Growth And Development Short Answer Questions
Question 1. Define growth and development.
Answer:
- Growth: Growth refers to an increase in the size or mass of the tissues. It is largely attributed to the multiplication of cells and the increase in intracellular substances. It can be measured in inches centimeters, kilograms, and pounds. So it is a quantitative term.
- Development: Development specifies the maturation of functions or physiological maturation The term ‘ development ’ is used to refer to a progressive increase in skills and capacity to function. It is a qualitative change in a child’s functioning and is difficult to measure. Development is the result of maturation and learning.
Read And Learn More: Bsc Nursing 3rd Year Child Health Nursing Previous year Question And Answers
Question 2. Principals of growth and development
Answer:
- Growth: Growth refers to an increase in the size or mass of the tissues. It is largely attributed to the multiplication of cells and the increase in intracellular substances. It can be measured in inches centimeters, kilograms, and pounds. So it is a quantitative term.
- Development: Development specifies the maturation of functions or physiological maturation The term ‘ development ’ is used to refer to a progressive increase in skills and capacity to function. It is a qualitative change in a child’s functioning and is difficult to measure. Development is the result of maturation and learning.
Principles / Characteristics of Growth and Development:
Gessel (founder of clinical child psychology) has concluded from genetic studies of children – “although no two children are alike, all normal children tend to follow a general sequence of growth”. There are certain basic predictable characteristics or principles of growth and development which are as follows:
1. Development is Similar for all:
- All children follow a similar pattern of development with one stage leading into the next.
- Every child passes through similar stages. For example, the baby learns to stand before he walks, similarly, the baby draws a circle before a square.
2. Development Proceeds from General to Specific:
- In motor as well as mental responses, general activity always precedes specific activity.
- Before birth, the fetus moves the whole body but is incapable of making specific movements. Generalized body movements occur before fine motor control is achieved.
- For example, first, the infant moves the whole body in the womb and later starts moving his hands. Similarly, infants move their hands first and then learn to use their fingers.
3. Development is Continuous:
- Development is a continuous process, starting from conception and ending at death.
- It is continuous but sometimes rapid and at times slow.
- For example, speech in a child does not develop overnight, the child coos, gurgles, and makes sounds first and then slowly and gradually learns words, and then language develops.
4. Development proceeds at Different Rates:
- Growth and development is a continuous process that is rapid at times and at times slows down.
- Rapid growth occurs during fetal life and infancy and it slows down during school age.
- A growth spurt occurs in puberty and early adolescence but it slows down during adulthood and old age.
5. There is a Correlation in Growth and Development:
- Correlation in physical and mental abilities is especially marked.
- There is a marked relationship between sexual maturation and patterns of interest and behavior.
6. The development comes from Maturation and Learning:
- The sudden appearance of certain traits that develop through maturation is quite common.
- For example, a baby may start walking overnight. Behavioral changes occur at the time of puberty suddenly without any reason. Learning comes from exercise and effort on the part of an individual.
- Unless the child has the opportunity to learn, many of his hereditary potentials will never reach their optimum development.
- For example, a child may have an aptitude for music because of his superior neuromuscular organization, but if he is deprived of opportunities for practice and systematic training, he will not reach his maximum potential. Intrinsic growth is a gift of nature. Innate capacities should be stimulated by positive environmental factors.
7. There are Individual Differences:
- Although the pattern of development is similar for all children, each child follows a predictable pattern in his own way and at his own rate.
- Each child with his unique heredity and nature (environment) will progress at its own rate in terms of size, shape, capacity, and developmental status.
8. Early Development is More Significant than Later Development:
- If the foundation of a building is strong, the building will be strong.
- Similarly, favorable conditions during infancy lead to the growth of child into a healthy adult.
- If the conditions during the prenatal period and postnatal period are unfavorable, there is a damaging effect on later growth and development of the child.
9. Development Proceeds in Stages: Development is not abrupt, it proceeds in stages that are as follows:
- Prenatal period: From conception to birth
- Neonatal Period: Birth to four weeks Infancy: Four weeks to 1 year
- Toddler: From 1-3 years
- Preschool: 3-6 years (early childhood)
- School-age: 6-12 years (late childhood)
- Adolescence: From puberty to beginning of adulthood (13-18 years)
10. There are predictable patterns of growth and development: Both during prenatal and postnatal periods, growth and development follow two patterns.
- Cephalocaudal
- Proximodistal
According to the cephalocaudal pattern, development spreads over the body from head to foot. This means that improvement in the structure and functions of the body comes first in the head region, then in trunk, and lastly the legs.
According to the proximodistal pattern, development proceeds from near to far, i.e. from the central axis of the body towards the periphery or extremities. During the prenatal period, the head and trunk develop fully and then the limb buds appear. Slowly the arms lengthen, followed by the forearms and lastly the fingers. Functionally, the baby starts using his arms before his hands and fingers.
Question 3. Factors Affecting the growth and development.
Answer:
- Growth: Growth refers to an increase in the size or mass of the tissues. It is largely attributed to the multiplication of cells and the increase in intracellular substances. It can be measured in inches centimeters, kilograms, and pounds. So it is a quantitative term.
- Development: Development specifies the maturation of functions or physiological maturation The term ‘ development ’ is used to refer to the progressive increase in skills and capacity to function.
It is a qualitative change in a child’s functioning and is difficult to measure. Development is the result of maturation and learning.
Factors Affecting Growth and Development:
- Growth and development depend not only on one but a combination of many factors. The typical pattern of growth and development is regulated by a complex balance between heredity or genetic constitution and environmental factors.
- Heredity determines the extent to which growth and development are possible and environment determines the degree to which the maximum potential is achieved.
1. Heredity / Genetic Factors:
- Heredity:
- It refers to the genetic constitution of an individual which is established during conception.
- It is that property by which offspring have the nature and characteristics of parents or ancestors.
- From parents, the child receives a combination of parental genes. Every individual’s supply of genes is given to him at the time of conception.
- The color of eyes, hair, facial features, the structure of the body, physical peculiarities, blood group, etc. are determined entirely by heredity.
- It is because of heredity that members of a family have a physical resemblance to each other.
- Race: The growth potential of children of different racial groups is different.
- Sex: The sex of the baby is determined at conception. After birth, the male infant is longer and heavier than a female infant. At the age of 1 year, there is no difference in the length and weight of male and female infants. During puberty, a growth spurt occurs and boys become taller and heavier than girls of their age.
- Biorhythm and Maturation: Daughters often reach menarche at the same age as their mothers. Also, the length of the menstrual cycle is the same as that of the mother.
- Genetic Disorders: Growth and development are adversely affected by certain genetic disorders.
These disorders are of two types:
- Chromosomal abnormalities like Turner’s syndrome and Down’s syndrome which cause growth retardation
- Gene mutations may lead to metabolic defects like galactosemia
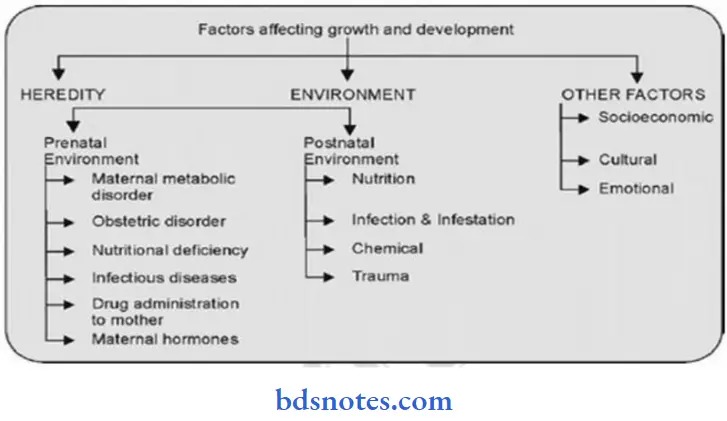
2. Environmental Factors:
Although each human being at birth has a genetically determined physical, mental, and biochemical potential, this potential may or may not be reached because of environmental Influences. Stimulation for the development of innate abilities comes from the environment which may be favorable or unfavorable.
Prenatal Environment:
- The environment that the fetus gets in utero, before birth is known as the prenatal environment. This environment provides nutrition and does gas exchange also. The uterus protects the fetus from the adverse effects of external conditions. A substandard or diseased Intrauterine environment hurts the growing fetus.
- For example, intrauterine rubella infection produces a severe reduction in the quantity of cells in many organs while toxemia in late pregnancy leads to a significant increase in cell size though the number of cells is normal.
The factors affecting fetal growth are as follows:
- Nutritional deficiency in mother: Maternal undernutrition and anemia lead to intrauterine growth retardation and consequently the small size of the fetus.
- Obstetric Disorders: Obstetric disorders like pregnancy-induced hypertension, pre-eclampsia, multiple pregnancy, and malposition of the fetus produce fetal growth restriction.
- Metabolic Disorders in Mother: Disorders of metabolism like Diabetes mellitus lead to a large size of the fetus.
- Infections: Maternal rubella infection occurring during the first trimester of pregnancy results in congenital malformation in the fetus. Children with birth defects cannot grow at an optimal rate. Other maternal infections like Syphilis, Hepatitis B, HIV, Cytomegalovirus inclusion, Toxoplasmosis, etc. may be transmitted to the fetus which may arrest or retard the growth of the fetus.
- Administration of Certain Drugs: Consumption of certain drugs like Thalidomide by the mother during the first trimester of pregnancy adversely affects the embryo and leads to birth defects. These drugs are called teratogenic agents.
- Influence of Maternal Hormones:
- Thyroxine: The human fetus secretes thyroxine from the 12th week of gestation. Thyroxine deficiency in the mother retards skeletal maturation in the fetus. Maternal myxedema results in hypothyroidism in the fetus.
- Insulin: Insulin stimulates fetal growth. In mothers with diabetes, the fetus is usually large with excessive birth weight. As maternal blood sugar levels is high, fetal blood sugar is also elevated. This leads to hyperplasia of islet cells of the fetal pancreas leading to excessive insulin secretion resulting in macrosomia.
Postnatal Environment:
The environment that the baby gets after birth is known as the postnatal environment. This environment determines the pace and pattern of growth and development. Postnatal environmental factors affecting growth and development are:
- Nutrition: The growth of children suffering from protein-energy malnutrition, Anemia, and Vitamin deficiency diseases ( like rickets ) is severely affected. Also overeating and overnutrition lead to obesity.
- Infections and Infestations: Persistent or recurrent diarrhea and respiratory tract infections are common causes of growth impairment. Systemic infections and parasitic infestations usually decrease the velocity of growth
- Chemical Agents: Consumption of androgenic hormones accelerates skeletal growth.
- Trauma: Fracture of the end of bone, damages the growing epiphysis and thus hampers skeletal growth. Head injury may cause brain damage and seriously jeopardize the mental development of the child.
3. Other Factors:
Socioeconomic Condition:
- The environment of children born in lower socioeconomic groups is usually less favorable than those in middle and upper groups.
- Parents with poor financial conditions usually cannot take proper care of their children, as they do not have money to buy essentials of health and diet.
- Poverty, crowded and unhygienic living conditions lead to retardation of growth and development in children.
Cultural Influences:
- Culture influences the child-rearing and infant-feeding practices in the community. There are many cultural taboos against the consumption of particular foodstuffs. This affects the nutritional status and growth of the children.
- For example, some communities are strictly vegetarian and do not consume eggs, meat, etc. The children of these communities do not get proteins of high biologic value due to which their growth may be retarded.
- Similarly in some communities, colostrum is not fed to the child as it is considered impure yellow milk. This practice devoids the children of many nutritional substances and antibodies present in colostrum which makes these children susceptible to infections thereby affecting growth.
Emotional Factors:
- Children from broken homes and orphanages do not grow and develop at an optimal rate. Anxiety, insecurity, lack of emotional support, and love from the family affect the neurochemical regulation of hormones.
- Which affects the growth and development of children On the other hand, parents who have a happy childhood and have cheerful personalities transmit these characteristics to their children.
Question 4. Aspects of growth and development.
Answer:
Growth and development have the following aspects:
- Growth
- Growth
- Biological growth Sensory Growth Motar Growth
Developmental: Intellectual Moral Emotional Sexual Social Language.
- Growth: Growth refers to an increase in the size or mass of the tissues. It is largely attributed to the multiplication of cells and the increase in intracellular substances. It can be measured in inches centimeters, kilograms, and pounds. So it is a quantitative term.
- Development: Development specifies the maturation of functions or physiological maturation The term ‘ development ’ is used to refer to the progressive increase in skills and capacity to function. It is a qualitative change in a child’s functioning and is difficult to measure. Development is the result of maturation and learning
Growth:
1. Biologic Growth: Changes in the body result from the growth of different parts of the body. The National Center for Health Statistics ( NCHS ) made a massive survey of characteristics of growth – length or height, weight, and head circumference. These are the parameters for assessing growth in children.
- Length or Height:
- Length or height increases from birth to maturity. The rapid increase in height occurs during infancy and adolescence.
- The average length of a newborn is 45-50 cm and it increases at the rate of 2-2.5 cm/month for the first six months and then 1.25 cm/month during the next six months.
- At the age of 1 year length is 75 cm. The height of an infant doubles at the age of 4 years and triples at 13 years.
- Weight:
- Weight is the best gross index of health and nutritional status of children. The average weight of a newborn is 2.5-3.5 kg.
- There is an initial loss of weight during the first 10 days of life due to adjustment to extrauterine life, inadequate feeds, and digestive adaptation.
- After 10 days of life, the baby gains about 30 gms weight per day for 5-6 months so weight doubles at 6 months of age and becomes about 5-6 kg.
-
- Thereafter weight gain becomes grams per day during the next 6 months. So at the age of one year, weight becomes triple of birth weight ( about 7.5-8 kg )
- At the age of 2 % years, weight becomes four times the birth weight which is 10-12 kg.
- Head Circumference:
- The head circumference is an important measurement since it is related to intracranial volume. An increase in head circumference indicates the rate of brain growth.
- At birth, the normal head circumference is 33 cm approximately and it increases at the rate of about ½ inch per month during the first 6 months and then at the rate of ¼ inch per month during the next 6 months.
- The head circumference is 40 cm at 3 months and 45 cm at 1 year of age.
- Chest Circumference:
- The chest is barrel-shaped at birth and the anterioposterior and transverse diameters are equal.
- Gradually the transverse diameter increases, causing the width to become greater than the anteroposterior diameter.
- At birth chest circumference is 31cm and at the end of 1 year head circumference becomes equal to the chest circumference, thereafter only the chest circumference increases.
2. Motor Growth: Motor development depends on the maturation of the muscular, skeletal, and nervous systems. The motor development follows a cephalocaudal and proximodistal pattern.
Motor development is of two types:
- Gross Motor: Gross Motor development leads to the acquisition of increasing mobility and independent movements. Gross motor activities include turning, sitting, standing, and walking.
- Fine Motor: Fine Motor development leads to the acquisition of motor dexterity like the use of hand and fingers, palmar grasp and release, pincer grasp, etc.
3. Sensory Growth:
- Although the sensory system is functional at birth, the child gradually learns the process of associating meaning with a perceived stimulus.
- The most active senses at birth are sense of taste and smell. As myelinization of the nervous system occurs, the child can respond to specific The visual system is last to mature, at about 6-7 years of age.
Development:
Many theories have been devised to study the development of different aspects in children.
- Intellectual Development theory by Jean Piaget
- Moral Development theory by Jean Plaget and Kohlberg
- Psychosocial Development theory by Eric H Erikson
- Spiritual Development theory by James W Fowler
- Sexual Development theory by Sigmund Freud
- Emotional Development Theory by Eric H.
Question 5. Discuss the Psychosocial Development theory.
Answer:
Psychosocial Development: The theory of Erikson Concerning ‘ Psychosocial Development ’ states that emotional or personality development is a continuous process which has
The following stages:
1. Trust Versus Mistrust ( Birth to one year – Infant ):
- Infants learn to trust the adults and are sensitive to their needs.
- A negative usually the parent’s care for the outcome of the period of infancy is the sense of mistrust that develops if the basic needs of the infant are not met.
2. Autonomy Versus Shame ( One to three years – Toddler ):
- Infants develop from clinging, dependent creatures into individuals with minds and will of their own.
- The three major psychosocial tasks of toddlerhood are gaining self-control, developing autonomy, and increasing independence.
- If the child succeeds in the development of autonomy he develops a feeling of self-esteem, but if he does not succeed, he doubts his abilities and develops a sense of shyness and shame.
3. Initiative Versus guilt ( Three to six years – Preschool child ):
- This is a period of very energetic play and active imagination. The child can develop a sense of accomplishment and satisfaction in his or her activities.
- As the child oversteps his or her limits he or she experiences a feeling of guilt.
4. Industry Versus Inferiority ( Six to twelve years- School age child ):
- Children in this age have a strong sense of duty. Their energy is channeled into activities such as school projects, sports, and hobbies.
- These concrete endeavors become the child’s work and industry, and feelings of inferiority may develop. bring a sense of accomplishment. If the children are not able to achieve a sense of
5. Identity Versus Role Diffusion ( Twelve to fifteen years – Beginning of Adolescence ):
- Two major tasks for adolescents are figuring out who they are and what is their place in the world.
- Success in this period makes the individual well-adjusted, stable and mature. Individuals who have not experienced any active exploration nor made a commitment to any occupation, develop identity diffusion.
6. Intimacy versus self-absorption ( Late Adolescence ):
- In this stage, the adolescents focus on forming intimate relationships with others. They develop a sense of intimacy with peers.
- Failure to establish such intimacy results in psychological isolation, i.e. keeping relations without warmth.
Question 6. Discuss the Psychosexual Developmental theory
Answer:
Psychosexual Development:
By the view that basic human motivation is a sexual drive, Sigmund Freud developed a psychosexual theory of human development from infancy onwards, divided into a series of psychosexual stages.
Freud named these stages as Oral, Anal, Phallic, Latency, and Genital. Each stage focuses on the gratification of libido through a particular erogenous zone of the body. If a child does not complete a stage, he or she will develop a fixation that will later influence adult personality and behavior.
- Oral stage ( Infancy, the first year of life ): This is the first stage exemplified by an infant’s pleasure in nursing. The gratification of needs centers around feeding.
- Anal stage: ( Toddler Period, 2-3 years ): This stage revolves around an interest in body functions and gratification of needs by retaining and expelling faces.
- Phallic Stage ( Preschool period, end of 3rd year of age up to 5 years ): In this stage, the site of greatest sensual pleasure is the genital region. In this stage oedipal conflict arises, wherein a boy desires for his mother but has a fear of castration by a rival father. In this stage, the boys fixate on the mother as a sexual object ( known as the Oedipus Complex ) but the child eventually overcomes and represses this desire because of its taboo nature. Freud attempts to formulate a comparable process for girls fixating on fathers ( known as the Electra Complex ).
During this stage, the child loves parents of the opposite sex and takes them as providers of sensual satisfaction:
- Latency stage ( School age, 6-12 years ): This is a repressive or dormant stage of psychosexual development.
- Genital Stage ( About 12 years to adulthood ): During this stage, a developing human matures from a pleasure-seeking infant into a sexually mature adult who is free to enter heterosexual relationships.
Question 7. Breastfeeding advantages.
Or
Breastfeeding, importance, advantages.
Answer:
Breastfeeding is the wholesome food for the baby. Breastfeeding is the most effective way to provide babies with a caring environment and complete nutrition. it meets the nutritional as well as emotional needs of the baby. UNICEF and WHO recommended exclusive breastfeeding to babies until six months of age.
Advantages of Breast Feeding:
Breastfeeding is ideal for neonates. It has several advantages both for the baby and the mother.
Advantages for Baby:
1. It is a wholesome food for the baby as it contains all the nutrients that a baby needs in the first 6 months of life for optimum growth and development.
- Proteins: Human milk has lower protein ( 0.7gm / dl ) than cow’s milk ( 3.5g / dl ) which lowers the solute load on the kidneys of babies. Also, human milk protein mainly ( lactalbumin ) is more easily digested than cow’s milk protein ( Casein ).
- Fat: Higher content of mono-unsaturated fatty acids especially linoleic acid in human milk promotes brain growth and protects individuals from atherosclerosis in later life.
- Minerals: Human milk contains a smaller but more balanced proportion of calcium and phosphorous as compared to cow’s milk.
2. Lowers Risk of Infection:
- Human milk contains high levels of lysozyme and IgA which offers protection to the baby against several viral and bacterial diseases.
- Breast milk especially colostrum contains numerous host defense factors like macrophages, granulocytes, T, and B lymphocytes.
- Lactoferrin present in breast milk protects the baby from enteric infections. Para-aminobenzoic acid ( PABA ) present in breast milk protects the baby from malaria.
3. Protects From Allergy:
A higher concentration of secretory IgA in breast milk lowers the risk of milk allergy in the baby so it is the safest food for the baby
4. Therapeutic Effect:
- Breastfeeding protects the baby from E. coli infection due to high levels of bifidus factor in it. Lactoferrin present in breast milk protects the baby from enteric infections.
- It protects the baby from neonatal hypocalcemia and tetany ( due to its ideal calcium and phosphorous ratio ).
- Also, exclusively breastfed infants are at lower risk of developing diabetes mellitus, childhood lymphomas, liver diseases, and bronchial asthma later in life.
5. Physiological Adaptation:
- Mother’s milk is very suitable for the baby. The milk of a mother who has delivered a preterm baby is different from the milk of a term baby’s mother.
- Preterm mother’s milk contains more energy, protein, fat, sodium, zinc, anti-infective factors, and macrophages and has lower lactose, calcium, and phosphorous content.
6. Economic Factors:
- Breast milk is available free of cost for the baby. Also, it is safe and free from any contamination so there is no risk of infection to the baby.
- This ultimately reduces the cost of hospitalization and the economic burden of illness on the family.
7. Emotional Bonding:
- Breastfeeding promotes emotional and physical bonding between the mother and the baby.
- This leads to better child and mother relationships and fewer behavioral problems in children.
Advantages for Mother:
- Lactation suppresses ovulation in mothers who give exclusive breastfeeding to their infants and serves as a natural contraceptive.
- Breastfeeding lowers the risk of ovarian and breast cancer.
- Breastfeeding is convenient for the mother as she is not required to clean the bottle and prepare milk whenever she feeds the baby.
- Breastfeeding the baby helps the mother lose the extra weight that she had put in during pregnancy.
- Breastfeeding promotes the involution of the uterus, thus bringing back the mother in shape after delivery.
Question 8. Factors Inhibiting Breast Feeding
Answer:
The following factors may inhibit breastfeeding:
1. Psychological Factors:
Shock, strong pain, anger, anxiety, or worry can affect the patient. So the mother should be encouraged and supported to be calm, relaxed, and have a positive attitude while breastfeeding.
2. Early Breast Engorgement:
During and immediately after delivery, the breast may feel full and uncomfortable. Some mothers have hard, engorged, and painful breasts which makes feeding the baby difficult. This problem can be solved by applying of warm compress to the breast and then expressing excess milk.
3. Flat and Inverted Nipples:
- If the nipples are flat, it is difficult for the baby to get hold of the nipple and pull it into the mouth so sucking is interrupted.
- To overcome this, the flat or inverted nipple may be pulled outward with fingers to stimulate erection.
- After the erection of the nipple, the baby can be gently put to the breast. If not successful, a nipple shield may be used.
4. Sore Nipple:
- Nipples may be sore because of faulty sucking techniques such as the baby taking an insufficient amount of areola into the mouth while feeding.
- Nipples may become sore due to long periods of vigorous sucking, sucking in a bad position, engorged breasts, and oral thrush of the baby.
- This can be prevented by teaching the mother about proper breastfeeding techniques during the antenatal period.
- Mothers should decrease the length of feeding and increase the frequency of feeding. Also, mothers should avoid the use of soap on the breast as it causes drying.
- Any emollient like vaseline or edible oil should be applied to the nipples after feeding the baby.
Question 9. Complementary Feeding Or Weaning.
Answer:
Complementary Feeding Definition:
Complementary feeding or weaning is the process of giving an infant other foods and liquids along with breast – milk after the age of 6 months as breast milk alone is no longer sufficient to meet the nutritional requirements of the growing baby. It is the process by which the infant gradually becomes accustomed to an adult diet.
Guiding Principles for Complementary Feeding:
- Breast milk alone is not sufficient to meet the nutritional requirements of the baby after 6 months. Also, infants are developmentally ready to take other foods at about 6 months. By 6-8 months teeth eruption begins and the baby learns to bite and chew.
- The digestive system becomes mature enough to digest starch, protein, and fat in non – a non-medent diet. Very young infants push food out with their tongues, but by the age of 6-9 months, they are able to hold food in their mouths. Hence, 6 months is the recommended age for weaning.
- The energy needed in addition to breast milk is about 200 K.cal/day in infants of 6-8 months, 300 K.cal/day during 9-11 months, and 550 K.cal/day during 12-23 months of age.
So baby needs extra food in addition to breast milk:
Principle 1: Practice exclusive breastfeeding from birth up to 6 months of age and introduce complementary foods after 6 months of age along with breastfeeding.
Principle 2: Continue frequent on-demand breastfeeding until 2 years of age or beyond.
Principle 3:
- Practice responsive ( active ) editing by applying the principles of psychosocial care Feed infants slowly and patiently and encourage them to eat but do not force them.
- If the child refuses to eat any food, experiment with different food combinations, tastes, and textures. Minimize distractions during meals if the child loses interest easily.
Principle 4: Practice good hygiene and proper food handling to reduce the risk of diarrhea.
Principle 5: Start at 6 months of age with small amounts of food and increase the quantity as the child gets older while maintaining frequent breastfeeding.
Principle 6:
- Gradually increase food consistency and variety as the infant grows older, adapting to the infant’s requirements and abilities.
- Begin liquids at 6 months. By 8 months he can eat semi-solids and by 12 months he can eat solid foods as consumed by the rest of the family members.
Principle 7:
- Increase the number of times the child is fed complementary food, as the child gets older.
- A breastfed infant who is 6-8 months old needs 2-3 meals a day and at 9-23 months he needs 3-4 meals a day.
Principle 8:
- Feed a variety of nutrient-rich foods to ensure that all nutrient needs are met. Complementary foods should provide sufficient energy, protein, vitamins, iron, and micronutrients.
- Complementary food should include animal products, dairy products, pulses, fruits, vegetables, and oils.
Principle 9: Give micronutrient-rich complementary foods or vitamin and mineral supplements to the infant as needed.
Principle 10:
- It is advisable to start one or two teaspoons of new food at first which should be given when the baby is hungry, just before regular feeding, during day time.
- It may be continued for a few days until the child gets used to the same. Then the new food item may be started, one at a time.
Weaning Foods:
Examples of weaning foods that may be started according to the child’s ability to feed are:
- Liquids: Soup of vegetables, pulses, rice water, and fruit juices.
- Semi Solids: Mashed potato, pulses, boiled vegetables, mashed banana, soft cooked rice and fish.
- Solids: Cooked rice, chapati, idli, bread, biscuits, groundnuts, banana and fruits.
Problems during Weaning:
Several problems may be encountered during weaning, which is as follows
- If on starting weaning, breastfeeding is stopped suddenly, it can have adverse psychological effects on the child.
- Weaning food, if prepared unhygienically or not digested properly can cause diarrhea.
- If weaning foods are not nutrient-rich, the child can develop malnutrition.
- Children may develop indigestion, abdominal pain, diarrhea, or rashes if they are allergic to certain foods.
Question 10. BFHI
Answer:
The Healthy C Baby Friendly Hospital Initiative Baby Friendly Hospital Initiative ( BFHI ) was launched jointly by WHO and UNICEF in March 1992 to encourage and promote exclusive breastfeeding.
Bottle feeding is the biggest killer of babies so BFHI was launched to resurrect the dwindling practice of breastfeeding. BFHI aims to improve the knowledge, attitude, and practices of healthcare workers by providing them with knowledge and skills to promote exclusive breastfeeding among infants up to the age of 6 months. )
The following ten steps are recognized as minimum global criteria for attaining the status of a Baby Friendly Hospital:
Step 1:
- Have a written breastfeeding policy that is routinely communicated to all health staff.
- A written policy consisting of ten steps for successful breastfeeding should be displayed in the maternal and child health area of the hospital.
- The policy statement should be available both in English and the local language.
Step 2:
- Train healthcare staff in the skills necessary to implement this policy.
- The healthcare staff should get practical training to implement the ten steps of breastfeeding.
- They should be taught the skills needed to assist nursing mothers with the expression of breast milk, correct positioning, and attachment of babies during breastfeeding.
Step 3:
- Inform all pregnant women about the benefits and management of breastfeeding.
- During the antenatal period, mothers should be informed and educated about the advantages of breastfeeding for both mother and baby.
- Problems like retracted, small, or cracked nipples should be managed during the antenatal period.
Step 4:
- Help mothers to initiate breastfeeding within half – hour of birth.
- UNIT Establish mother-baby bonding soon after delivery and encourage all mothers to initiate breastfeeding within half hour of birth.
- Mothers should be advised not to administer pre-lacteal feeds.
Step 5:
- Show mothers how to breastfeed and how to maintain lactation if they are separated from their infants.
- Mothers should be taught the art of breastfeeding including position and technique of feeding.
- They should be taught the correct technique of expression of breast milk manually or with the help of a breast pump, in order to maintain adequate lactation.
Step 6:
- Give newborn infants no food or drink other than breast milk, unless medically indicated. No pre-lacteal feeds should be given to the newborn Only breastfeeding should be given.
- In case breast milk is not available supplementary feeding is given.
Step 7:
- Practice rooming in and allow mothers and infants to remain together round the clock.
- Keeping mother and newborn together promotes bonding between mother and baby and also helps in the timely initiation of breastfeeding
Step 8:
- Encourage breastfeeding on demand.
- Mothers should breastfeed the babies whenever they are hungry and not according to the clock
Step 9:
- Give no artificial feeds or pacifiers to the baby. Pacifiers should not be given to babies due to the risk of infection and non-nutritive sucking.
- Expressed breast milk or any other medically indicated fluid should be administered through Katori / spoon or malady but not feeding bottle
Step 10:
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital.
- Women breastfeeding support groups should be established in the community for the promotion of breastfeeding.
- Follow-up support for all breastfeeding mothers is necessary after they are discharged from the hospital.
BFHI movement is active in India under a National Task Force comprising of Government of India, UNICEF, WHO, Voluntary organizations, and many professional bodies
Question 11. Under-Five Clinic
Answer:
The concept of an Under-five Clinic is derived from the Well Baby clinic of the West, for comprehensive health care of children below five years of age. This clinic provides preventive services along with health supervision, treatment, nutritional surveillance, and health education
- The services are economical within available resources for a large number of young children
- Underfive age groups are vulnerable and special risk groups constituting a major portion of the total population with a high death rate
- The important causes of morbidity and mortality of this group are mainly, ARI, diarrhea, neonatal and perinatal diseases, infections, and accidents.
- These conditions are mostly preventable with adequate health care. This age group also needs regular monitoring for growth and development
- For these reasons, the under-five age group children are provided with special health care through this clinic’s services
- The services provided by the clinic are set out in the symbol, which has been proposed for under-five clinics in India.
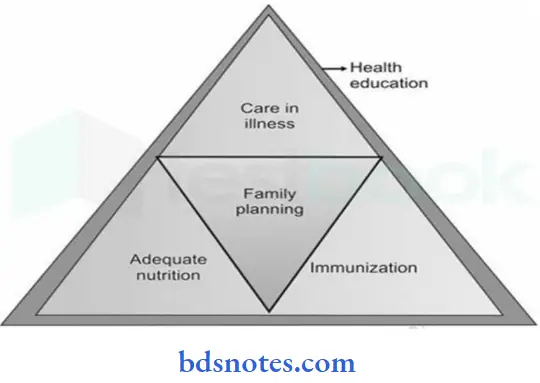
The apex of the large triangle represents care in illness, the left triangle represents adequate nutrition, the right triangle represents immunization and the central red triangle represents family planning. The line bordering the big triangle represents health teaching to the mother
Under-Five Clinic Care in Illness:
The care of illness for children provided in the under-5 – 5 clinics includes the following:
- Diagnosis and treatment of:
- Acute illness, for example, oral rehydration therapy
- Chronic illness including physical, mental, congenital, and acquired abnormalities
- Disorders of growth and development
- X-ray and laboratory services
- Referral services
Under-Five Clinic Adequate Nutrition:
- Adequate nutrition is vital for the growth and development of children. The health worker should ensure adequate breastfeeding, weaning, and balanced diet of the under – 5 children
- Almost all nutritional disorders like PEM, anemia, rickets, and nutritional blindness occur in this age group
- Attempts to be made to identify the early onset of growth failure and malnutrition. One of the basic activities of the under – fives clinic is growth monitoring It is done by weighing the child periodically at monthly intervals during the first year, every 2 months during the second year, and every 3 months thereafter up to the age of 5 to 6 years
- Food supplementation or on-site feeding is often an integral part of intervention strategies
- The ICDS projects have taken up the supplementary feeding of children below 6 years of age
- Nutrition education to mothers is an important aspect of the clinic
Under-Five Clinic Immunization:
- Immunization of six killer diseases, viz. tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, and measles, are administered as per national immunization schedule recommendation.
- The health worker should motivate and promote immunization acceptance to prevent morbidity, mortality, and disability hazards by these six killer diseases
Under-Five Clinic Family Planning:
- The family planning program is successfully conducted through these clinics.
- The mothers attending the clinic receive counseling on different aspects of family planning practices, which is a significant concern for the health and well-being of the child.
Under-Five Clinic Health Education:
- Health education for the mother is an essential and compulsory activity of the under-five clinic. The mothers should receive information on various aspects of child care and child-rearing practices.
- Preventive measures against malnutrition, ARI, diarrhea tuberculosis, worm infestations, etc. should be informed to the mothers to improve awareness about the disease and its prevention.
The under-five clinic is usually located in a village a slum or a labor colony. It is managed by trained health workers. She also visits home to educate the mothers and to make sure that children are brought to the clinic for regular check-ups.
She maintains child registers and records related to child care given and health check-ups done. She distributes supplementary food, vitamin ‘ A ’ oil, and iron-folic acid tablets and keeps accounts of expenditure. She arranges health exhibitions, well-baby competitions, and mothercraft training programs. Thus, ‘under-five’ clinics provide low-cost comprehensive care through preventive promotive, curative and rehabilitative healthcare services to under-five children
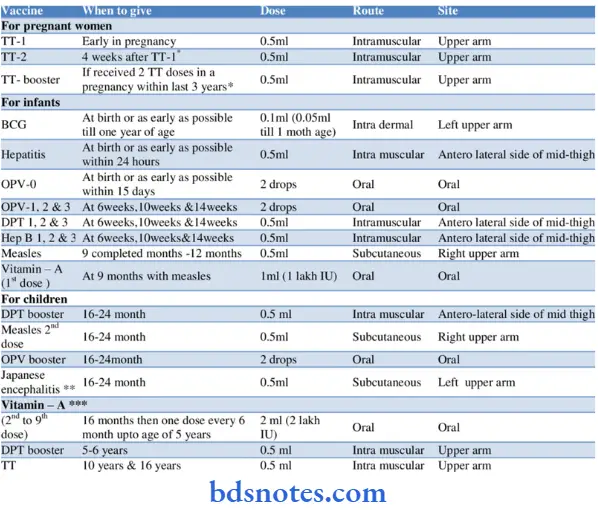
Question 12. National immunization schedule
Answer:
Question 13. Cold chain of vaccines.
Answer:
Cold chain of vaccines:
- The ‘ cold chain ’ is a system of storage, transport, and distribution of vaccines in the state of efficacy and potency at the recommended temperature from the manufacturer to the actual recipient of the vaccine.
- The failure of the cold chain system may lead to ineffective protection against vaccine-preventable diseases. Maintenance of the cold chain is the cornerstone for the success of the immunization program
- All vaccines must be stored, transported, and distributed at the recommended temperature by the manufacturer in the literature accompanying the vaccine, otherwise, they may become denatured and ineffective with loss of potency.
- For a successful cold chain system, three elements are essential, i.e. cold chain equipment, transportation system, and motivation and training of the workers for maintenance of the cold chain link. Among all vaccines, polio is the most heat sensitive, requiring storage at -20 ° C. Polio and measles vaccines must be stored in the freezer compartment.
- DPT, DT, TT, BCG, Typhoid, and diluents of vaccines must be stored in the cold part and never allowed to freeze. Vaccines must be protected from sunlight and contact with antiseptic. At the health centers, most vaccines, except polio, can be stored at 4 to 8 ° C for 5 weeks.
- Multidose opened vial, which is not used fully must be discarded, within one hour, if no preservative is present. It should be discarded within 3 hours or at the end of a session when a preservative is used. Necessary instructions for the particular vaccine must be followed regarding maintenance of the required temperature. Instruction for maintenance of vaccine vial monitor ( VVM ) especially for oral polio vaccine should be followed strictly
Cold Chain Equipment The cold chain equipment consists of the following:
- Walk-in Cold Rooms: At the regional level, vaccines are stored for 4 to 5 districts in the walk-in cold rooms (WIC), at recommended temperatures of upto 3 months
- Deep Freezers: A deep freezer is a top-opening cold chain equipment and is available as 300 liters or 140 liters capacity. Big deep freezer.
- Ice lined refrigerator
- Cold boxes
- Vaccine Carrier
- Day carriers
- Ice packs
Question 14. Define play and types of play
Answer:
Play:
Just as adults work, so does the child play. It is the main business of the child. Through play the child grows, develops, leams, and ultimately matures. Play is the child’s daily work
Play Definition:
Play is an activity in which anyone is engaged for enjoyment without considering its end results
Play Types :
There are different types of play suitable for young children.
All types of play can be categorized into two:
- Active play
- Passive play
Active play means children get enjoyment from what they do, whereas in passive play children get enjoyment from watching or listening to someone. Passive play is also known as amusement
1. Types of Active Play:
Exploratory Play:
- A young child’s first interest in play is exploratory. The child looks at a toy, shakes it, pounds it to see what noise it makes, sucks it, smells it, and squeezes it to see how it feels. Young children enjoy these exploratory activities.
- They also learn things that they can learn in no other way except by play
Construction:
- By the time a child is 3 years old, he is no longer satisfied with exploring toys. Children of this age want to use toys to make things.
- Instead of throwing or biting the blocks, these young ones use them to build towers, bridges, trains, etc. fit
Dramatic Play:
- Just about the time, young children begin to use toys to construct things; they discover that it is fun to dramatize with toys. To these young children, a doll is not just a doll; it can be a teacher, a mother, or a woman.
- A toy phone can be used to call and talk with someone. With a few articles and clothing, children can quickly turn into any character in drama
Family Games:
- Before the babies are 2 years of age, they like to play simple games with family members. These games have very few rules and are usually played with any of the family members.
- The traditional family games for babies are peek-aa-boo, ‘ Guess which hand? finding a hidden object etc.
Neighborhood Games:
- By the age of 4-5 years, children begin to lose interest in family games. Now they want to play with children of their age.
- These children are usually from the neighborhood. These games are a little more complicated than family games.
2. Types of Passive Play
The enjoyment comes from watching or listening to others. Amusement is ideal when the child is tired and yet needs something to avoid boredom and restlessness
Passive play is of the following types:
- Watching Others: No matter how simple an activity is, young children are fascinated by watching people do it. They like to watch parents and other adults do things in-house. Watching others helps children learn how to do things and learn new meanings
- Looking at pictures: Bright-colored pictures in books, comics, magazines, and newspapers greatly appeal to young children. Besides the enjoyment that they get from looking at picture, they also learn new words and meanings. They learn to associate words with their meaning
- Listening Stories
Question 15. Advantages or Benefits of Play
Answer:
Advantages / Benefits of Play:
1. Sensory Motor Development: Sensory-motor activity is a major component of play at all ages
- It has the following benefits:
- It serves as an outlet for extra energy
- It helps in muscle development
- It gives the child a chance to learn body control
- It helps the child develop hand and eye coordination
- It helps children to learn increasingly complex and coordinated activities such as races, games, roller skating, bicycle riding, etc.
2. Intellectual Development:
- Through play children develop the ability to keep their minds on the task at hand
- Play gives children a chance to discover the meaning of things in the environment
- Through play, children learn about colors, shapes, sizes, textures, etc. Play helps children develop an understanding of abstract concepts and spatial relationships such as up, down, under, over, etc.
- Play helps children to differentiate between fantasy and reality.
- It helps in language development
3. Social Development:
- Play helps children in socialization. Through play, they learn to make friends and get along with others
- Play gives children a chance to learn to be a good sport a good loser or a winner
- It helps children learn the acceptable standards and norms of society
- It helps children learn to take responsibility for their actions
4. Creativity:
- Play encourages creativity in children
- Play gives children an opportunity to experiment and try out their ideas through all the available things like clay, clothes, etc.
Therapeutic Value:
- Play provides a way to get rid of anger, fear, jealousy and grief
- It is a means for the release of stress and tension
- It increases appetite
- It leads to healthful sleep Through play, children can communicate their needs, fears, and desires that they are unable to express with their limited language skills
Moral Value:
- Though children learn at home and school those behaviors considered right or wrong, the interaction with peers during play contributes significantly to their moral training
- To maintain a place in the playgroup children learn to conform to the standards of the group
- Through play, children learn acceptable behaviors like fairness, honesty, self-control, tolerance, etc.
Question 16. Explain the Selection of Toys.
Answer:
Selection of Toys Play things or toys should be provided based on the child’s age, personality, abilities, interests as well as safety. While buying toys for children, parents must keep in mind the child’s physical, intellectual, and emotional abilities.
Toys should be challenging or should offer problem-solving opportunities, but children must be old enough to master the skills required to play with them. Toys should teach new skills and leave room for children to use their imaginations
While selecting toys for children, parents should keep in mind the following:
- Toys should not have sharp edges that can cut
- Toys should not have sharp points that can puncture
- Toys should not have propelling parts that can injure eyes.
- Toys should not have small parts that children can swallow or inhale.
- For children under 3 years of age, any toy or part of the toy that is smaller than 1.25 inches in diameter and 2.25 inches in depth is dangerous and should not be given
- For infants avoid toys with strings that are 7 inches or longer, since they may cause strangulation
- Toys that produce excessive noise should be avoided as they can cause hearing loss
- Select toys that are light enough and will not cause any harm even if they fall on the child
- Make sure that the materials used in toys are non-toxic.
- For all children less than 8 years old, avoid electric toys.
- Select toys that are durable enough to survive rough handling by children
- Avoid toys made up of glass. Children must be taught about the correct use of toys. Also, they must be instructed about the maintenance and storage of their toys
Question 17. Play Therapy
Play Therapy Introduction:
Play therapy is generally employed with children aged 3-11 years It provides a way for them to express their experiences and feelings through a natural and self-guided process
Play Therapy Definition:
Play therapy is a form of counseling or psychotherapy that uses play to communicate with children and help them resolve psychosocial challenges. It can also be defined as a technique whereby the child’s natural means of expression i.e. play, is used as a therapeutic method to assist him/her in coping with emotional stress or trauma.
Play Therapy Types :
Play therapy can be conducted following different schedules which are as follows:
1. Individual versus Group Play Therapy:
- Individual play therapy is useful to cater special requirements of each child. In this type, the play therapist’s attention is focused on one child only, to help him solve his problems.
- Some children do not respond well to Individual play therapy as their problems are of such a nature, for example, shyness, where Individual Play therapy might be difficult.
- For such children, Group Play Therapy is used where other children are utilized to draw the child out of his problems
2. Spontaneous or Free Versus Controlled or Situational Play Therapy:
- In spontaneous play therapy, the child is free to decide what toys he wants to play with, the mode of play, expression of emotions, and interaction with play therapists and those around him.
- This form of therapy is very useful in aggressive children. In controlled play therapy, the child is provided with a situation or setting and his reactions in that situation are noted.
- This form of therapy gives the child a chance to reflect on his conflicts through the characters that he plays in a given play situation
3. Structured Versus Unstructured Play Therapy:
In Structured Play Therapy planned situations are used to obtain information about the child’s behavior In unstructured play therapy no situation is set and no plans are followed, the child is left free to play
4. Directive Versus Non-Directive Play Therapy:
In Directive play therapy, the play therapist sets directions for the child to play. The play therapist makes suggestions and interpretations of the child’s words and actions. In non-directive play therapy, the child receives no directions from the therapist. The child is allowed to play according to his wish
Play Therapy Team:
Many people in the health team serve as play therapy team like:
- Child psychologist
- Trained play leader
- Child specialist or pediatrician.
- Nurse.
- Social worker or Counsellor.

Leave a Reply