmentation)
- Anaemia
- Vitamin A deficiency
- Angular stomatitis(Cracks in the corners of the mouth)
- Cheilosis (inflammation and cracks in lips)
- Moon face
Marasmus:
This is caused by a severe deficiency of proteins and calories in the diet. The important features are as follows:
- Severe wasting of muscles
- Loss of subcutaneous fat (Limbs appear as skin and bones)
- Skin is dry and atrophic
- Anaemia
- Eye lesions due to Vitamin A deficiency
- Irritability and fretfulness
- Diarrhea
- Dehydration
- Body temperature is sub-normal
- Failure to thrive
- Wrinkled skin – Old man’s face
- Grossly underweight
3. Marasmic Kwashiorkor:
Children suffering from this disease show signs of both kwashiorkor and marasmus.
Question 4. Kwashiorkor.
Answer:
Kwashiorkor is due to inadequate protein in the diet despite an adequate calorie intake
- Children are more affected by kwashiorkor than adults. it typically than adults. It typically starts after the child has breast milk has been replaced by diet low in protein, although it can occur in infants if the mother is protein-deprived.
- Kwashiorkor is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates.
- It is caused by sufficient calorie intake but with insufficient protein consumption, which distinguishes it from marasmus.
- Kwashiorkor occurs in areas of famine or poor food supply.
- Kwashiorkor is a severe form of malnutrition associated with a deficiency in dietary protein, the extreme lack of protein causes an osmotic imbalance in the gastro-intestinal system causing swelling of the gut diagnosed as an edema or retention of water.
Kwashiorkor Sign and symptoms:
- The defining sign of kwashiorkor in a malnourished child is pitting edema. (Swelling of ankles and feet).
- Other signs includes a distended abdomen, an enlarged liver wuth fatty infiltrate , thinning of liver ,loss of teeth , skin depigmentation and dermatitis.
- Generally, the disease can be treated by adding protein to the diet, however, it can have a long term impact on a child physical and mental development, and in severe cases may leads death.
Question 5. Malnutrition.
Answer:
Definition of malnutrition:
Faulty nutrition due to inadequate or unbalanced intake of nutrients or their impaired assimilation or utilization. Malnutrition occurs when the body doesn’t get enough nutrients.
Causes include a poor diet, digestive conditions, or another disease:
- Malnutrition is a condition that occurs that results from eating a diet in which more nutrients are not enough or are to much that the diet causes health problems.
- It may involve calories, protein, carbohydrates, fat, vitamins, or minerals.
- No enough nutrients is called undernutrition or undernourishment while too much is called overnutrition.
- Malnutrition is often used to specifically refer to undernourishment where an individual is not getting enough calories, proteins, or micronutrients.
- If undernutrition occurs during pregnancy or before two years of age it may result in permanent problems with physical and mental development.
- Extreme undernourishment known as starvation may have symptoms that include a short height, thin body, very poor energy levels, and swollen legs and abdomen.
- People also often get infectious and are frequently cold. The symptoms of micronutrients deficiencies depend on micronutrient deficiencies depend on the micronutrient that is lacking.
- Undernourishment is most often due to not enough high-quality food being available to eat this is food being available to eat This is often related to high food price and poverty.
There are two main types of undernutrition:
- Protein-energy malnutrition (PEM)
- Dietary deficiencies
Protein-energy malnutrition has two severe forms:
- Marasmus ( A lack of protein and calories)
- Kwashiorkor ( A lack of protein )
Dietary deficiencies: A lack of iron, iodine, vitamins, and minerals.
We can beat malnutrition by giving food security to people. Gov to be take a proper actions and efferts to bring modern agricultural techniques to increase food quality and quantity and increases nutrients contains.
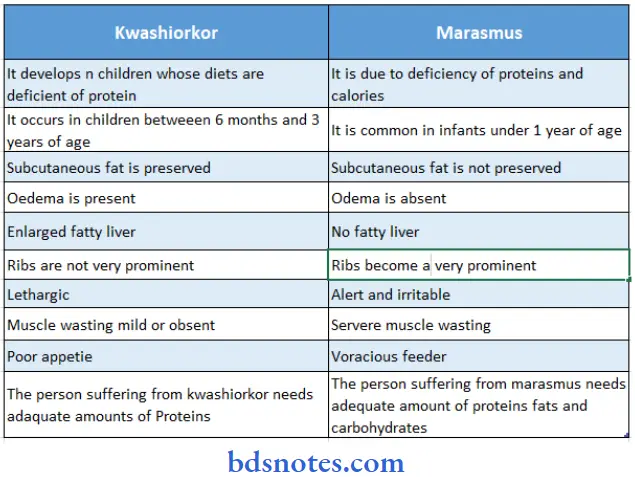
Question 6. Difference between kwashiorkor and marasmus
Answer:
Difference between kwashiorkor and marasmus:
Disorders Of Respiratory System Long Answer Questions
Question 7.
- Define Bronchopneumonia.
- Enlist the Causative agents, and clinical features of Bronchopneumonia.
- Explain the nursing management of patients with Bronchopneumonia
Answer:
Broncho Pneumonia Definition
Pneumonia is defined as acute inflammation and consolidation of lung parenchyma.
Broncho Pneumonia Incidence:
- Pneumonia in children is a major concern in developing countries because 1/3rd of all hospital out patients comprise of acute respiratory infections of which nearly 30% have pneumonia.
- It is the second leading cause of death in children under five years of age.
- Classification Pneumonia can be classified on anatomic and etiologic basis.
1. Classification on anatomic basis:
- Lobar or lobular pneumonia: One or more lobes of the lungs are involved.
- Interstitial pneumonia: Interstitial tissues of the lungs are affected.
- Bronchopneumonia: Patchy consolidation of lungs is known as bronchopneumonia.
2. Classification on an etiologic basis:
- Bacterial pneumonia: It may be caused by Pneumococcus, Streptococcus, Staphylococcus, Hemophilus influenza and H. pertussis.
- Viral pneumonia: It is caused by viruses like Influenza, Measles, Adenovirus and Respiratory Syncytial Virus.
- Fungal pneumonia: It may be caused by histoplasmosis and Coccidiomycosis.
- Protozoal pneumonia: It is caused by Pneumocystis camii, Toxoplasma gondii and Entamoeba histolytica
3. Miscellaneous types:
- Aspiration Pneumonia: It is caused by the aspiration of food, nasal drops, amniotic fluid by newborns, water (drowning), and chemicals like kerosene oil, etc.
- Loffler’s pneumonia: It is a disease in which eosinophils accumulate in the lungs, in response to parasitic infection. It may be caused by parasites like Ascaris lumbricoides, Strongyloide stercoralis and Ancylostoma duodenale.
- Hypersensitivity pneumonitis: It is an inflammation of the alveoli within the lungs caused by hypersensitivity to inhaled dust.
- Hypostatic pneumonia: It results from collection of fluid in dorsal region of lungs and occurs especially in those confined to bed for long time (like bedridden or elderly persons).
Broncho Pneumonia Clinical Features:
Clinical features of Pneumonia include
- Sudden onset
- High fever with chills
- Cough with thick sputum
- Increased respiratory rate
- Grunting respiration
- Nasal flaring
- Running nose
- Irritability
- Malaise
- Sore throat
- Anorexia
Late Symptoms Include:
- Convulsions
- Drowsiness
- Inability to drink from the mouth
- Chest in drowning
- Wheezing
- Hoarseness of voice
- Cyanosis
- Pleural pain which may be increased by deep breathing is referred to shoulder or abdomen.
Broncho Pneumonia Management: Nursing Management
1. Make continuing assessment:
- Monitor the child’s respiratory rate and pattern.
- Monitor breath sounds to note presence of rales, ronchi and wheezing.
- Observe for signs of respiratory distress.
2. Facilitate respiratory efforts:
- Maintain patent airway and provide high humidity atmosphere.
- Administer oxygen to maintain the oxygen saturation in blood.
- Place the child in semi-fowlers position to help in breathing.
- In case of unilateral pneumonia, make the child lie on the affected side, to splint the chest wall and prevent painful pleural rubbing.
- Position of the child should be changed frequently to prevent pooling of secretions in lungs.
- Keep the child warm and comfortable.
- Administer cough suppressants and bronchodilators, as prescribed.
- Provide steam inhalation and chest physiotherapy to help in drainage of secretions.
- If the child is old enough, teach him effective coughing and deep breathing.
- Give increased amount of fluids as this will help in liquefying the thick tenacious secretions.
3. Control fever:
- Provide bed rest to the child.
- Administer the prescribed antibiotics.
- Tepid sponging is done to reduce fever.
- Increase the fluid intake to prevent dehydration.
- Maintain fluid and electrolyte balance along with nutritional status of the child.
- Provide adequate fluids to meet the increased fluid demand of the body.
- If the child is having breathing difficulty, do not give anything orally as there is greater risk of aspiration.
- When oral feedings are started, after the child’s condition permits, feed the child slowly and carefully to prevent aspiration and aggravation of cough.
- Give high calorie liquid diet to the child.
Promote rest and sleep:
- Handle the child as little as possible to provide rest. Provide diversion therapy to the child to avoid boredom.
- Administer mild sedatives (if prescribed) when the child is restless or irritable.
- Make the baby lie on affected side, to splint the chest wall and reduce pleural pain.
- Administer cough suppressants before the baby sleeps.
Question 8. Respiratory Distress Syndrome
Answer:
Respiratory Distress Syndrome Introduction:
Respiratory distress syndrome of newborn previously called hyaline membrane disease, is a syndrome in premature infants caused by developmental insufficiency of surfactant production and structural immaturity of the lungs.
- Respiratory Distress syndrome is the leading cause of death in preterm infants. It occurs in 50% babies born at 26-28 weeks and 25% of babies born at 30-31 weeks.
- Idiopathic respiratory distress syndrome is an acute disorder that occurs almost exclusively in premature infants.
- The syndrome is more frequent in infants of diabetic mothers and those born by cesarean section.
Respiratory Distress Syndrome Clinical Features:
Respiratory Distress Syndrome begins shortly after birth and is manifested by
- Tachypnea
- Tachycardia
- Chest Wall Retractions
- Expiratory Grunting
- Nasal Flaring and
- Cyanosis
As the disease progresses the baby may develop ventilatory failure (rising CO2 concentration in blood) and prolonged cessation of breathing
Respiratory Distress Syndrome Diagnostic Evaluation:
- Physical examination:
- Most neonates who have Respiratory distress syndrome experience breathing difficulty at birth within 2 hours after birth.
- Silverman retraction score is a very good method of assessing the severity of respiratory distress. The most common sign of abnormal ventilation is tachypnea, a respiratory rate of over 60 breaths /minute.
- The infant has grunting on expiration. Nasal flaring is also present, which indicates respiratory distress.
- Auscultation of the chest reveals diminished breath sounds. As the baby’s condition worsens, bradycardia or tachycardia occurs.
- Physical examination: These infants are generally flaccid hypoactive and motionless. They assume a typical frog-legged position. The neonate may have pallor, oedema, hypothermia and shock-like state in severe conditions.
- Chest x-ray: Chest x-ray of baby shows areas of atelectasis and an air bronchogram shows air filled bronchi.
- Arterial blood gas analysis is done which shows arterial pco2 above 65mm of Hg (though the normal upper limit is 45mm Hg), an arterial po2 of 40mm Hg (though the normal limit is 50mm Hg) and PH below 7.15 when normal PH is 7.35-7.45.
- Shake test is done on gastric aspirate withdrawn from the neonate in the first hour of life.
- Prenatal diagnosis of Respiratory distress syndrome can be made by determining lecithin/ sphingomyelin ratio in amniotic fluid. L/S ratio of more than 2 indicates adequate lung maturity.
Respiratory Distress Syndrome Management:
Respiratory distress is the most common life threatening emergency in premature newborns.
- The principles of management of Respiratory distress syndrome include
- Improving ventilation to enhance oxygenation.
- Correction of acidosis
- Maintenance of thermo neutral environment
- Adequate nutrition
Management of baby with RDS includes:
- Monitoring of the baby’s condition:
- To monitor the baby’s condition, following clinical observations are to be done
- Rectal or skin temperature should be noted hourly
- Hourly monitoring of respiratory rate.
- Noting the severity of retraction and grunting.
- Status of peripheral pulse and B.P.
- Skin color
- Apneic episodes:
- Activity, responsiveness and cry of the baby.
- Urine output. till stable and thereafter every 4 hourly.
- Intravenous infusion:
- Intravenous infusion for maintaining acid-base balance and nutritional status of baby: It is advisable to start intravenous infusion in all the babies with Respiratory distress syndrome because oral feeding may not be possible with the baby as oral feeding has the risk of aspiration.
- The infant needs to be given nasogastric feeding or total parenteral nutrition to prevent tissue catabolism.
- 7.5% soda bicarb should be administered to the baby in dose of 3-8 meq/kg in 24 hours or the dose of soda bicarb may be calculated according to the baby’s PH.
- Ventilatory support:
- Infants with hyaline membrane disease are handicapped by decreased lung compliance and alveolar collapse during expiration.
- Administration of oxygen under positive pressure would prevent alveolar collapse and ensure gas exchange throughout the respiratory cycle. CPAP (Continuous Positive Airway Pressure) is indicated and useful in infants with decreased lung compliance.
- Oxygen via hood
- warmth and humidity.
- Surfactant therapy.
- Antibiotics:
- Administration of antibiotics
Nursing Management:
- Preterm with Respiratory distress syndrome should be prevented from infection by using isolation and aseptic precautions.
- The critically ill infant should be minimally handled
- These infants should be positioned with head elevated, to reduce the pressure on the diaphragm.
- Airway should be kept patent and opened by extending the head slightly. This can be done by placing a folded sheet or towel under the baby’s shoulders.
- As the baby requires oxygen administration for long duration via face mask or nasal prongs, a soothing antibiotic ointment can be applied to irritated skin surface.
- Keep the baby warm by placing the baby in incubator/radiant warmer.
- Monitor vital signs regularly.
- Endotracheal suctioning should be done as required, using strict aseptic techniques.
- Monitor oxygen saturation while suctioning the baby
- Measure baby’s weight daily to assess adequacy of fluid administration.
- Administer intravenous fluids/Nasogastric feed and medications as prescribed by the physician.
Disorders Of The Gastrointestinal System
Question 9. Explain the disorders of the gastrointestinal system
Answer:
1. Congenital Disorders Of Gastrointestinal System:
- Disorders of mouth: Cleft lip and cleft palate
- Disorder of oesophagus: Tracheo- oesophageal fistula
- Disorders of stomach: Pyloric stenosis
- Disorder of intestine: Intestinal obstruction
- Hernia
- Intussusception
- Hirschsprung’s disease
- Anorectal malformation
2. Infection And Infestation Of Gastrointestinal System:
- Diarrhea
- Worm infestation
3. Miscellaneous Disorders:
- Indian childhood cirrhosis
- Fluid and electrolyte crisis
Question 10. Define Cleft lip and cleft palate. Explain the its complications, Surgical management, and Pre and post-operative nursing management Cleft lip and cleft palate.
Answer:
Cleft palate Introduction:
Cleft lip and cleft palate are congenital malformations resulting from the failure of fusion of maxillary processes during intrauterine development. The defect may occur either alone or together.
Cleft palate Definition:
1. Cleft lip (cheiloschisis):
- A cleft lip results from failure of fusion of the maxillary process with nose elevation on frontal prominence.
- The extent of defect varies from a notch in the lip (partial or incomplete cleft) to a large cleft reaching the floor of the nose (complete cleft).
- A cleft lip can occur on one side (unilateral) or maybe on both sides (bilateral).
2. Cleft Palate (Palatoschisis):
- Cleft palate results from failure of fusion of the hard palate with each other and with the soft palate.
- The cleft lip also usually occurs with cleft palate. The cleft palate may be complete (involving hard and soft palate, possibly including a gap in the palate) or incomplete (a ‘hole’ in the roof of the mouth, usually in the soft palate).
Cleft palate Complications:
Cleft lip and cleft palate leads to the following problems:
- Feeding problems: Due to a separation in the lip or opening in the palate, sucking is ineffective and the food and liquids can pass from the mouth back through the nose. There may be aspiration of feeds.
- Respiratory infections: The aspiration of feeds may result in respiratory infections like aspiration pneumonia.
- Ear infections/hearing loss: Children with cleft palate are at an increased risk of ear infections. Usually, middle ear infections occur. If left untreated, may result in hearing loss
- Speech problems: Children with cleft lip or palate may have trouble in speaking. The voice of these children may take a nasal sound and speech may be difficult to understand.
- Dental problems: Children with clefts are more prone to dental cavities and often have missing, extra, malformed or displaced teeth requiring orthodontic treatment.
Cleft palate Management:
A Cleft lip:
- Cleft lip may require one or two surgeries depending on the severity of the defect. The initial surgery is usually performed at the age of 3 months.
- Common procedures for repair of cleft lip are Tennison Randall Triangular Flap (Z-plasty) and Millard’s Rotational Advancement technique.
- Surgeons may also combine these two techniques if needed.
A Cleft palate:
- Cleft palate repair often requires multiple surgeries over the course of 18 years. The first surgical repair usually occurs when the baby is between 6-12 months.
- The initial surgery creates a functional palate, reduces the chance of fluid entering the middle ears and helps in proper development of teeth and facial bones.
- Children with a cleft palate may need a bone graft when they are about 8 years old to fill in the upper gum line so that it can support permanent teeth and stabilize upper jaw.
- About 20% of children with a cleft palate require further surgeries to help improve speech. Once the permanent teeth grow, braces may be put to straighten the teeth.
Nursing Management:
Care of the Baby at Birth:
- Cleft lip and cleft palate is detected immediately after birth, during initial neonatal assessment. Associated, congenital anomalies and life-threatening complications should be identified for prompt management.
- This is a disfiguring defect so soon after birth, the baby looks unattractive. The defect evokes negative reactions and shock in parents. The nurse must explain to the parents about the possibility of defect correction.
- Feeding of the infant with cleft lip and cleft palate is a problem because this defect reduces the infant’s ability to suck.
- Breastfeeding is possible with the use of a palatal prosthesis (Palatal Obturator). If the baby is unable to suck the breast, expressed breast milk may be given using syringe with a rubber tube.
- Expressed breast milk or artificial feeding can also be given with a long-handled spoon or dropper or a soft nipple with a large hole.
- Mother and family members should be demonstrated, the various techniques that can be used for feeding the baby at home.
- Explain to the parents about the risk of aspiration due to cleft palate. So they must be instructed to feed the baby in an upright position.
- Small bolus should be given from the corner of the mouth.
- Give the baby sufficient time to swallow. Small frequent feeds should be given.
- Burp the baby in between the feeds and after feeding. Parents must be explained the importance of adequate nutrition for growth and development of the baby.
- The baby must be given all essential care including immunization, warmth, hygiene, prevention of infection etc.
- Explain about timely follow-up to the parents.
- Care of the Baby before Surgery:
- Basic preoperative care is required. The baby must be prepared according to the surgeon’s orders.
- Consent must be taken prior to surgery.
- All the investigation reports must be entered in the patient’s file.
- The baby must be kept NPO, at least 6 hours prior to surgery.
Care of the Baby after Surgery:
- Immediately after the surgery, closely observe and monitor the vital signs of the baby.
- Observe for any bleeding from the site of surgery.
- Turn the baby’s face to one side, for drainage of secretions and preventing aspiration.
- Most importantly the surgical site is to be protected from any injury, by taking the following measures
- Position the baby on the back or side and arm or elbow restraints are applied to prevent him/her from touching the suture site. These restraints must be periodically removed to exercise the arms.
- An arched metallic device known as ‘Logan’s bow’ must be placed over the upper lip and taped to the infant’s cheeks to prevent tension at the suture line.
- Administer the prescribed analgesic, to minimize pain that causes the baby to cry causing tension on the suture line.
- Prevent infection at the site, by cleaning the operated area gently using aseptic techniques, after each feeding.
- Do not allow the baby to put any object in the mouth, as this may injure the surgical repair.
- Provide love and affection to the baby, as this enhances the feeling of comfort and security in the baby.
Question 11. Define TEF.
Answer:
- Explain the types and clinical features of TEF
- Explain pre and post-operative management of patient with TEF
Answer:
Define TEF:
- Esophageal atresia/tracheoesophageal fistula (EA/TEF) is a condition resulting from abnormal development before birth of the tube that carries food from the mouth to the stomach (the esophagus ).
- Tracheoesophageal fistula is an abnormal connection (fistula) between the esophagus and the trachea. TEF is a common congenital abnormality.
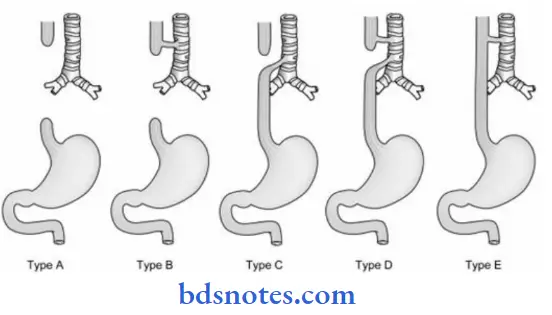
- Enumerates Types of TEF with a diagram.
Classification EA with TEF can be classified as follows:
- Type – 1: EA without fistula (8%): It is the second most common type. There is no connection of the esophagus to trachea. The upper (proximal) segment and lower (distal) segment of the esophagus are blind.
- Type – 2: EA with TEF (upper): It is rare and found in less than 1 percent of all cases. Upper segment of the esophagus open into the trachea by a fistula. The distal or lower segment is blind.
- Type – 3: EA with TEF (lower) (80-90%): It is the most common type. In this condition, the proximal or upper segment of the esophagus has blind end. The distal lower segment of
the esophagus connects to the trachea by a fistula. - Type – 4: EA with TEF both upper and lower segment. It is also rare (less than 1%). There is EA with fistula between both proximal and distal ends of trachea and esophagus.
- Type – 5: H – Type TEF: It is found in about 4 percent of all cases and not usually diagnosed at birth. Both proximal / upper and distal / lower segments of esophagus open into the trachea by a fistula. No EA is present.
TEF Clinical Features:
The presence of maternal polyhydramnios and single umbilical artery should alert the pediatricians and pediatric nurses to look for Atresia of upper digestive tract.
The disorder is usually detected soon after birth when feeding is attempted on the basis of following manifestations:
The violent response occurs on feeding:
- The infant coughs and chokes,
- Fluid returns through the nose and mouth
- Cyanosis occurs
- The infant struggles
- Excessive secretions coming out of the nose and constant drooling of saliva.
- The saliva is frothy.
- Abdominal distension occurs in the presence of type 3, 4, and 5 fistula.
- Intermittent unexplained cyanosis and laryngospasm, caused by aspiration of accumulated saliva in blind oesophageal pouch
- Pneumonia may occur due to the overflow of milk and saliva from the esophagus through the fistula into the lungs.
TEF Management:
Medical Management:
- Immediate management Immediately after diagnosis, the infant should be managed with a propped up position (30 ° angle) to prevent reflux of gastric secretion, and nothing per mouth, airway clearance O2 therapy, IV fluid therapy, nasogastric tube aspiration nasogastric tube to be kept in situ and suctioning to be done frequently to prevent aspiration.
- The blind pouch to be washed with normal saline to prevent blocking of the tube with thick mucus.
- Gastrostomy is done to decompress the stomach and to prevent aspiration and afterward to feed the infant.
- Supportive care should include maintenance of nutritional requirements and warmth, prevention of infections, antibiotics therapy, respiratory support, detection and treatment of complications, continuous monitoring of the patient’s condition, chest physiotherapy, and postural drainage.
Surgical Management:
- The surgical correction of the defect is done by end-to-end anastomosis with excision of the fistula by right posterolateral thoracotomy followed by intercostal chest drainage.
- This is done when the infant has more than 2 kg 6 body weight and no pneumonia present and the baby is clinically stable
- Surgical correction can be done in stages with the division of the fistula. Gastrostomy is performed in the initial stage followed by esophageal anastomosis or colonic transplant after one year.
- This staging is done in small premature or very sick neonates or with other associated congenital anomalies. Other surgical interventions include cervical esophago stomy, esophago Coloplast, and esophago – gastroplasty.
Nursing Management:
- Nursing assessment is very important to detect the condition immediately after birth or at first feed.
- Risk factors to be excluded by details history of the condition.
- Clinical features and problems to be assessed promptly for life – saving measures.
Pre-Operative Nursing Care:
1. Risk of aspiration related to structural abnormality. As soon as the diagnosis of TEF is made, the attempt to feed the baby is stopped.
- A nasogastric tube is put in the upper oesophageal segment and is aspirated frequently, to prevent collection and aspiration of secretions from upper oesophageal segment into the trachea (in case of type II and type IV Fistula).
- Maintain the patency of indwelling nasogastric tube, by frequently irrigating it with normal saline.
- Place the infant in a semi-upright position, to prevent reflux of gastric contents into the trachea (in case of Type 3, 4, and 5 Fistula).
- Constantly observe the child for symptoms of respiratory distress like pallor, cyanosis, choking, nasal flaring etc.
- A gastrostomy tube is placed for gastric decompression, before the definitive surgery.
- Gastric decompression prevents reflux of gastric contents into the trachea (in case of Type 3 and 4 TEF)
- Turn the baby frequently, to prevent atelectasis and pneumonia. Administer the prescribed antibiotics, to prevent and treat pneumonia resulting from aspiration or reflux of gastric contents into the trachea.
2. Risk of deficient fluid volume related to inability to take oral feeds.
- As soon as the diagnosis of TEF is established, oral feedings are stopped.
- Intravenous fluids are administered, as prescribed by the physician.
- Maintain intake and output chart.
- Monitor the hydration status of the infant and look for signs of dehydration.
- A gastrostomy tube may be placed, before definitive surgery to aid in gastric decompression and provide gastrostomy feedings.
3. Impaired breathing related to frequent laryngospasm and excessive secretions in the trachea.
- In case of Type 2 TEF, secretions from the upper blind pouch of the oesophagus may easily enter the trachea leading to laryngospasm and respiratory distress, so frequently suction the upper oesophageal segment.
- Monitor the vital signs of the infant.
- If cyanosis occurs, administer oxygen.
- Keep the infant in semi- upright position.
Post-Operative Nursing Care:
1. Ineffective airway clearance related to disease process:
- A cervical oesophagostomy is made to drain out secretions from upper blind oesophageal pouch, so that the secretions may not overflow and enter the trachea.
- Administer oxygen to the infant.
- Ventilatory support may be provided, until the infant is clinically stable (up to 24-48 hours of surgery).
- Change the infant’s position frequently to prevent the pooling of secretions in the lungs.
2. Impaired nutrition related to surgery:
- Feed the infant orally or by gastrostomy, depending upon the type of surgery done and the infant’s condition
- The gastrostomy is generally attached to gravity drainage for 3 postoperative days, thereafter it is elevated and left open to allow air from the stomach to escape and gastric secretions to pass into the duodenum.
- Gastrostomy feeding is started as soon as ordered.
- Prevent air from entering the stomach during gastrostomy feeding, as it may cause abdominal distension.
- After 10-14 days of surgery, before starting oral feeds, an x-ray is taken, to find out whether anastomosis has healed. When healing has occurred, test feeding is given with glucose water. Slowly oral feeds are started with small amounts of clear fluids and then milk can be started.
3. Altered comfort related to chest tube drainage and surgery:
- Position the baby comfortably in a semi-fowler’s position.
- Administer the prescribed analgesics.
- Provide a calm and quiet environment so that the baby may rest.
- Special care should be taken that the baby may not pull out the nasogastric tube, put in after anastomosis of oesophageal segments.
This may cause injury to the operative site. The baby’s hands should be restrained. - Whenever possible avoid or open the restraints. Somebody should
be there with the baby to hold his hands. - Assess the type of chest drainage present. Report if saliva or blood is present in the drainage
- Keep the drainage system closed to prevent the occurrence of pneumothorax.
- Anxiety related to the disease process and care of the baby after discharge.
- Discharge planning must be done.
- Explain to the parents about routine care, especially feeding the baby.
- Explain about any future surgery, if needed.
- Refer parents to genetic counseling clinics and social welfare agencies that may help them.
Question 12. Hirschsprung‘S Disease and Megacolon
Answer:
Hirschsprung‘S Disease Definition:
Hirschsprung’s disease is a disorder of the gut caused by to congenital absence of ganglion cells in the submucosal and myenteric plexus of the intestine. This disease is also known as Megacolon or Congenital Aganglionic Megacolon
Hirschsprung‘S Disease Pathophysiology:
Hirschsprung’s disease is caused by the congenital absence of autonomic parasympathetic ganglion cells in the submucosal and myenteric plexus of the intestine. In the majority of cases, the disorder affects the short segment of the distal colon.
In 5 % of cases the entire colon is affected:
- Due to the absence of ganglionic cells
- There is a lack of peristalsis in the affected portion
- Functional obstruction of the colon
- Accumulation of gas and feces proximal to the defect
- Enlargement of the colon occurs, so it is also known as Megacolon
Hirschsprung‘S Disease Clinical Features:
The symptoms of congenital megacolon vary from acute obstruction in newborns to chronic constipation in older children
In neonates and infants:
- The initial symptom is failure to pass meconium
- Abdominal distension occurs within 1-2 days after birth
- Bile- stained vomiting occurs because of intestinal obstruction
- Failure to take fluids and vomiting lead to weight loss and dehydration
- Shock may develop , if condition is not treated promptly
- Episodes of diarrhea and constipation occur alternately during infancy
- Enterocolitis may occur due to faecal stagnation
- Enterocolitis may lead to dehydration and sepsis which may cause death of the infant.
In older children:
- Hirschsprung’s disease is manifested by constipation with abdominal distension due to mass of feces and gas
- When stools are passed, they are foul smelling and may be expelled in pellet or ribbon-like form or may be liquid in consistency
- These children are malnourished and anemic due to malabsorption of nutrients
- They have protruding abdomens and thin wasted extremities
Diagnostic Evaluation:
- Hirschsprung’s disease is suspected in a baby who has not passed meconium within 48 hours of birth, Normally, 90 % of babies pass first meconium within 24 hours and 99 % within 48 hours of birth
- On rectal examination of suspected cases, there may be an explosive leakage of gas and accumulated feces
- On palpating the abdomen , fecal mass is felt in the left lower portion of the abdomen
- Definitive diagnosis can be made on the basis of anorectal manometry, barium enema, and rectal biopsy. Rectal biopsy is the gold standard for definitive diagnosis. The biopsy shows absence of ganglion cells in the submucosa
Hirschsprung‘S Disease Management:
Medical Management: Medical management of child having mild chronic symptoms of megacolon include
- Administration of isotonic enema
- Administration of stool softeners
- Low residue diet
Surgical Management:
- The aim of surgery is to remove the aganglionic bowel followed by anastomosis of the remaining portion. The surgery involves two steps. In first stage , a temporary colostomy is done above the transition zone of the ganglionic and aganglionic bowel in the sigmoid or transverse colon.
- This enables the normal distal bowel to return to its original tone and size. The second stage involves definitive surgery, which is done when the child’s weight and condition are appropriate
- Definitive surgery consists of excision of the aganglionic segment with a ’ pull through ‘ procedure enabling an anastomosis to be done between ganglionic colon and anus. The most frequently performed surgeries are those done by Swenson, Soave, Duhamel, and Boley.
- All these procedures vary slightly from each other. After about a year of these corrective surgeries, the colostomy is closed
Nursing Management Pre-operative Nursing Care:
- The first step, to begin the care of an affected newborn is assessment. A complete history of the newborn is taken. The history shows a failure to pass meconium and vomiting. Physical assessment of the baby shows the presence of abdominal distension.
- In the case of older children, the nurse must enquire about the bowel habits of the child, including the age at which constipation started
- After the diagnosis of Hirschsprung’s disease, the nurse must help parents to adjust to their imperfect newborn and foster parents- Infant bonding. The nurse must explain about the disease to the parents
- Parents are taught the procedure of giving isotonic enema, suppositories, and stool softeners
- A low residue diet may be given to the child, to keep the stool small in amount and soft, so that it can be evacuated easily. A soft diet including potato, rice, milk, soup, strained fruit juice, bread etc. must be given to the child
- Vital signs of the child are monitored to obtain baseline data about the child
- Monitor abdominal girth to detect abdominal distension
- Keep the child in semiFowler’s position to facilitate lung expansion and breathing
- Withhold oral feeds and nasogastric aspiration is done on the night before surgery
- Repeated saline enema and bowel wash with antibiotic solution like neomycin is done in case of older children, to prepare the bowel for surgery
- Observe the child for pre-operative complications like shock, acute intestinal obstruction, and bowel. perforation and dehydration
- The nurse observes for shock by monitoring vital signs and blood pressure
- For detecting intestinal obstruction , monitor abdominal girth and observe for the absence of stool, vomiting, abdominal pain, and absence of bowel sounds on auscultation
- Perforation of the intestine results in peritonitis, which is manifested by sudden relief in abdominal pain and then increased generalized pain, increased pulse rate, respiratory rate, and high fever.
- Another complication that may arise is dehydration. The nurse must assess the child properly to detect the severity of dehydration. Dehydration is indicated by reduced urine output , increased thirst, sunken eyes, poor skin turgor etc.
- If any of these complications arise, immediately notify the physician and provide appropriate care in the preoperative period, prepare the child for colostomy and related procedures
Post – Operative Nursing:
- Care Postoperative nursing care includes routine post-abdominal surgery interventions, which are as follows:
- Monitor the vital signs of the child
- Observe abdominal dressing or ostomy bag for bleeding.
- Place the child in a comfortable position according to the physician’s order
- Monitor for abdominal distension
- After surgery the child is NPO, so administer IV fluids as ordered. Maintain fluid and electrolyte balance
- Monitor for return of bowel sounds. As soon as bowel sounds return, start oral feeding
Colostomy care is to be done which includes the following:
- Observe the stoma for its color (normally it is pinkish or reddish-pink in color)
- Observe the stoma for any bleeding, purulent drainage, or edema
- Provide a bland diet to the child, which is non – non-irritating to stoma
- Apply zinc oxide ointment on the skin around the stoma to prevent excoriation of the skin
- Frequently empty the collecting bag applied to the stoma
- Keep the colostomy clean and dry
- Educate parents about colostomy care
- If definitive pull-through surgery is done, the following care needs to be given:
- The incision site is to be prevented from infection. There is a high risk of infection from urine and stool. So, do not put diaper, to observe for passage of urine and stool.
- As soon as the baby passes urine or stool, clean and dry the child
- Meticulous skin care is essential
- IV fluids are given until peristalsis resumes, the baby starts passing stool through the anus, and healing of the anastomosis has taken place
- As soon as bowel sounds return start oral feeds with glucose water and then milk
- Observe for indications of post-operative complications like hemorrhage, shock, abdominal distension, wound infection, peritonitis, enterocolitis, etc. A serious complication of corrective surgery is leakage at the site of anastomosis leading to pelvic abscess, as evidenced by sudden abdominal distension, rise in body temperature to up to 40 ° C, and extreme irritability. If any of these signs and symptoms appear, notify the surgeon immediately
- Advice caregivers that after discharge from hospital provide adequate fluids, dietary fiber and stool softeners or bulk agents to the child in order to achieve normal bowel activity
- Encouraging and supporting the family during this stressful time is the key nursing intervention.
Disorders Of The Cardiovascular System
Question 13. Define congenital heart diseases. Classify congenital heart diseases. Explain about ventricular septal defect
Answer:
Congenital heart disease (CHD) is the structural malformations of the heart or great vessels, present at birth. It is the most common congenital malformations. The exact number of
prevalence is not known.
Congenital heart disease Classification:
Congenital heart disease (CHD) can be grouped into three categories:
1. Acyanotic CHD: There is increased pulmonary blood flow due to left to right shunt.
It includes:
- Ventricular septal defect (VSD)
- Atrial septal defect (ASD)
- Patent ductus arteriosus (PDA)
- Atrioventricular canal (AVC)
2. Cyanotic CHD: There is diminished pulmonary blood flow due to right to left shunt.
It includes:
- Tetralogy of Fallot (TOF)
- Tricuspid atresia (TA)
- Transposition of great arteries (TGA)
- Truncus arteriosus.
- Hypoplastic left heart syndrome.
- Total anomalous pulmonary venous return.
- Eisenmenger syndrome or complex.
3. Obstructive lesions:
- Coarctation of aorta
- Aortic valve stenosis.
- Pulmonary valve stenosis.
- Congenital mitral stenosis.
Ventricular Septal Defect:
- A ventricular septal defect (VSD) is an abnormal opening in the septum between the right and left ventricles. It is the most common cyanotic congenital heart disease with left to right shunt.
- It is found in approximately 25 percent of all CHD. The size of the defect can be small or large. Large VSDs can be restrictive or nonrestrictive type.
- The number of defects can be single or multiple. VSD can be found as perimembranous or muscular
Pathophysiology:
- There is the flow of oxygenated blood from high pressure left ventricle to the low-pressure right ventricle through the VSD. Increased right ventricular and pulmonary arterial pressure leads to pulmonary overcirculation.
- Increased venous return to the left heart results in left heart dilation. Long-standing pulmonary overcirculation causes change in the pulmonary arterial bed resulting increased pulmonary-vascular resistance, which can reverse the shunt from right to left. This complicated condition is known as Eisenmenger’s complex.
- The child with this condition presents with cyanosis and surgical correction of VSDs is not possible in this stage. In the case of a restrictive VSD (under 0.5 cm²), higher pressure in the LV is able to cause only a limited left-to-right shunt.
- In the case of nonrestrictive VSD (large, usually over 1 cm²), the magnitude of the shunt from left to right is, therefore, limited at birth due to higher pulmonary vascular resistance. In the next few weeks, with the reduction in resistance, the shunt magnitude increases. VSD becomes symptomatic when the shunt magnitude becomes quite large.
Congenital heart disease Clinical manifestations:
- Small VSDs are asymptomatic. In large defects, symptoms develop within one to 2 months of age.
- The manifestations are recurrent chest infections, feeding difficulties, tachypnea, exertional dyspnea, pale, delicate looking, tachycardia, excessive sweating associated with feeding, poor weight gain, failure to thrive, hepatomegaly, biventricular hypertrophy, and CCF.
- The characteristic loud pan systolic murmur heard maximal down the left sternal border, usually accompanied by the thrill. A functional diastolic murmur may present.
Diagnostic evaluation:
- History of illness, physical examination, and auscultation of harsh systolic murmur and pulmonary second sound (p₂) are important for diagnosis of the condition.
- Chest X-ray shows enlargement of the heart and increased pulmonary vascular marking. ECG reveals biventricular hypertrophy.
- Two-dimensional echocardiogram with Doppler study and color flow mapping are performed to identify the size, number, site of the defect, and associated problems.
Congenital heart disease Management:
In small VSD, usually, no medical management is required. Surgical repair may be indicated in some cases.
- Prevention of complications is very essential measure.
- Spontaneous closure of VSD occurs in 30 to 50 percent of cases with small defects. In large VSD, initial management of associated problems like CCF and endocarditis should be done with appropriate treatment. Early surgical repair is planned after the management of complications.
- Surgery is done as a one-stage or two-stage operation. One-stage operation with patch closure of VSD by the open-heart method can be performed. A two-stage approach is done with the first stage, to, band the pulmonary artery to restrict pulmonary blood flow by the closed-heart method.
- The second stage operation is done to patch close the VSD and remove the PA band. Surgery is contraindicated in shunt reversal. The long-term prognosis after corrective surgery is excellent.
- Expert nursing management is important during surgical interventions and in complications.
- Long-term follow-up and monitoring of ventricular functions are important measures to promote excellent prognosis.
Congenital heart disease Complications:
- The common complications of VSD are CCF, recurrent respiratory tract infections, infective endocarditis, Eisenmenger’s syndrome, pulmonary stenosis, pulmonary hypertension, and failure to thrive.
- Postoperative complications after thoracic surgery may be life-threatening for the child.
Question 14. Explain the causative predisposing factors for acute rheumatic fever.
Answer:
Rheumatic fever is an immunological disorder initiated by group A beta-hemolytic streptococcus.
It is a systemic inflammatory disease of childhood that can involve the heart, joints, central nervous system, skin, and connective tissues.
Risk factors:
Things that may increase the risk of rheumatic fever include:
- Genes: Some people have one or more genes that might make them more likely to develop rheumatic fever.
- Specific type of strep bacteria: Certain strains of strep bacteria are more likely to contribute to rheumatic fever than are other strains.
- Environmental factors: A greater risk of rheumatic fever is associated with overcrowding, poor sanitation, and other conditions that can cause strep bacteria to easily spread among many people.
- Rheumatic fever is caused by a bacterium called group A Streptococcus. This bacterium causes strep throat or, in a small percentage of people, scarlet fever. It’s an inflammatory disorder.
- Rheumatic fever causes the body to attack its own tissues. This reaction causes widespread inflammation throughout the body, which is the basis for all symptoms of rheumatic fever.
Question 15. Jones criteria for Rheumatic fever
Answer:
Rheumatic fever:
Rheumatic fever is an immunological disorder initiated by group A beta-hemolytic streptococcus.
- It is a systemic inflammatory disease of childhood that can involve the heart, joints, central nervous system, skin, and connective tissues.
- The diagnosis of ARF can be made by applying the modified (1992) Jones criteria. Diagnosis requires evidence of recent streptococcal infection and 2 major criteria, or 1 major and 2 minor criteria.
Rheumatic fever Major Criteria:
- Polyarthritis: Migrating arthritis that typically affects the knees, ankles, elbows, and wrists. The joints are very painful and symptoms are very responsive to anti inflammatory medicines.
- Carditis: All layers of cardiac tissue are affected (pericardium, epicardium, myocardium, endocardium). The patient may have a new or changing murmur, with mitral regurgitation being the most common followed by aortic insufficiency.
- Chorea: Also known as Syndenham’s chorea, or “St. Vitus’ dance.” Chorea consists of abrupt, purposeless, jerky, uncoordinated movements, especially affecting the hands, feet, tongue, and face. This may be the ONLY manifestation of ARF.
- Erythema marginatum: A non-pruritic rash that commonly affects the trunk and proximal extremities, but spares the face. The rash typically migrates from cen tral areas to periphery, forming a snakelike ring while clearing in the middle and having well-defined borders. This rash is made worse with heat.
- Subcutaneous nodules (a form of Aschoff bodies): Small non-tender, firm collections of collagen fibers on the back of the wrist, the outside elbow, and the front of the knees. These now occur infrequently.
An additional way to remember the major criteria is by the mnemonic:
Cancer:
- C: Carditis
- A: Arthritis
- N: Nodules (subcutaneous)
- C: Chorea
- ER: Erythema Marginatum
Cancer Minor Criteria:
- Arthralgia: Pain on joint movement without evidence of swelling or heat
- Fever
- Previous ARF or rheumatic heart disease
- Leukocytosis, elevated ESR, and CRP
- Prolonged P – R interval on ECG
Cancer Management:
- Bedrest is important in the management of children with rheumatic fever. It is needed for at least 6 to 8 weeks till the rheumatic activity is disappeared.
- A nutritious diet to be provided with sufficient amounts of protein, vitamins, and micronutrients.
- Salt restriction is not necessary unless CCF is present. Avoid rich spicy food.
- Antibiotic therapy, penicillin is administered after a skin test to eradicate streptococcal infection. Initially, procaine penicillin 4 lacks units deep IM, twice a day is given for 10 to 14 days. Then the long-acting benzathine penicillin 1.2 mega units every 21 days or 0.6 mega unit every 15 days to be given.
- Oral penicillin 4 lakhs units (250 mg), every 4 to 6 hours for 10 to 14
days can be also given. Erythromycin can be used in penicillin-sensitive patients. - Aspirin is administered as suppressive therapy to control pain and inflammation of joints.
- The dose of aspirin is 90 to 120 mg/kg/day in 4 divided doses. It may be needed for 12 weeks.
- The dose can be modified for the individual patients. Aspirin should not be given in an empty stomach. Antacid to be given just prior to or with the aspirin.
- Steroid (prednisolone) therapy is given as suppressive therapy along with aspirin. The initial dose is 40 to 60 mg/ day or 2 mg/kg/day in 4 divided doses, for 7 to 10 days. Then the dose is reduced to 1 mg/kg/day.
- It should be tapered off gradually over 12 12-week periods and used for patients having carditis with or without CCF.
- Management of chorea can be done with diazepam or phenobarbitone.
- Treatment of complications, if present, especially for CCF should be done. Symptomatic care to be provided accordingly.
Nursing Management:
Nursing assessment is vital for the care of a child with rheumatic fever. It should include special attention to vital signs, cardiac monitoring (ECG, heart sound), pain assessment and other associated problems.
Important nursing diagnoses are:
- Decreased Cardiac Output Related To Carditis
- Pain Related To Polyarthritis
- Risk of injury related to involuntary movements in chorea,
- Anxiety Related To Disease Process,
- Knowledge deficit related to long-term treatment and prognosis of the acquired heart disease.
Nursing Interventions: Nursing interventions should emphasize the following along with routine care:
Improving cardiac output by:
- Providing rest as long as rheumatic activity and heart failure persist. In milder cases, light indoor activity is allowed.
- Organizing nursing care with uninterrupted rest and modifying activities.
- maintaining normal body temperature by managing fever.
- Providing a bland diet with adequate nutrition and fluid intake with salt restriction in case of CCF.
- Administering medication as prescribed with necessary precautions.
- Monitoring cardiac functions, intake-output, and features of improvement or deterioration.
Relieving pain by:
- Administering anti-inflammatory analgesics as prescribed and assessing features of aspirin toxicity.
- Providing comfortable position and support to the inflamed joints.
- Arranging diversional activities and play materials according to the age and choice of the child.
Protecting the child from injury by:
- Removing hard and sharp objects from the child’s reach.
- Assisting the child in feeding, ambulation, and other fine motor activities and channelization of the stress.
- Administration of drugs to control the chorea.
- Explaining about self-limiting course of the condition and the importance of physical and mental rest. health teaching for maintenance of health and prevention of Complications:
- Explaining the duration of treatment, its importance and compliance, activity restriction, follow-up, continuation of school performance, and improvement of living standard.
- Instructing about preventive measures.
Disorders Of Hematological Systems
Question 16. Define anemia, Enumerate the causes of the anemia, and enumerate the nursing management of anemia.
Anemia:
Anemia is the most common blood disorder in infants and children, especially in poor socioeconomic groups. Anemia is defined as the reduction in the number and quality of circulating red blood cells when the hemoglobin content is below the normal level for a particular age, resulting in decreased oxygen-carrying capacity.
World Health Organization (WHO) proposed the cut-off points of Hb level for different age groups for the diagnosis of
- Children 6 months to 6 years – 11 g/dL
- Children 6 years to 14 years – 12 g/dL
- Above 14 years
- Male – 13 g/dL
- Female -1 2 g/dL
- Mild anemia (10.0-10.9 g/dL) – 26.3 percent
- Moderate anemia (7.0-9.9 g/dL) – 40.2 percent
- Severe anemia (less than 7 g/dL) – 2.9 percent
- Any anemia (Hb level less than 11 g/dL) is found in 69.5 percent of children.
Anemia Causes:
- Red blood cells (RBCs) and hemoglobin are normally formed and destroyed at the same rate.
- But when the formation of RBC and hemoglobin is decreased and their destruction is increased then anemia develops. The oxygen-carrying capacity and CO2-removing capacity are decreased.
- There are various causes of anemia but in some cases, causes can be idiopathic.
Impaired of RBC production:
Impaired RBC production due to deficiency of hemopoietic factors in nutritional deficiency (nutritional anemia)
The most common nutritional anemia is iron deficiency anemia:
Other nutritional deficiency conditions causing anemia are folic acid deficiency, vitamin B12 deficiency, vitamin B deficiency, and vitamin C deficiency.
Increased destruction of RBCs (hemolytic anemia):
1. Hemolysis due to intrinsic factors:
- Abnormal hemoglobin synthesis-thalassemia, sickle cell disease Causes of anemia can be described as follows:
- Enzymatic defect-Glucose-6-phosphate-dehy drogenase deficiency.
- Abnormalities in RBC membrane or structural defects of RBC-Hereditary spherocytosis.
Hemolysis due to extrinsic factors:
- Infections-malaria, kala-azar.
- Antibody reaction-Rh or ABO isoimmunization, autoimmune hemolytic anemia, lupus.
- Drugs-Primaquine, phenacetin, phenytoin.
- Poisoning-Lead.
- Burns
- Splenomegaly.
Increased blood loss:
- Acute trauma, epistaxis, bleeding diathesis (leukemia, purpura, hemophilia), hemorrhagic
- disease of newborn, and scurvy. blood loss (hemorrhagic anemia) chronic hookworms, bleeding piles, chronic dysentery, esophageal varices.
Decreased RBC production (bone marrow depression):
- Primary-Hypoplasia or aplasia, Fanconi anemia.
- Secondary-Irradiation, infections, chronic illness like nephritis, leukemia and other neoplastic diseases, tuberculosis, liver disease, hypothyroidism, and drug therapy (chloramphenicol, sulfa)
Anemia Clinical Manifestations:
- The early symptoms of anemia are fatigue, listlessness, and anorexia. Late symptoms may include pallor (skin, nail bed, mucous membrane), weakness, vertigo, headache, malaise, and drowsiness.
- Other features are sore tongue, gastrointestinal problems, tachypnea, shortness of breath on exertion, tachycardia, palpitations, etc. Jaundice, petechiae, and ecchymosis may present in some cases.
- Hepatomegaly may be an associated feature in hemoglobinopathies and liver disorders.
- Enlarged lymph glands may be found in leukemia, infections, malignancy, and myeloproliferative disorders.
Anemia Management:
- Medical management of anemia depends upon the specific cause of the condition.
- Anemia due to excessive blood loss should be treated accordingly. Acute blood loss needs immediate control of bleeding and to restore blood volume by IV infusion, and blood transfusion along with treatment of shock and the cause of bleeding.
- Chronic blood loss usually produces iron deficiency anemia. The exact cause should be detected and treatment should be planned according to the specific cause.
- Anemia due to excessive blood cell destruction requires the identification and treatment of specific hemolytic disorders.
- Anemia due to decreased blood cell formation is mainly due to deficiency states and bone marrow disorders. Specific deficiency of iron, folic acid, vitamin B12, etc should be detected and treatment to be done with replacement therapy of specific nutrients.
- In case of bone marrow depression, the specific cause (like drugs, toxins) is to be identified and treatment is to be performed by removal of offending agents.
Nursing Management:
- Nursing assessment is the cornerstone of nursing interventions. It is done by obtaining a details history to detect potential causes of the condition.
- History of present complaints, past illness, chronic diseases, presence of infections, worm infestations, exposure to medications, poisons, dietary habits, behavioral problems like pica, and history of familial diseases are important aspects of assessment.
- Physical examination to be done to exclude the presence of clinical features like pallor of skin and mucous membrane with other signs and symptoms related to anemia.
- Assessment of anthropometric data (height, weight, MUAC, skin fold thickness, head, and chest circumference), vital signs, and review of laboratory investigations are important to identify the problems and to implement the care
Question 17. Define thalassemia, Explain the clinical manifestation and Medical management of the Thalassemia. Nursing diagnosis with interventions.
Answer:
- A thalassemia is a group of hereditary hemolytic anemia characterized by a reduction in the synthesis of hemoglobin.
- It produces hypochromic microcytic anemia due to defective hemoglobinization of RBCs, hemolysis, and ineffective erythropoiesis.
- Thalassemia can be considered as hemolytic and hyperproliferative anemia related to abnormal hemoglobin.
Thalassemia Clinical Manifestations:
- Thalassemia r usually manifests at the age of 3 months with progressive pallor, jaundice, hepatosplenomegaly, recurrent respiratory infections, enlargement of lymph nodes, and growth failure.
- In severe cases, facial appearance becomes mongoloid and characterized by bossing of the skull, prominent frontal and parietal eminences with flat vault, and straight forehead.
- Maxilla becomes prominent with exposure to malformed teeth. The bridge of the nose becomes depressed with puffy eyes.
- Anorexia, poor feeding, and abdominal distension may present. Irregular fever may occur due to intercurrent infections, and increased metabolic activity.
- Increased pigmentation of the skin is found as bronze discoloration due to high levels of melanin and hemosiderin.
- Hypogonadism, and poor nutritional status with reduced activity level are common findings.
- Marked growth retardation is observed. Skeletal changes are marked and pathological fracture may occur due to osteoporosis.
Thalassemia Management:
Repeated Blood Transfusion
- It is given at regular intervals to maintain a hemoglobin level of at least 10 to 11 g/dL. The interval and amount of blood transfusion depends upon the level of hemoglobin of the child.
- Usually, 10 to 15 mL/kg every 2 to 3 weeks washed packed RBCs are transfused. Special precautions are to be taken during transfusion to prevent complications.
Iron Chelation Therapy:
- Iron chelating agent desferrioxamine (Desferal) is recommended to prevent complications of repeated blood transfusions, i.e. hemosiderosis and hemochromatosis.
- It is given as a continuous subcutaneous infusion in the dose of 25 to 50 mg/kg/day over 8 hours to 12 hours.
Splenectomy:
Splenectomy is indicated when the child needs a very frequent blood transfusion and develops hypersplenism or a big spleen causing discomfort.
Folic Acid Supplementations:
Folic acid supplementations are recommended whereas iron therapy and dietary iron should be avoided to prevent more iron deposition.
Supportive Management:
- Supportive management is important to manage associated problems and to treat complications (like CCF, and hepatic failure). Vaccination with hepatitis ‘B’ to be given to prevent transfusion-related infection along with other routine immunizations.
- Emotional support is very essential to the parents and child. Basic supportive nursing care is very important to prevent various complications.
Bone Marrow Transplantation:
- Bone marrow transplantation is an effective treatment modality with the potential to cure thalassemia.
- Defective stem cells are replaced by normal stem cells. It is extremely expensive and possible in only very selective cases.
New Approaches:
- New approaches in the management of thalassemia are gene therapy and gene manipulation.
- In gene therapy, the insertion of normal genes is done in the stem cells to correct the underlying defect.
- It is done in two approaches, i.e. somatic and transgenic. In gene manipulation, the excess of alpha chains is decreased by increasing the gamma chains.
Nursing Management:
Nursing assessment should be done based on subjective and objective data to formulate the nursing diagnoses for the particular child and to implement the nursing interventions.
The important nursing diagnoses for a thalassemic child are as follows:
- Altered tissue perfusion related to abnormal hemoglobin.
- Risk of infection related to anemia.
- Activity intolerance related to anemia, CCF, etc.
- Chronic pain related to skeletal changes.
- Body image disturbances related the bony changes and facial deformities.
- Ineffective family coping related to poor prognosis.
- Knowledge deficit related to child care in long-term chronic illness with hemolytic anemia.
Nursing Interventions:
- Nursing interventions should be emphasized on the following aspects: Assessment of the child’s condition to prevent complications that can be done at a hospital-based or community-based home).
- Preparation for repeated hospitalization for treatment of the disease and its complications. (at home )
- Arrangement of necessary diagnostic measures.
- Administration of blood transfusion and iron chelating agent with appropriate precautions for specific therapy.
- Provision of supportive care with rest, comfort, nutritious diet with restriction of iron-containing food. Vitamin supplementation, immunization, hygienic care, and other symptomatic care.
- Prevention of infection by aseptic techniques and promotion of general cleanliness.
- Preoperative and postoperative care during splenectomy with necessary health education after the surgery.
- Information regarding treatment plans, prognoses, and complications is to be given to parents and family members with appropriate explanations.
- Emotional support to the parents and family for effective coping with the stress of the illness.
- Teaching the parent about the importance of follow-up, blood transfusion, investigations, signs of complications, dietary restriction, activity modification, recreation, diversion, and available treatment facilities.
- Referral and necessary guidance for available support services and community facilities.
Question 18. Define leukemia and describe the Clinical Manifestations, Pathophysiology, and medical and Nursing management of leukemia.
Answer:
Leukemia:
Leukemia is the most common type of childhood malignancy characterized by persistent and uncontrolled production of immature and abnormal white blood cells. It is a disease of abnormal proliferation and maturation of bone marrow which interferes with the production of normal RBCs, WBCs, and platelets.
Leukemia Clinical Manifestations:
- Clinical presentations of leukemia depend upon the types of leukemic cells. The onset is usually acute or insidious.
- The ALL is a great imitator with vague and varied signs and symptoms, resembling almost any disease.
- The initial manifestations are fever anorexia, malaise, weakness, petechiae, purpura, ecchymosis, and bleeding. The child may present with progressive pallor, decreased activity level, weight loss, and muscle wasting.
- The child may complain of abdominal pain, bone pain, joint pain, and sternal tenderness.
- Hepatosplenomegaly, hematemesis, melena, hematuria, and oral infections are common associated features.
- Excessive bleeding from nose pricks minor injury or minor operations like tooth extraction may be the first alarming features.
- Rarely lymphadenopathy may be found in T-cell ALL or leukemic transformation of lymphoma.
- Central nervous system (CNS) involvement or meningeal leukemia may be manifested with headache, vomiting, drowsiness, unconsciousness, convulsions, cranial nerve involvement, papilledema, and blurred or double vision.
Leukemia Management:
Effective treatment is available for leukemia. It includes chemotherapy, radiation therapy, and bone marrow transplantation.
Nursing Management of a Child with Leukemia:
- Nursing assessment should be done based on subjective and objective data. The important nursing diagnoses are:
- Anxiety of the parent related to diagnosis of malignant disease.
- Risk for infections and bleeding related to abnormal bone marrow functions.
- Pain related to infiltration of leukemic cells.
- Activity intolerance related to fatigue resulting from disease process.
- Alternation of body temperature, more than normal due to infections.
- Altered nutrition, less than body requirement related to anorexia, nausea, and gingival ulcers.
Nursing Interventions:
- Providing emotional support to the parent to reduce parental anxiety. Encouraging the parents to express their feelings and answer their questions honestly. Necessary information and instructions to be given to the parents and family members to avail support services, community resources, and religious help to adjust to the stressful situation.
- Preventing infections and hemorrhage. The following measures to be followed
- Maintaining aseptic technique, hygienic measures, general cleanliness, good handwashing practices, restriction of visitors, and taking precautions during any invasive procedures.
- Administering antibiotics, as prescribed. Oral and IV routes are to be used. Intramuscular injection should be best avoided.
- Precautions to be taken during blood transfusion.
- Avoiding injury. Soft toothbrushes can be used for dental care.
- Soft jelly is to be applied for dry lips. Nonirritating mouthwash is to be used, no alcohol or H2O2 is to be used. Breaking of skin
and mucous membranes is to be avoided. - Monitoring vital signs, urinary output, hydration level, signs of infections, bleeding, or any other complications.
- Relieving pain by rest, comfort, minimizing exertion, promoting relaxation and diversion, and administering prescribed analgesics.
- Assisting in the activity of daily living (ADL), promoting hygienic care, and minimizing disturbance during nursing interventions by gentle approach.
- Maintaining normal body temperature by tepid sponge in high fever, airy environment, adequate fluid intake, avoiding overclothing and hot environment, and administering antipyretics and other prescribed drugs. Recording vital signs 4 hourly. Avoiding the use of a rectal thermometer.
- Promoting adequate nutritional intake with a highly nutritious diet with small frequent feed.
- Avoiding high salty food, when steroids are given. Antiemetics is to be given to prevent vomiting.
- The diet should be attractive and tasty to promote intake of more amount.
- Explaining the change in body image, especially in the case of alopecia due to chemotherapy. Ensuring future change and contacting people having new hair following alopecia.
- Reducing fear of the children by allowing parents with them during procedures, improving IPR, and allowing play materials.
- Teaching the parents about health maintenance regarding regular blood testing, chemotherapy or other mode of management, possible complications and their warning signs, necessary medical help, and follow-up.
Disorders Of Kidney And Urinary Track
Question 19. Epispadias
Answer:
Epispadias is the congenital abnormal urethral opening on the dorsal aspect of the penis.
The urethra is displaced dorsally due to abnormal development of the infra umbilical wall and the upper wall of the urethra. It is usually associated with exstrophy of the bladder and ambiguous genitalia. Rarely it may be found in female infants.
Epispadias Classification:
Epispadias in male children can be classified as:
- Anterior epispadias with normal continence
- Glandular
- Balanitis or penile.
- Posterior epispadias-associated bladder neck and incontinence of urine
- Penopubic
- Subsymphyseal
- The male infants with epispadias are having short and broad penis with dorsal curvature.
- In females, a cleft extends along the roof or entire urethra, involving the bladder neck.
- The urethra is short and patulous.
Female epispadias can be classified as:
- Bifid clitoris with no incontinence of urine. Subsymphyseal with incontinence of urine.
- In both males and females, pubic bones are usually found separated, along with epispadias.
Epispadias Management:
- Management of epispadias is done by surgical correction usually in three stages.
- The first stage operation is done in about 1.5 to 2 years of age for penile lengthening, elongation of the urethral strip, and chordee correction.
- The second stage operation is done at least 6 months after the first stage for urethral reconstruction.
- Third-stage operation is done at about 3 to 4 years of age for bladder neck reconstruction and correction of VUR. Cystoplasty can be done to enhance the bladder capacity after 2 to 3 years of 3rd stage operation.
- Supportive nursing care should emphasize on prevention of infections, emotional support for long-term management schedules, and routine preoperative and postoperative management.
- Health maintenance and promotion of growth and development should be emphasized by a balanced diet, immunization, hygienic measures, and parental guidance.
Question 20. Hypospadias
Answer:
Hypospadias:
- Hypospadias is the congenital abnormal urethral opening on the ventral aspect (under surface) of the penis.
- It is one of the most common malformations of male children. Undescended testes inguinal hernia or upper urinary tract anomalies may be associated with hypospadias
- It may be found in females as a urethral opening in the vagina with dribbling of urine.
Hypospadias Classification:
Hypospadias can be classified depending on the site of the urethral meatus.
- Anterior hypospadias (65-70%): It may be found as glandular or coronal or on the distal penile shaft. Middle (10-15%) penile shaft hypospadias.
- Posterior hypospadias (20%): It may be found on the proximal penile shaft or as a penoscrotal, scrotal, or perineal type.
Problems Related to Hypospadias
A child with hypospadias may have the following problems:
- Presence of painful downward curvature of the penis during erection as chordee.
- Due to chordee, there is a deflected stream of urine and the child wets his thigh during urination.
- Inability to void urine while standing, in case of penoscrotal, scrotal, and perineal hypospadias. It also may be found with the penis in the normal elevated position.
- If appropriate management is not done or left untreated, the condition, in later life, interferes during sexual intercourse with difficulty in penetration due to the presence of chordee.
- Severe forms of hypospadias interfere with reproductive ability as the sperms are deposited outside the vagina due to the proximal situation of the meatus.
- There can be meatal stenosis, fistula, urethral stricture or stenosis, or diverticulum.
Hypospadias Management:
- Management of hypospadias is done by surgical reconstruction to obtain a straight penis at erection, to form a urethral tube and urethral meatus at the tip of the glans penis. Meatotomy is done at any age after birth.
- Chordee correction and advancement of prepuce can be done at the age of 2 to 3 years.
- Urethroplasty is done 3 to 4 months after chordee correction. The surgical repair should be completed before admission to the school. The operation can be performed as a multistage or single-stage repair.
Question 21. Wilms‘Tumor (Nephroblastoma)
Answer:
Wilms‘Tumor:
- Max Wilms, a German surgeon described this most common renal tumor of childhood. It is associated with chromosome deletions, especially from chromosomes 11 and 16.
- Wilms’ tumor is a rapidly developing highly malignant embryonal tumor usually diagnosed within 3 years of age. It is generally unilateral and can be familial in some cases. It may be associated with other congenital anomalies, like hemihypertrophy of the vertebrae, genitourinary anomalies, aniridia, ambiguous genitalia, etc.
- This tumor develops within the kidney parenchyma, distorting it and invading the surrounding tissues. The tumor tends to grow in a concentric fashion invading the adjacent renal parenchyma.
- Characteristically a well-developed capsule is present.
Hemorrhage, necrosis, and calcification may occur rarely. - Metastatic spread occurs by lymphatics to the renal hilar, periaortic, and pericaval lymph nodes.
- Distant blood-borne metastasis occurs most frequently in the lungs, bone, and liver.
Wilms‘Tumor Clinical Manifestations:
- The majority of the affected children present with an asymptomatic abdominal mass, detected during routine examination or by the mother during daily baths or undressing the child. Increasing abdominal girth is an important finding.
- Microscopic hematuria, pain abdomen, fever, pallor, hypertension, and superficial venous engorgement may present. Gross hematuria indicates advanced Stage III or Stage IV tumors.
- On examination large, smooth, fixed, firmed, nontender palpable mass was detected in the flank.
Wilms‘Tumor Clinical Features:
- Wilm’s tumor is asymptomatic in early stages:
- The most common presenting feature of Wilm’s tumor is the presence of an abdominal mass or an enlarging abdomen.
- The mass is discovered accidentally by parents during diaper changing or bathing the baby or may be detected when the child complains of abdominal discomfort.
- Other features include Pain if the tumor is rapidly enlarging or due to hemorrhage, necrosis, or invasion of neighboring structures.
- Urethral obstruction, if the tumor is large, may lead to urinary infection.
- Anorexia
- Hematuria High blood pressure Increased growth on only one side of the body
- Nausea and vomiting
Wilms‘ Tumor Clinical Staging :
This staging helps to determine the prognosis and survival of the patients.
- Stage 1: Tumor limited to the kidney and can be fully excised. The renal capsule is intact. The tumor was not ruptured and no residual tumor after excision.
- Stage 2: The tumor extends beyond the kidney but can be completely excised. There is a regional extension of the tumor by penetration through the renal capsule. Vessels outside the kidney are either infiltrated or contain tumor thrombus. No residual tumor is apparent beyond the margins of resection.
- Stage 3: Residual nonhematogenous extension of the tumor confined to the abdomen following surgery. Involvement of hilar, periaortic, or other lymph nodes may present. The tumor cannot be completely resectable because of local infiltration into the vital structure.
- Stage 4: Hematogenous metastasis to distant organs, i.e. lungs, liver, brain, etc.
- Stage 5: Bilateral renal involvement which occurs in 5 to 8 percent of the cases.
Wilms‘ Tumor Management:
- Management of Wilm’s tumor depends upon histological findings, clinical staging, and metastasis.
- Stage 1 and 2 Wilm’s tumors with favorable histology are usually managed with nephrectomy and chemotherapy for 18 weeks.
- Stage 3, 4, and 5 tumors are treated with nephrectomy, abdominal radiotherapy, and chemotherapy for 24 weeks. Preoperative radiotherapy and chemotherapy are indicated in massive tumors.
- Chemotherapy is usually administered with vincristine, dactinomycin, actinomycin, adriamycin, doxorubicin, and cyclophosphamide.
- Radiotherapy is not given to children below one year of age. Nursing management should include special care during nephrectomy, radiotherapy, and chemotherapy.
- Reducing the anxiety of the parents, through explanation, involvement in child care, and teaching long-term home-based care are important nursing interventions to help the family cope with the situation.
Question 22. Define nephrotic syndrome, Explain the Causes, and pathophysiology of nephritic syndrome, and Explain the nursing management.
Nephrotic Syndrome Introduction:
The nephrotic syndrome is a clinical state characterized by proteinuria, hypoalbuminemia, hyperlipidemia, and edema, sometimes accompanied by hematuria, hypertension, and reduced glomerular filtration rate.
Nephrotic syndrome Definition:
- Nephrotic syndrome is a clinical manifestation of a large number of glomerular disorders. It is characterized by massive proteinuria, hypoalbuminemia, hyperlipidemia, and edema which is generalized and also known as anasarca or dropsy.
- Primary causes of nephrotic syndrome are usually described by the histology. i.e. minimal change disease (MCD) like minimal change nephropathy which is the most common cause of nephrotic syndrome in children, and focal segmental glomerulosclerosis which is the most common cause of nephrotic syndrome in adults.
- When it is due to systemic disease, it is termed secondary nephrotic syndrome.
Nephrotic syndrome Causes:
1. Primary renal causes: Minimal change nephropathy
- Glomerulosclerosis
- Acute post-streptococcal glomerulonephritis
- Immune complex glomerulonephritis
2. Systemic causes:
- Infections
- Toxins- Mercury, Bismuth,
- Gold Allergies- Bee sting, Serum sickness,
- Inhaled pollen, Food allergy.
- Cardiovascular-sickle cell disease, Renal vein thrombosis, Congestive Heart Failure
- Malignancies- Leukemia
- Others-Amyloidosis, Systemic Lupus Erythematous, Anaphylactic purpura
Nephrotic syndrome Pathophysiology:
- Due to any pathological condition, there is alteration in the glomerular basement membrane which increases the glomerular permeability to plasma proteins. Proteinuria occurs and plasma proteins decrease.
- The colloidal osmotic pressure which holds water in blood vessels is decreased due to a decreased amount of serum albumin.
- This allows fluids to flow from capillaries into the tissues.
- Thus vascular volume decreases which stimulates the secretion of aldosterone from adrenals thereby leading to retention of sodium and water, leading to increasing edema.
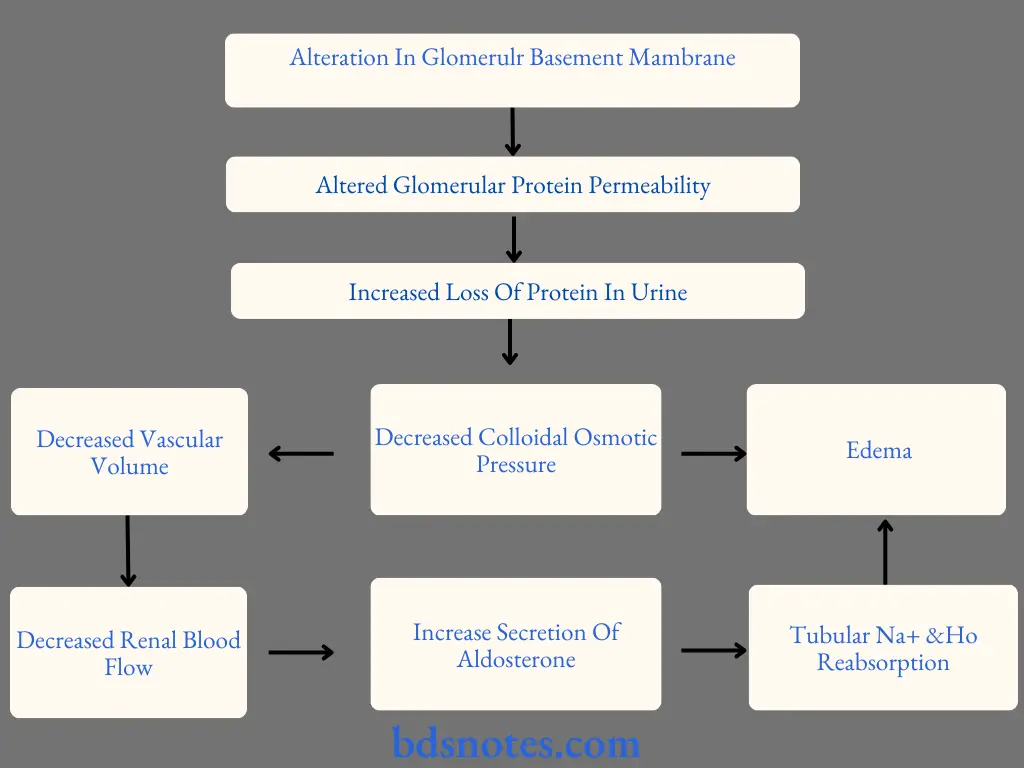
Nephrotic syndrome Clinical Manifestations:
- The onset is slow. Features of nephrotic syndrome include:
- Edema around eyes, legs, and labia
- Anasarca (generalized body edema)
- Ascites
- Hydrothorax and hydrocele
- Decrease urine output, urine appears to be frothy and has increased specific gravity
- Hematuria
- Fever, rash, and joint pain
- Pallor
- Irritability
- Loss of appetite but weight gain
- Susceptibility to infections.
Nephrotic Syndrome Nursing Management:
1. Care during Hospitalization:
- The child is hospitalized for initial therapy. Parents may not understand the importance of hospitalization because initially, the child is symptomless. During hospitalization, parents should be involved in child care and goal setting.
- Nurses should regularly monitor the vital signs and check the child’s daily weight.
- Monitor signs of infection and edema.
- Detailed charting of intake/output must be done to monitor the child’s response to medical therapy.
- A daily urine examination for albumin is required.
2. Administer the prescribed Medications:
- Children with nephrotic syndrome are receiving steroids so the nurse must be aware of the side effects of these drugs.
- Patients should be observed for gastrointestinal bleeding, gastrointestinal ulcers, hyperglycemia, and cataracts.
- Steroid is continued till the child is protein-free, thereafter the drug dose is decreased gradually.
3. Maintain fluid and electrolyte balance:
The nurse should monitor the serum sodium level of the child. Fluid intake either Oral/IV should be strictly monitored. The child is assessed for venous stasis, ascites and pulmonary edema.
4. Prevention of infection:
The child is on corticosteroid therapy (immunosuppressant) and there is a loss of immunoglobulin in urine, so these children are at greater risk of infection. Strict aseptic techniques should be used during invasive procedures. Monitor vital signs to detect early signs of infection,
5. Promote Rest:
- Provide passive play to the child as tolerated. E.g. watching reading story books etc.
- Allow a period of rest after activities. Limit visitors during the acute phase of illness.
Nephrotic syndrome Provide Emotional Support:
- Explain to parents about the disease and its treatment. Allow the parents and child to express their feelings.
- Due to sudden weight gain and disturbed body image, the child may manifest behavioral changes, may refuse to look at the mirror, and have decreased interest in appearance.
- Enhance the body image of the child. Encourage the child to wear their clothes rather than hospital clothes as this makes the child feel good.
Discharge Planning and Home Care Teaching:
Explain to parents about the treatment program, follow-up, and risk of relapse.
Question 23.
- Define Acute glomerulonephritis.
- Explain the Pathophysiology and clinical features of acute glomerulonephritis
- Complications and nursing care plan of acute glomerulonephritis
Answer:
Glomerulonephritis Definition: Acute glomerulonephritis is an acute or sudden inflammation of glomeruli within the kidneys. This inflammation results in acute renal failure.
Glomerulonephritis Etiology: The etiologic agent is usually a bacteria or virus. The most common organism is Beta Hemolytic streptococcus. The primary site or infection is usually the throat or the skin, after which nephritis occurs.
Glomerulonephritis Pathophysiology:
- On infection with Beta hemolytic streptococcus, it invades the child’s system.
- The immune system responds by producing antibodies that fight the infectious agents or antigens.
- The antigen and antibody complex forms, which get deposited in the renal glomeruli
- This leads to inflammation of glours leading to edema and hypertension.
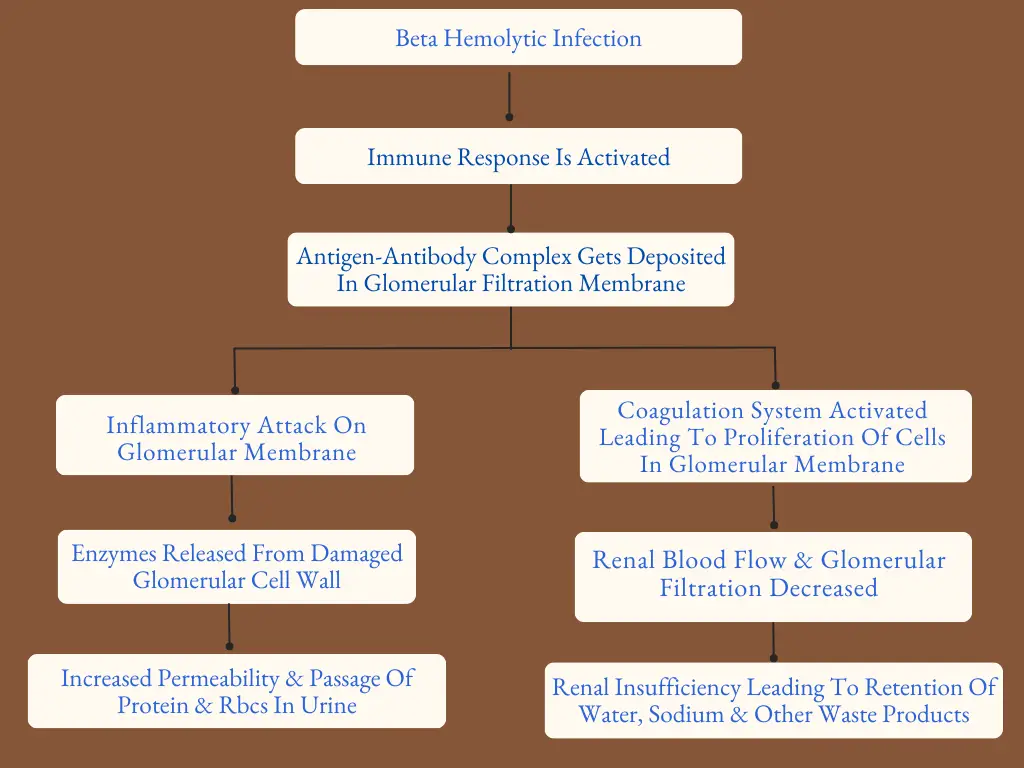
Glomerulonephritis Clinical Features:
The onset of glomerulonephritis is sudden or acute.
The clinical features are as:
- Hematuria
- Oliguria Tea-coloured urine due to hematuria
- Periorbital edema
- Anasarca.
- Hypertension (very common and occurs in over half of the patients)
- A minimal pain
- Fever
- Fatigue and lethargy
Glomerulonephritis Management:
The aims of management are
- To identify and treat the source of infection.
- To maintain fluid and electrolyte balance.
- To maintain blood pressure within normal range.
For the achievement of these aims, the following needs to be done:
A detailed history and thorough physical examination is essential to find out the primary site of infection.
- Children with normal blood pressure and urine output can be managed at home with the administration of prescribed antibiotics.
- Children with generalized edema, hematuria, and hypertension need to be hospitalized because of the probability of developing acute renal failure. The child should be given complete rest during acute phase.
- Hypertension needs to be treated with antihypertensive like Hydralazine and Methyldopa.
- Generalized edema requires the administration of diuretics like Frusemide (Lasix) in a dose of 1-3 mg/kg/dose orally (2-3 times a day) or intravenously, repeated after every 2-6 hours.
- Sodium, Potassium, and fluid intake may be restricted to treat mild hypertension.
- A course of antibiotics is administered to eradicate the infectious agent.
- In the presence of severe azotemia, protein intake may also be restricted.
Glomerulonephritis Nursing Management:
- History taking and assessment: The nurse must obtain a complete history of past illnesses and infections. Assess the child’s weight, and urine output and look for the presence of manifestations of glomerulonephritis.
- Monitor fluid status: Monitor fluid and electrolyte status of the child, by assessing daily body weight, periorbital edema, and intake and output.
- Monitor the vital signs of the child.
- Monitor the degree of ascites, by measuring abdominal girth daily.
- Monitor blood pressure and administer the prescribed antihypertensives.
- Restrict fluid, salt, and potassium intake, if prescribed.
- Prevent infection Impaired renal function places the child at risk for infection so:
- Monitor the child for signs of infection like fever, malaise, and elevated WBCs.
- Educate the parents regarding good hand-washing techniques. Limit the number of visitors.
- Nobody with an upper respiratory infection should attend to the child, as the child is already infected.
- Prevent skin breakdown:
- As the child may have generalized edema, there are chances of skin breakdown, so:
- Turn the child frequently and keep changing his position.
- Keep the child clean and dry.
- Keep the bed sheet tight and wrinkle-free.
- Provide frequent back care and skin care.
- Meet the nutritional needs of the child
- Anorexia during the acute phase is the greatest challenge in meeting the nutritional needs of the child.
- Provide low protein and no added salt diet to the child.
- Provide food according to the likes and dislikes of the child.
- Allow the child to eat with other children, as this may motivate him to eat.
- Emotional support:
- The parents may blame themselves for the child’s condition. So discuss with them the causes and treatment and correct their misconceptions.
- Provide emotional support to the parents.
- Answer the queries of the parents and help them to vent their feelings.
Disorder Of Neurological System
Question 24. Define Meningitis, Enlist the clinical features of meningitis, and Discuss the medical management and nursing management of meningitis.
Answer:
Meningitis Definition:
Meningitis is defined as an inflammation of the meninges covering the brain and spinal cord.
Bacterial or Pyogenic Meningitis:
- It is caused by a wide variety of pyogenic bacteria like Haemophilus influenza, Meningococcus, Pneumococcus, Streptococcus etc. Haemophilus influenza and Meningococcus together account for 70% of all cases of bacterial meningitis.
- Bacterial meningitis is almost always a complication of bacteremia occurring due to pneumonia, empyema, osteomyelitis, and endocarditis. It is rarely seen but is serious and can be life-threatening.
Meningitis Clinical Features:
The typical symptoms of meningitis are rarely seen in children less than two years of age. The onset of symptoms is acute in the case of bacterial meningitis but insidious in the case of viral meningitis. The clinical presentation of the child with meningitis depends primarily on the child’s age and etiologic agent.
The clinical features in neonates include:
- Poor Feeding
- Vomiting
- Diarrhea
- Lethargy
- Weak cry
- Sleepiness
- Presence of full fontanel
- The clinical features in infants older than 3 months include:
- Fever
- Irritability
- Poor Feeding
- Vomiting
- High pitch cry
- Seizures
- Bulging Fontanel/ Nuchal Rigidity
The clinical features in children older than 3 years include:
- Fever, chills, and malaise because of infection.
- Headache, Vomiting, and papilledema (rarely seen) because of increased intracranial pressure.
There are signs of meningeal irritation:
- Nuchal rigidity Positive Brudzinski’s sign- With the patient in the supine position, on passive flexion of the neck there is involuntary bending of the hip and knees.
- Photophobia, diplopia, and other visual problems due to cranial nerve irritation.
- Delirium, deep coma, or stupor due to cerebral edema and increased intracranial pressure.
Meningitis Management:
The treatment of meningitis includes:
1. Specific treatment Treatment is started with antibiotics, on the basis of culture and sensitivity report of CSF.
The commonly used antibiotics are:
- Penicillin with third-generation cephalosporins. Vancomycin with third-generation
- Cephalosporin, if penicillin resistance is suspected. Cefotaxine/Ceftriaxone with Aminoglycosides.
Duration of Antibiotic Therapy:
- 7-14 days depending upon the type of organism.
- 3 weeks in case of gram-negative bacteria.
2. Symptomatic treatment:
- Seizure management:
- For controlling seizures, Phenobarbitone 10 mg is given intravenously.
- Dilantin can also be given in a dose of 7 mg/kg body weight. Diazepam 2.5 mg may be given to reduce restlessness.
- Management of increased intracranial pressure: Mannitol -0.5 mg/kg body weight as 20% solution is administered. Frusemide 1mg/kg body weight may be given.
- Fever and headache: Aspirin or acetaminophen may be used to manage fever and headache.
3. Supportive Care:
- IV fluids to maintain fluid-electrolyte balance.
- Patients with septic shock require vasoactive drugs like epinephrine and dopamine.
Meningitis Nursing Management:
1. Isolate the child:
- When a child is admitted with suspected meningitis, the nurse should isolate the child, in order to protect other patients from infection.
- Proper isolation techniques and strict hand washing need to be observed and the parents of the child need to be instructed accordingly.
- Nobody with an upper respiratory tract infection should attend to the child as he is already infected.
2. Administration of drugs:
- Antibiotics and anticonvulsants should be administered as prescribed by the physician.
- Intravenous antibiotics are given for a minimum of 7-10 days.
3. Control seizures and protect the child from injury: Since the child is prone to seizures, the child must be protected from injury.
- Monitor the child’s level of consciousness.
- The side rails of the bed should be up and padded to prevent falls.
- Never leave the child alone.
4. Maintain fluid intake and nutrition:
- If the child is unconscious, intravenous fluids are given to meet the nutritional requirements of the body.
- If the child’s condition permits then nasogastric feeding can be given.
- Maintain intake and output records to assess for any fluid retention, impending shock, and SIADH (Syndrome of inappropriate anti-diuretic hormone).
- In the presence of SIADH, administer only 2/3rd of the total fluid requirement.
- When oral feeds are started, the diet should be rich in protein, calories, and vitamins.
5. Provide comfort and rest:
- The child may have photophobia so avoid bright light in the patient’s room.
- The environment of the child’s unit should be calm, quiet, and thermoneutral to ensure adequate rest and sleep.
- Avoid the use of a pillow as the child is having nuchal rigidity and giving a pillow under the head may cause discomfort.
- Position the child on the side to prevent any aspiration (if the child is unconscious).
- Care should be taken while moving and lifting the child as this may lead to pain and discomfort.
- The head and neck should be supported while lifting the child. Provide passive exercises to the child.
- Other comfort measures include frequent mouth care, changing of position to prevent bed sores, use of air or water mattresses, and keeping the skin clean and dry.
6. Monitor the child’s condition:
- Vital signs should be monitored frequently. Assess the neurological status and level of consciousness frequently.
- Assess the fontanels and measure head circumference daily. Maintain a record of the head circumference of the child. An increase in head circumference indicates the development of hydrocephalus.
Parental Guidance and Support:
Inform the parents about the child’s disease and his condition. If the child develops deficits, teach them about the care of the child at home. Referrals are made as necessary to provide support to the child and family
Question 25. Define hydrocephalus, What are the causes of the hydrocephalus, and list the clinical features of hydrocephalus.
Hydrocephalus Definition:
Hydrocephalus is defined as an imbalance between the production and absorption of cerebrospinal fluid It is characterized by an abnormal increase in the volume of cerebrospinal fluid within the intracranial cavity resulting in enlargement of the infant’s head.
Hydrocephalus Clinical Features:
- The clinical features of hydrocephalus depend on
- Age of the child
- Whether Fontanelle has closed or not
- Whether cranial sutures have fused
- Type of hydrocephalus:
Clinical Features in Infants:
- There is an accumulation of CSF in the ventricles leading to enlargement of the skull.
- Sutures become widely separated
- Delayed closure of anterior fontanelle
- Tense bulging fontanelle
A hollow or ” cracked pot ” sound is heard on the percussion of the skull (Macewen’s sig) :
- Scalp veins are prominent and the scalp appears shiny. The eyes may have a wide bridge between them and a visible sclera above the iris (sun setting sign)
- Neurologically, the infant may be fussy, restless, irritable, apathetic, or have an altered or diminished level of consciousness accompanied by a sluggish pupillary response to light, posturing and spasticity of lower limbs. In addition, there may be feeding difficulty and high-pitched cry due to increased intracranial pressure. The infant may have physical or mental developmental retardation.
Clinical Features in Older Children:
- In older children, there is no enlargement of the head, but there is an increase in intracranial pressure resulting in:
- Headache on awakening in the morning
- Nausea and vomiting
- Irritability and pitch cry
- Lethargy
- Apathy
- Confusion
- Impaired judgment and reasoning skills
- Affected motor abilities (ataxia, spasticity) Papilledema, Strabismus, or decreased visual acuity secondary to compression of optic nerve
Hydrocephalus Causes :
Non-communicating or obstructive hydrocephalus may occur due to congenital reasons or it may be acquired.
Congenital causes:
- Stenosis of aqueduct of sylvius
- Meningomyelocele
- Dandy-walker syndrome (obstruction of foramen of luschka or magendie)
- Arnold-Chiari malformation (a brain defect resulting in herniation of the cerebellum, medulla, pons, and fourth ventricle, through an enlarged foramen magnum)
Acquired causes:
- During the neonatal period and early infancy causes that lead to hydrocephalus are:
- Infections caused by rubella, cytomegalovirus, and toxoplasmosis Spontaneous intracranial hemorrhage
- Intracranial tumors like medulloblastoma, craniopharyngioma, or astrocytoma Head injury.
- The causes responsible for communicating hydrocephalus are: Subarachnoid hemorrhage
- Meningitis
- Toxoplasmosis or Cytomegalovirus infection in which there is obliteration of subarachnoid space due to inflammatory reaction.
- Diseases of connective tissue like Hurler’s syndrome and achondroplasia.
Hydrocephalus Management:
Management of hydrocephalus is directed towards:
- Relief of hydrocephalus or reducing the intracranial pressure
- Prevention and management of complications
- Managing problems caused by the pathology
The treatment of hydrocephalus depends on the cause. Medical management includes the use of osmotic diuretics – Acetazolamide and Frusemide to reduce the rate of CSF production. These medicines provide temporary relief but the main management is surgery for the removal of any space-occupying lesion and the insertion of a shunt.
A shunt is made up of radio-opaque plastic and has a ventricular catheter, a unidirectional pressure valve, a pumping chamber, and a distal catheter that directs the flow of CSF from the ventricles to other areas of the body from where it is absorbed. Thus the shunt helps in removing excessive CSF from the ventricles, thereby reducing the increased intracranial pressure.
Four types of shunts are available:
- Ventriculoperitoneal shunt
- Ventriculoatrial shunt ( from ventricles to the left atrium )
- Ventriculopleural shunt ( from ventricles to the pleural cavity )
- Ventriculoureteric shunt ( from ventricles to the ureter )
The ventriculoperitoneal shunt carries the CSF from the ventricles to the peritoneal cavity. It must have a large space to accommodate the coiled catheter tubing. Commonly used, as the peritoneal cavity provides adequate blood supply to ensure reabsorption of CSF and has a large space to accommodate the coiled catheter tubing.
The complications that may arise with shunt include kinking, separation, or plugging of shunt tubing. The most serious complication is infection which mostly occurs within two months of surgery. Infection of the shunt may lead to ventriculitis and septicemia. Conservative treatment for shunt infection is the administration of antibiotics.
Nursing Management:
Pre-operative: Nursing Care in the preoperative period focuses on the recognition of signs of increased intracranial pressure, providing supportive care, and preventing complications. Nurses must provide the following care:
Measure the head circumference of the child daily:
- Palpate the fontanele for evidence of increased intracranial pressure. The anterior fontanelle is bulging and tense.
- Due to raised intracranial pressure, the sutures may appear to be widely separated.
- Assess the pupillary response and level of consciousness.
- Monitor vital signs regularly. Any changes in vital signs should be promptly reported
- As the infant is irritable and restless, provide a calm and quiet environment so that the infant may take adequate rest.
- Prevent the child from nosocomial infections by using barrier nursing and strict aseptic techniques while providing care.
- Position the body with the neck adequately supported.
- As the scalp becomes thin, there is an increased chance for a breakdown of the scalp so , a water pillow or lamb’s wool may be used to keep the head over it.
- Change the infant’s position frequently.
- Support the infant’s head and neck while handling because the head may be too large and neck muscles may be too weak to support the head.
- The infant is prone to vomiting, so provide small, frequent feeding with intermittent burping.
- Keep the infant clean and dry.
Post-operative Care:
Postoperatively, place the infant in a flat position to prevent rapid CSF drainage and on the unoperated side to avoid pressure on the valve of the shunt.
If CSF is drained too rapidly, there is a risk of subdural hematoma caused by tearing of the vessels secondary to the cerebral cortex pulling away from the dura mater. Check vital signs every 15-30 minutes in the immediate post-operative period.
- Assess the neurological status and level of consciousness frequently.
- Assess the head circumference regularly.
- Monitor the intake and output, as fluids may be restricted during the first 24 hours postoperatively.
- Oral rehydration must be started after the bowel sounds reappear.
- Check dressings for any drainage.
- Meticulous skin care should be provided.
- The child must be observed for signs of infection such as fever, increased heart and respiratory rate, poor feeding or vomiting, altered mental status, and local symptoms such as redness or CSF leakage at the surgical site.
- If the fontanelle becomes sunken, notify the physician immediately. Also immediately lower the head end of the bed to decrease the outflow of CSF through the shunt. This will help in reducing the risk of subdural hematoma.
- Prophylactic antibiotics are administered as prescribed to prevent infections.
- Teach parents about care of the child at home, after discharge from the hospital.
- Tell them about:
- Handling the baby while feeding and positioning the child.
- Recognizing the signs of increased intracranial pressure and malfunctioning or blockage of shunt.
- Pumping of the shunt in case of increased intracranial pressure.
- Preventing constipation if the child has a Ventriculoperitoneal shunt, as straining during defecation may increase the intracranial pressure.
- Importance of follow-up care.
Question 26. Spina bifida
Answer:
Spina bifida is a neural tube defect where there is an incomplete closure of the vertebrae and neural tube.
Spina bifida Definition:
Spina bifida is a malformation of the spine, in which the posterior portion of the lamina of the vertebra fails to close with or without defective development of the spinal cord.
Incidence and Etiology:
Spina bifida is the most common developmental defect of the central nervous system, occurring in about 1 or 2 per 1000 live births. Spina bifida may occur in any area of the spine but most commonly occurs in the lumbosacral area.
The etiological factors associated with spina bifida are: (Causes)
- Genetic: A child of parents with spina bifida carries 15 times more probability of inheriting the defect.
- Maternal Age: The disorder is twice as common in pregnant mothers over 35 years of age or below 20 years of age.
- Environmental: Radiations increase the risk of defective neural tube development. Regional differences are also seen. The incidence of spina bifida is higher in Great Britain. It is three times more than in the USA
- Diet: Folic acid deficiency in the diet of a pregnant mother increases the risk of meningomyelocele in the baby
Spina bifida Classification: Spina bifida is of two types
- Spina Bifida occult
- Spina bifida cystica
- Meningocele
- Myelomeningocele
- Spina bifida occulta: It is a defect that results from failure of the formation of a bony arch around the spinal cord, but the spinal cord and meninges are normal It is not visible externally and
is asymptomatic This type of defect occurs in 5 % of cases of spina bifida. - Spina bifida cystica: Spina bifida cystica is a defect in the closure of the posterior vertebral arch with protrusion of the spinal cord and meninges through the defect
- Meningocele: It is a sac-like herniation through the bony malformation, containing meninges and cerebrospinal fluid. The covering of the sac may be thin and translucent or membranous.
- Myelomeningocele: It is a sac-like protrusion of the spinal cord, CSF, and meninges through the spinal cleft. During embryonic life, the lumbar segment of the spinal cord is the last part of the neural tube to close, therefore in most cases, meningomyeloceles are found in the lumbar or, lumbosacral region.
The defect may occur in lumbosacral region ( 70 % ), lower lumbar region ( 47 % ), upper lumbar region ( 23 % ) and sacral region ( 2.6 % ).
Spina bifida Pathophysiology:
- Spina bifida occurs because of defects in the orderly closure of the vertebral column and formation of the spinal cord during the 4th to 6th weeks of gestation.
- During the 3rd week of gestation, a depression forms in the dorsal of the ectoderm in the embryo. This depression becomes deeper and its margins close dorsally to create a neural tube.
- The ends of the neural tube close by the end of 4th week of gestation. The walls of the neural tube thicken and become the spinal cord and brain.
- The neural canal becomes the ventricles and the central canal of the spinal cord. The vertebral column is formed simultaneously with the neural tube. The exact mechanism by which neural tube defect occurs is not certain.
Two theories are proposed regarding the occurrence of defects:
- The neural tube fails to close normally or
- Neural tube ruptures after having once closed
Spina Bifida Clinical Features:
1. Spina Bifida Occulta: Most of the patients with spina bifida occulta are asymptomatic.
The only features seen are:
A dimple in the skin or growth of hair over malformed vertebra As the child grows, he may develop foot weakness or disturbances of the bladder and bowel sphincter.
- Progressive deformity of the foot
- Change in micturition pattern
- Alteration in gait
- Tropic ulcer on the toes and feet.
2. Spina Bifida Cystica:
Meningocele:
- An external cystic defect can be seen at the back. The sac is composed only of meninges and is filled with CSF.
- The spinal cord and nerves are normal. There is seldom evidence of weakness of the legs or lack of sphincter control.
Myelomeningocele:
- Seen in 1 out of every 800 infants, manifestations of myelomeningocele depend on the location and extent of the defect. The higher the deformity the more neurological deficits will be present.
- A round, raised, poorly epithelialized, herniated mass is present over the vertebral column, mainly in the lumbosacral region.
- Approximately, 90 % of infants with severe spina bifida develop hydrocephalus due to associated Arnold – Chiari syndrome. Loss of motor control and sensation occurs, below the level of lesion.
A low thoracic lesion may cause total flaccid paralysis.
- A Sacral lesion leads to weakness of the lower limbs. Bowel and bladder may or may not be affected; there may be fecal and urinary incontinence
- There may be renal impairment due to faulty renal innervation. Urinary tract infections are common complications associated with the defect.
- Congenital skeletal anomalies may be present in these children due to the denervation of muscles like clubfoot, developmental dysplasia of the hip, kyphosis, or scoliosis.
- These deformities are not only a cosmetic problem, they may also lead to back pain, respiratory distress, recurrent skin breakdown, and difficulty in movement.
Developmental delays are commonly seen in speech, mobility, etc.
Diagnostic Evaluation:
1. Prenatal diagnosis of neural tube defects is possible by using the following tests:
- Ultrasound
- Fetal MRI
- Amniocentesis: It may reveal an increase in alpha-fetoprotein, a fetal-specific gamma globulin in the amniotic fluid that indicates the presence of meningomyelocele. This test should be done between the 14th to 16th week of gestation in all pregnant females who are at risk.
2. Diagnosis after birth is made on the following basis:
- On neonatal examination, a sac may be seen on the back of the baby
- If a lesion is present, its contents can be determined using a trans-illumination test ( shining light through the sac ). If the sac becomes translucent when the light source is held to it, it is a meningocele, if the sac does not become translucent, it is a myelomeningocele.
- CT scans and MRIs of the spinal cord and brain are used to determine bony deformities and spinal cord herniation. They also help in diagnosing the presence of other structural defects like hydrocephalus or Arnold-Chiari malformation. etc may be done.
- Laboratory tests like urine tests for the presence of infection, Renal function tests, WBC counts, ESR
- Other tests include neurological assessment for motor response and sensory reactions, developmental assessment to detect any delay in milestones, etc.
Spina Bifida Management:
- The management of spina bifida depends on the nature and extent of the defect. Usually, no intervention is required for spina bifida occulta. For spina bifida cystica surgery is required Laminectomy and closure of the defect or removal of the sac is done within 24-48 hours of birth. T – Closure of skin graft is done.
- A co – ordinated multidisciplinary team approach is required to maximize the physical and intellectual potential of each affected child. A team of neurologists, neurosurgeons, orthopedic surgeons, urologists, primary care providers, nurses, speech therapists, and physiotherapists need to work together to manage the child.
Nursing Management:
The main aims of pre and post-operative nursing care are the prevention of infection
- Preventing injury to the sac
- Prevention of skin breakdown.
- Preventing urinary tract infection Preventing leg and hip deformities Provision of adequate nutrition.
Question 27. Define and write the classification of Epilepsy Seizures. Clinical manifestation of Status Epilepsy. Nursing management of Epilepsy.
Epilepsy Seizures Introduction:
Epilepsy is a disorder in which a person has repeated seizures.
Epilepsy Seizures Definition:
- Convulsions are a series of forceful involuntary contraction and relaxation of voluntary muscles due to disturbance of brain function.
- Convulsions are abnormal, involuntary, paroxysmal, motor, sensory, autonomic, or sensorial changes resulting from abnormal electrical discharges from the brain.
Seizures Classification:
The international classification of epilepsy is currently used to classify seizures This Classification Broadly divides seizures into two types.
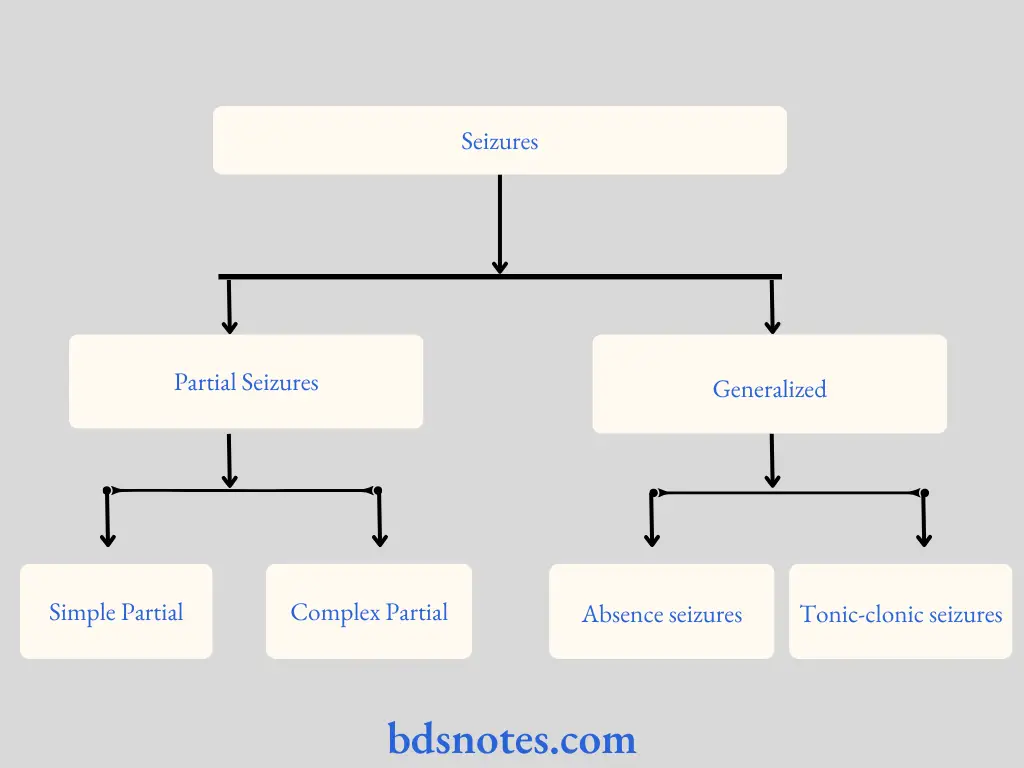
Partial Seizures:
- Partial seizures begin focally and result from abnormal electrical discharges from a circumscribed small portion of the brain.
- Partial seizures affect awareness or memory of events before, during, and immediately after seizures.
Generalized Seizure:
Generalized seizures involve abnormal electrical discharges from both cerebral hemispheres. Motor abnormalities, if any are bilaterally symmetric. Consciousness is always impaired. Absence seizures and tonic-clonic seizures are examples of generalized seizures.
- Tonic-clonic seizures (Grand mal)
- Absence seizures:
- Typical (petit mal)
- Atypical
- Atopic seizures (drop attacks)
- Myoclonic seizures.
Partial Seizures:
1. Simple partial seizures (with elementary symptoms and no impaired consciousness)
- With motor signs (Jacksonians or focal motor)
- With somatosensory or special sensory, i.e. visual or auditory.
- With autonomic manifestations (abdominal epilepsy)
2. Complex partial seizures manifested with impaired consciousness and with automatism. It includes psychomotor or temporal lobe seizures.
Status Epilepticus:
It is a state of continuing or recurrent seizures that are prolonged for more than 30 minutes or occur in a series without regaining consciousness in between attacks. It is a medical emergency as cerebral damage may occur due to prolonged cerebral hypoxia or hypoglycemia. In the postictal state, the child may have ataxia, aphasia, and mental sluggishness.
The mortality rate due to this condition is about 4 percent. The child may have cardiorespiratory arrest or aspiration of vomitus. Residual neurological deficits may develop in 9 percent of cases. Todd’s paresis or postictal paralysis may result due to metabolic exhaustion of epileptic neurons.
The symptoms include: Clinical Manifestation
Abnormal muscle contraction:
- Muscle contraction/relaxation
- One side of the body is affected
- Abnormal head movements
- Forced turning of the head
Automatism:
- Repetitive purposeless movements
- Starring spells Lip smacking Chewing/swallowing without cause
Abnormal sensations:
- Numbness, tingling, crawling sensation on the skin.
- May occur in only one part of the body or may spread.
- May occur with or without motor symptoms.
- Hallucinations (Auditory or visual)
- Abdominal pain or discomfort
- Flushed face and dilated pupils
Other symptoms include Blackout spells Changes in vision Changes in mood or emotion and confusion in the post-actual phase.
Seizures Nursing Management:
- Nurses should be prepared to administer emergency treatment to seizure patients and should
- Instruct family members concerning first aid measures.
Emergency care during seizures:
It includes the following:
- Assist the child to a lying position.
- Take off eyeglasses, if the child wears and loosen tight clothes.
- Remove dangerous objects from the vicinity of the child.
- Maintain patent airway and adequate oxygenation must be ensured.
- Administer the prescribed medications on time.
- Do not restrain the child during seizures.
- The side rails of the bed should be padded.
- Do not force anything into the child’s mouth during seizures.
Care of the child after seizures:
- After the seizures are over, the child should be provided complete bed rest.
- Change the clothes and bed sheet, if soiled.
- Suction the airway, if excessive secretions are present.
- Turn the face of the child to one side, to avoid aspiration of secretions.
- Give CPR if breathing is not re-established after the attack.
- Observe the child until fully conscious.
- Treat any injury that may have occurred during convulsions.
- Continuously monitor the vital signs of the child.
- After the child is awake and fully conscious, give oral fluids like fruit juice, lemonade, etc.
- Administer intravenous fluids if oral intake is less.
- Maintain intake and output chart. Provide a non-stimulating, calm, and quiet environment to the child.
- Parents need to be counseled regarding the disease and its prognosis.
- Parents should be taught how to take care of their children at home.
- The child should not be left alone and should not be allowed to perform activities that involve risk of injury.
- The child who is a known case of epilepsy should wear a medical identification card.
Disorder Of The Musculoskeletal System
Question 28. Club Foot
Answer:
Club Foot Introduction:
- Club foot is a congenital anomaly of the foot and lower leg, involving abnormalities of bony architecture and soft tissue. The foot may be divided into the forefoot (toes and metatarsals), midfoot (cuneiforms, navicular, cuboid), and the hindfoot (talus and calcaneus).
- Although the tibiotalar joint (ankle) provides plantar flexion and dorsiflexion, the subtalar joint (between talus and calcaneus) is oriented obliquely, providing inversion and eversion.
- Inversion represents a combination of plantar flexion and varus, and eversion involves dorsiflexion and valgus. The talonavicular and calcaneocuboid joints connect the midfoot with the hindfoot.
Club Foot Definition:
- The term club foot is used to describe a common deformity in which the foot is twisted out of its normal shape or position. Any foot deformity, involving the ankle is known as ’talipes’ derived from ’talus‘ meaning ankle, and ’pes‘ meaning foot.
- The clubfoot deformity can be positional or congenital.
- Positional club foot is a normal foot that has been held in a deformed position in utero and is found to be flexible on examination.
- The congenital club foot involves genetic factors and defects like Edward’s syndrome.
- Growth arrest at roughly 9 weeks and compartment syndrome of the affected limb causes congenital club foot.
Club Foot Incidence and Etiology:
Congenital club foot is seen in approximately 1 per 1000 live births.
Club Foot Clinical Features:
Clinical features of club foot include
- Adduction of the forefoot or metatarsus adductus.
- Contracture of Achilles tendon leading to equinus position or plantar flexion of the foot.
- The foot is also inverted so the lateral border is directed downwards.
- Development of the lower leg is also affected and the calf muscles appear thin and atrophic.
Club Foot Nursing Management:
Nursing Diagnosis is as follows
- High risk or impaired skin integrity related to application of casts.
- Parental anxiety and grieving related to impaired adjustment to anomalous condition.
- High risk for body image disturbance related to residual or recurrent deformity.
1. Nursing objective: To maintain the skin integrity.
Nursing Interventions:
- After surgery, the child has to undergo repeated casting so skin integrity needs to be taken care of.
- The nurse should assess the condition of the skin under the cast.
- A cast that is too tight can put pressure on the neurovascular structures. So the caregivers must be taught how to assess the neurovascular status of the toes.
- The skin at cast edges must be frequently assessed and provided care.
2. Nursing objective: To support the family through anxiety or grieving.
Nursing Interventions:
- The family members should be allowed to verbalize their feelings, concerns, and fears.
- The nurse must encourage the parents to view the child as a whole and not just the club foot deformity.
- The nurse must support the caregivers throughout the treatment.
3. Nursing objective: To promote healthy body image.
Nursing Interventions:
- It is frustrating to have a residual or recurrent deformity. The nurse should provide information to the family about further treatment options.
- The nurse must encourage the family for constant follow-up till the child reaches skeletal maturity.
- The child with residual deformity should be encouraged to participate in age-appropriate physical activities.
Common Communicable Diseases
Question 29. Measles
Answer:
Measles is an acute, infectious disease manifested by fever, cough, coryza, lacrimation, and koplik’sspots in the pre-eruptive phase and maculopapular rash starting on the 4th or 5th day of illness.
Measles Epidemiology:
- Agent: Measles is caused by an RNA virus belonging to paramyxoviridae family.
- Reservoirs of infection: Man is the only reservoir of infection.
- Transmission of infection: By droplet infection from secretions of nose and throat usually 4 days before and 5 days after the appearance of rashes.
- Incubation period: 8-12 days Occurs in preschool children In all seasons, more in winter and spring months
Risk Factors:
- Unvaccinated children
- Children with immune deficiency due to HIV
- Leukemia
- Corticosteroid therapy
- Malnutrition
- Vitamin A deficiency.
Measles Clinical Features:
1. Prodromal Phase/Catarrhal stage (Enanthema):
The onset is acute with moderate elevation of
- Temperature
- Hacking cough
- Running nose Sneezing
- Redness of eyes
- Excessive lacrimation
On the 2nd on 3rd day of illness ’Koplik’s SPOTS’ appear on the inner side of the cheek, opposite to the lower molar teeth.
- These may be single or multiple and appear as greyish or bluish-white grains of sand, surrounded by reddish areola.
- Koplik’s spots increase in number for 2-3 days.
2. Eruptive Phase/Exanthema:
- The whitish appearance of rash on 4th day
- Fever tends to rise.
- The early rash is erythematous and blanches on pressure.
- Rashes first appear behind the ears, near the hairline on the forehead, face, and neck, and spread to the trunk, extremities, palms, and soles within 3 days.
- The rash now appears brown and doesn’t fade on pressure. As rashes increase fever rises and pruritis occurs
3. Convalescent stage/Decline:
The rash starts disappearing after 4-5 days in the same order in which they appeared leaving behind a browny desquamation. Anorexia and malaise are present. A moderate generalized Lymphadenopathy may be seen.
Measles Types:
1. Modified measles:
- Observed in partially immune individuals.
- The symptoms are milder and the duration of the illness is short.
2. Atypical Measles:
Occurs in previously immunized persons after exposure to natural infection. Rashes are associated with hepatosplenomegaly and sensory symptoms.
3. Hemorrhagic measles:
It is characterized by
- High fever
- Convulsions
- Delirium
- Stupor
- Coma Bleeding occurs from the mouth, nose, and bowel and may result in death.
Measles Nursing Management:
- Bed rest in the febrile stage.
- Isolation up to 4-5 days after rashes appear. The catarrhal stage is highly infective.
- Oral hygiene should be attended to every 4 hours.
- Skin hygiene should be attended to.
- Parents should be encouraged to give baths to the child.
- Care of the eyes is important. Wash eyes with warm water to prevent ulceration and soothe irritation.
- Oral fluid intake should be adequately maintained during fever. If there is vomiting give intravenous fluids.
- Maintain the child’s nutrition because, after measles, the child becomes malnourished, PEM is precipitated and also child becomes prone to TB.
- Protein and calorie intake should be high.
- Milk with sugar, egg, juice, etc. should be given to the child.
- Fever is controlled by PCM and sponging.
- Severe cough is relieved by humidification or saline nebulization.
- Vitamin A, 2 lakh IU, given orally to children above 1 year of age for two consecutive days reduces the severity, complication rate, and mortality due to measles.
- Management of complications is essential. For respiratory complications -Antibiotics are given.
Convulsions – Diazepam/ Phenobarbitone may be given.
Measles Prevention:
- Live attenuated measles vaccine offers good protection to susceptible children. It is given at 9-12 months with revaccination at 18 months as part of the MMR vaccine.
- Passive immunization in exposed infants with Y globulin intramuscular 0.25 ml/kg for children less than 1 year of age.

Leave a Reply