Chapter 3 Infection Control Questions and Answers
Question 1. Sources of infection
Answer:
Infection and immunity involve interaction between the animal body (host) and the infecting microorganisms. The lodgement and multiplication of a parasite in or on the tissues of a host constitute infection. It does not invariably result in disease.
Sources Of Infection
- Human beings
- Animals
- Insects
- Soil and water
- Food.
1. Human Beings: The most common source of infection for human beings is human beings themselves. The parasite may originate from a patient or carrier.
Humans serving as the microbial reservoir:
- Acquisition of “strep” throat through touching
- Hepatitis by blood transfusions
- Gonorrhea, syphilis, and AIDS by sexual contact
- Tuberculosis by coughing; and the common cold through sneezing.
2. Animals
- Reservoir hosts: Many pathogens are capable of causing infections in both human beings and animals. Therefore, animals may act as a source of infection of such organisms. These, animals serve to maintain the parasite in nature and act as a reservoir and they are, therefore, called reservoir hosts.
- Zoonosis: The diseases and infections, which are transmissible to man from animals are
called zoonosis.- Examples of zoonotic diseases
- Bacterial: Anthrax, brucellosis, Question fever, leptospirosis, bovine tuberculosis, bubonic plague,
Salmonella food poisoning. - Viral: Rabies, yellow fever, cowpox, monkeypox.
- Protozoal: Leishmaniasis, toxoplasmosis, trypanosomiasis, babesiosis.
- Helminthic: Echinococcosis, taeniasis, trichinellosis.
- Fungal: Microsporum canis, Trichophyton verrucosum.
3. Insects:
Arthropod-Borne Diseases: Blood-sucking insects, such as mosquitos, ticks, mites, ies, and lice may transmit pathogens to human beings, and diseases so, caused are called arthropod-borne diseases.
Insects Vectors: Insects that transmit infections are called vectors. Vector-borne transmission can be of two types either mechanical (external) or biological (internal).
Mechanical vector: The disease agent is transmitted mechanically by the arthropod.
Mechanical vector Examples: Transmission of diarrhea, dysentery, typhoid, food poisoning, and trachoma by the house.
Biological vectors: Biological vectors are those in whom the pathogens multiply sufficiently or has undergone a developmental cycle. The interval between the time of entry of the pathogen into the vector and the vector becoming infective is called the extrinsic incubation period.
Biological vectors Examples: Aedes aegypti mosquito in yellow fever, Anopheles mosquito in malaria.
Reservoir hosts: Besides acting as vectors, some insects may also act as reservoir hosts (for example, ticks in relapsing fever and spotted fever). Infection is maintained in such insects by transovarial or transstadial passage.
4. Soil And Water
Soil: Some pathogens can survive in the soil for long periods.
Soil Examples
- Spores of tetanus and gas gangrene: Spores of tetanus and gas gangrene remain viable in the soil for several decades and serve as source of infection.
- Fungi and parasites: Fungi (causing mycetoma, sporotrichosis, histoplasmosis) and parasites such as roundworms and hookworms also survive in the soil and cause human infection.
Water: Water may act as the source of infection either due to contamination with pathogenic microorganisms (Shigella, Salmonella, Vibrio cholerae, poliomyelitis virus, hepatitis virus) or due the presence of aquatic vector (cyclops containing larvae of guinea worm infection).
5. Food: Contaminated food may act as source of infection of organisms causing food poisoning, gastroenteritits, diarrhea and dysentery.
Question 2. Classification of infection.
Answer:
The lodgement and multiplication of a parasite in or on the tissues of a host constitute infection. It does not invariably result in disease.
Classification Of Infections: Infections may be classied in various ways
- Primary infection: Initial infection with a parasite in a host is termed primary infection.
- Reinfections: Subsequent infections by the same parasite in the host are termed reinfections.
- Secondary infection: When a new parasite sets up an infection in a host whose resistance is lowered by a preexisting infectious disease, this is termed secondary infection.
- Local infection: The term local infection (more appropriately local sepsis) indicates a condition where, due to infection or sepsis at localized sites such as appendix or tonsils, generalized effects are produced.
- Cross-infection: When in a patient already suffering from a disease, a new infection is set up from another host or another external source, it is termed cross-infection.
- Nosocomial infections: Cross-infections occurring in hospitals are called nosocomial infections (from Greek nosocomion hospital).
- Iatrogenic infection: The term iatrogenic infection refers to physician induced infections resulting from investigative, therapeutic or other procedures.
- In apparent infection: In apparent infection is one where clinical effects are not apparent.
- Subclinical infection: The term subclinical infection is often used as a synonym to in apparent infection.
- Atypical infection: Atypical infection is one in which the typical or characteristic clinical manifestations of the particular infectious disease are not present.
- Acute infection: An infection which lasts for a relatively short time. (few days to few weeks). Example: Measles.
- Chronic infection: An infection which lasts for a long time (over months and years). Example: TB.
- Autoinfection: An infection that occurs between two sites on the same host.(worms)
- Mixed infection: An infection caused by two or more organism.(bacterial vaginosis)
- Masked infection: An infection is known to occur but the infectious agent cannot be demonstrated.
- Oppurtunistic infection: An infection with organisms which are normally harmless but become pathogenic when the body’s defence mechanisms are compromised.
Question 3. Define carrier and its classification with examples.
Answer:
Carrier: A carrier is person who harbours or lodge of the microorganisms without suffering from any ill effect because of it. There are several types of carriers:
- Convalescent carrier: An individual who has recovered from the infectious disease but continues to harbour or lodge large numbers of pathogen.
- Healthy carrier: A healthy carrier is an individual who harbours or lodge the pathogen but is not ill.
- Incubatory carrier: An incubatory carrier is an individual who is incubating the pathogen in large numbers but is not yet ill.
- Temporary carriers: Convalescent, healthy, and incubatory carriers may harbour or lodge the pathogen for only a brief period (hours, days, or weeks) and lasts less than six months.
- Chronic carriers: They harbour the pathogen for long periods (months, years, or life).
- Contact carriers: The term contact carrier is applied to a person who acquires the pathogen from a patient.
- Paradoxical carrier: This refers to a carrier who acquires the pathogens from another carrier.
Question 4. Modes of transmission of infection
Answer:
Modes Of Transmission Of Infection: Pathogenic organisms can spread from one host to another by a variety of mechanisms.
These include as follows:
Contact: Infection may be acquired by contact, which may be direct or indirect.
- Direct contact: Diseases transmitted by direct contact include STD (sexually transmitted diseases), such as syphilis, gonorrhea, lymphogranuloma venereum, lymphogranuloma inguinale, trichomoniasis, herpes simplex type 2, hepatitis B and acquired immunodeciency syndrome (AIDS).
- Indirect contact: Fomites: Indirect contact may be through the agency of fomites, which are inanimate objects, such as clothing, pencils or toys which may be contaminated by a pathogen from one person and act as a vehicle for its transmission to another.
Inhalation – Droplet nuclei: Respiratory infections, such as the common cold, influenza, measles, mumps, tuberculosis, and whooping cough are acquired by inhalation.
Ingestion
- Intestinal infections are generally acquired by the ingestion of food or drink contaminated by pathogens. Infection transmitted by ingestion may be waterborne (cholera), foodborne (food poisoning), or handborne (dysentery).
- Diseases transmitted by water and food include chiey infections of the alimentary tract, for example, acute diarrheas, typhoid fever, cholera, polio, hepatitis A, food poisoning, and intestinal parasites.
Inoculation: The disease agent may be inoculated directly into the skin or mucosa, for example, rabies virus deposited subcutaneously by dog bite, tetanus spores implanted in deep wounds, and arboviruses injected by insect vectors. Infection by inoculation may be iatrogenic when unsterile syringes and surgical equipment are employed. Hepatitis B and the human immunodeciency virus (HIV).
Insects – Vector-Borne: Vector is denied as an arthropod or any living carrier (for example: nail) that transports an infectious agent to a susceptible individual. In some diseases, blood-sucking insects play an important role in the spread of infection from one individual to another.
Congenital-Vertical Transmission: Some pathogens are able to cross the placental barrier and reach the fetus in utero. This is known as vertical transmission.
Congenital Examples: So-called TORCH agents (Toxoplasma gondii, rubella virus, cytomegalovirus, and herpes virus), varicella virus, syphilis, hepatitis B, Coxsackie B, and AIDS.
Question 5. Aseptic techniques
Answer:
The methods which are used to prevent the access of microorganisms during the preparation of parenteral products and their testing are called ‘ Aseptic Techniques’. Aseptic techniques are used to reduce the risk of post-procedure infections and to minimize the exposure of healthcare providers to potentially infectious microorganisms. Aseptic techniques include practices performed just before, during, or after any invasive procedures.
- Good aseptic techniques can only be applied if one knows the possible sources of contamination. The various sources of contamination are – Atmosphere, which is contaminated with dust, droplet and droplet nuclei becomes the breeding ground of microorganism.
- The hands are a major means of transmitting infection. Coughing, sneezing, and spitting can cause contamination at a considerable distance. The cloths which absorb dust particles are also a source of contamination.
- A handkerchief is the richest source of contamination. The hair, which is constantly exposed to atmospheric dust is source of contamination. These dust particles are liberated from the hair during brushing and shaking of the head.
- The unsterile equipment. The working surface.
Question 6 Characteristics of an ideal disinfectant.
Answer:
Disinfectants: Chemicals that kill vegetative bacteria, fungi, viruses, and rarely bacterial spores.
- It should have a wide spectrum of activity.
- It should have fast action.
- It should be able to destroy infectious agents in clean as well as dirty condition.
- It should dissolve easily.
- It should have high penetration power.
- It should be non-toxic and non-irritant.
- It should not stain tissues.
- It should not have an unpleasant odour.
Question 7. Define disinfection. Write down the applications of most commonly used disinfectants. Or Enumerate any 4 chemical disinfectants.
Answer:
Disinfectants: Chemicals that kill vegetative bacteria, fungi, viruses, and rarely bacterial spores.
The various chemical disinfectants are:
1. Phenol and Related compounds:
- Phenol also called carbolic acid is the first chemical agent used as an antiseptic introduced by
Lord Joseph Lister (1854). - Phenol causes cell membrane damage and cell lysis. Phenol(1%) has bactericidal action but it is readily absorbed by skin and mucous membranes and causes toxicity.
- Thus it has been restricted and has been replaced by chemically related compounds like cresol, chloroxylenol, and chlorohexidine which are widely used as antiseptics.
Cresol: It is used as a solution of cresol in soaps(Lysol). It is used for disinfection of infected glassware. In laboratory disinfection of excreta, cleaning floors of wards and operation theatres.
Chloroxylenol: It is active ingredient of Dettol.
Chlorohexidine: It is bactericidal at high dilution. It is an active ingredient of Savlon which is widely used in burns, wounds, pre-operative disinfection of skin, etc.
2. Halogens: Chloride and Iodine are used as disinfectants being strong oxidizing agents.
Iodine: Used as skin disinfectant in the form of iodophores. A tincture of iodine (1-2% iodine in 70% alcohol) is used for cleaning or disinfecting skin and treating skin injuries. It is virucidal, herbicidal, and active against Tubercle bacilli.
Chlorine: Used widely as water disinfectant(0.5 to 1.0 milligrams per liter of water is effective). Products containing calcium hypochlorite are used for sanitizing utensils in restaurants. Sodium hypochlorite is used as a disinfectant for laboratory gloves, linen, syringes, and reagent
bottles.
3. Aldehydes: Two aldehydes are of considerable importance:
Formaldehyde:
- It is bactericidal, sporicidal and virucidal.
- It can be used in gaseous form or an aqueous solution.
- The gaseous form of formaldehyde is used for disinfection of rooms and for fumigation of operation theatres.
- A 10% solution of formalin (Formaldehyde gas + methanol) is used for killing bacterial cultures and suspension, cleaning contaminated surfaces, metal instruments and preservation of tissues for histopathological examination.
- It is also used to sterilize bacterial vaccines and in preparation of toxoid from toxin.
Glutaraldehyde:
- It is more effective and less irritant (toxic) than formaldehyde.
- It is active against bacteria (especially tubercle bacilli) and their spores, fungi, and various types of viruses including HIV and Enteroviruses.
- Glidex(2% buffered solution) is a commercial preparation used to sterilize cystoscopes, bronchoscopes, rubber anesthetic tubes, thermometers, polythene tubing, etc.
4. Alcohols: Pure alcohol has no disinfecting property. Three kinds of alcohols used as disinfectants are
Ethyl alcohol(ethanol): EA in a concentration between 50-70% is effective against viruses.
Methyl alcohol(methanol): Effective against fungal spores but it is toxic to eyes. Used for treating cabinets and incubators affected by spores.
Isopropyl alcohol(50-70%): Better than ethyl alcohol in bactericidal property used for disinfection of clinical thermometers.
5. Dyes: Two groups of dyes (aniline dyes and acridines) have been extensively used as skin and wound antiseptics. Both these groups are bacteriostatic in high dilution but have low bactericidal activity.
Aniline dyes: Include malachite green, brilliant green, and crystal violet. They are used on skin and mucous membranes as antiseptics and have been also used for some fungal infections like oral thrush.
Acridine dyes: Includes acriflavine, proflavine, aminacrine and euflavine. They are bacteriostatic and used for treating wounds and for irrigation of bladder and vagina.
Question 8. Standard safety measures.
Answer:
Standard Safety Measures Definition: Standard safety measures standard precautions or universal precautions are simple set of effective practices designed to protect health workers and patients from infection with a range of bloodborne and other pathogens from both recognized and unrecognized sources.
These practices are used when caring for all patients regardless of diagnosis. These rules are:
- Single-use disposable injection equipment.
- Discard contaminated sharps immediately in puncture or leak-proof containers.
- Do not recap needle or use the hand technique for recapping.
- Do not wash or disinfect latex gloves.
- Handle soiled linen correctly(cleaning with detergent and hot water).
- Disinfect instruments and surface areas.
- Hand hygiene/Hand washing: Hand hygiene is a major component of standard precautions and one of the most effective methods to prevent transmission of pathogens associated with health care.
- Standard Safety Measures Technique:
- Hand washing(40-60sec): Wet hands and apply soap; rub all surfaces rinse hands and dry thoroughly with a single use towel use towel to turn off the faucet.
- Hand rubbing(20-30sec): Apply enough product to cover all areas of the hands and rub hands until dry.
- Hand washing should be done
- Before and after any direct patient contact and between patients, whether or not gloves are worn.
- Immediately after gloves are removed.
- Before handling an invasive device.
- After touching blood, body fluids, secretion, excretions, non-intact skin, and contaminated items, even if gloves are worn.
- During patient care, when moving from a contaminated to a clean body site of the patient.
- After contact with inanimate objects in the immediate vicinity of the patient.
- Standard Safety Measures Technique:
- Wear Protective barriers: Gloves
- Wear when touching blood, body fluids, secretions, excretions, mucus membranes, and nonintact skin.
- Change between tasks and procedures on the same patient after contact with potentially infectious material.
- Remove after use, before touching non-contaminated items and surfaces, and before going to another patient. Perform hand hygiene immediately after removal.
- Prevention of needle sticks and injuries from other sharp instruments:
- Use care when:
- Handling needles, scalpels, and other sharp instruments or devices.
- Cleaning used instruments.
- Disposing of used needles and other sharp instruments.
- Use care when:
- Respiratory hygiene and cough etiquette: Persons with respiratory symptoms should apply source control measures: Cover their nose and mouth when coughing/ sneezing with tissue or mask, dispose of used tissues and masks, and perform hand hygiene after contact with respiratory secretions.
- Enviromental cleaning: Use adequate procedures for the routine cleaning and disinfection of environmental and other frequently touched surfaces.
- Linens:
- Handle, transport, and process used linen in a manner which:
- Prevents skin and mucus membrane exposures and contamination of clothing.
- Avoid transfer of pathogens to other patients and or the environ
- Waste disposal:
- Ensure safe waste management.
- Treat waste contaminated with blood, body fluids, secretions, and excretions as clinical waste, in accordance with local regulations.
- Human tissues and laboratory waste that is directly associated with specimen processing should also be treated as clinical waste.
- Discard single-use items properly.
Question 9. Define sterilisation. Describe in detail about sterilization by heat.
Answer:
Sterilization: Sterilization is a process by which an article, surface, or medium is freed of all living microorganisms including viruses, bacteria, their spores, and fungi.
Sterile: Material is heated in such a way that it contains no living organisms is said to be sterile.
Sterilization Physical methods:
- Sunlight
- Drying
- Heat:
- Dry heat: Red heat, Flaming, Incineration, Hot air oven.
- Moist heat: Temperature below 100°C,
- Temperature at 100°C
- Temperature above 100°C
- Filtration
- Radiation
- Sonic and Ultrasonic vibrations.
1. Sunlight: Direct sunlight has a sterilizing effect due to combined effect of UV rays and heat rays.
It has bactericidal effect and is one of the natural methods of sterilization of water in rivers, lakes, and tanks.
It is used to sterilize blankets, bedding, clothes, utensils, bedpans, etc. It is experimentally proved that typhoid bacilli when exposed to the sun on a piece of white drill cloth were killed in two hours, whereas bacteria remain alive in the dark even after six days.
2. Drying Or Desiccation: Moisture is essential for the growth of bacteria, so drying in air has deleterious effects on many bacteria. However, spores are unaffected and can remain alive for several month or even years. Therefore, it is not an ideal method of sterilization
3. Heat: Most common and one of the most effective methods of sterilization. Factors influencing sterilization by heat are
- Nature of heat
- Dry
- Moist
- Temperature and time
- Number of organism present
- Characteristics of organism such as species and sporing capacity.
- Type of material from which organism is to be eradicated
Dry Heat: Dry heat kills microorganisms by causing destructive oxidation of essential cell constituents. The various methods of dry heat sterilization include:
- Red Heat: It is used to sterilize metallic objects by holding them on the flame of a Bunsen burner till they are red hot.
- Read Heat Example: inoculating wires, needles, forceps spatulas, etc.
- Flaming: The article is passed over the flame of a Bunsen burner for few(3-4) times without allowing it to become red hot or stand too long.
- Flaming Example: Glass slides, the mouth of culture tubes and bottles, cover slips, scalpels, blades, and needles.
- Incineration: It is the process of complete burning of disposable wastes and some biomedical wastes in an electric furnace known as an “Incinerator”. It is the best method to decontaminate the destroying material and disposal of biochemical wastes. It is useful in the disposal of:
- Soiled dressings, swabs.
- Soiled paper and mouth wipes.
- Animal carcasses.
- Human anatomical waste.
- Pathogenic materials.
- Hot air oven: The hot air oven is made up of a double-walled steel chamber with the stout door.
- The top or side contain a ventilator which is left open during sterilization, to disperse any
moisture. - Air circulates within the oven by convention currents. This is most widely used method of sterilization by dry heat.
- The top or side contain a ventilator which is left open during sterilization, to disperse any
Moist heat: Sterilization by moist heat implies killing microorganisms by steam or hot water. Moist heat kills microorganisms by denaturation and coagulation of proteins. Moist heat in sterilization has 3 temperature ranges
- Temperature below 100°C
- Temperature at 100°C
- Temperature above 100°C
4. Filtration
- This method is used for sterilization of liquid substances or fluids such as sera and solutions of heat liable substances such as sugars, urea, enzyme, and antibiotics which get damaged by heat process. The method is also used for separation of bacteriophages and bacterial toxins from bacteria.
- The spore size is not less than 0.75m in diameter and it retains bacteria but allows viruses to pass
through filtrate. Therefore filtered preparations are not safe and cannot be employed for clinical use.
5. Irradiation: Radiation used for sterilization is of two types Ionizing radiation, for example, X-rays, gamma rays, and high-speed electrons. Non-ionizing radiation, for example, ultraviolet light, and infrared light. These forms of radiation can be used to kill or inactivate microorganisms.
Question 10. Describe the principle of an autoclave.
Answer:
Autoclave:
“An autoclave is a modified pressure cooker in which sterilization by saturated steam under high pressure is achieved (autoclaving)”. An autoclave may be horizontal or vertical. It is a double-walled or jacketed chamber (outer chamber) made up of stainless steel or gun metal with supporting frame.
- The steam circulates within the jacket and is supplied under high pressure to closed inner chamber where articles for sterilization are kept.
- One-fifth of the cylinder is filled with water, materials to be sterilized are kept inside, lid is closed and heater is put on. vThe safety valve is adjusted to required pressure (15psi/inch square).
- The boiling of water inside the chamber after some time results in steam which is allowed to escape with air mixture till the cylinder becomes air-free.
- The discharge tap is closed and the desired pressure inside in chamber is allowed to rise to the one chosen for autoclaving for a fixed time thus complete sterilization is achieved.
- One-fifth of the cylinder is filled with water, materials to be sterilized are kept inside, the lid is closed and the heater is put on. The safety valve is adjusted to the required pressure (15psi/inch square).
Read And Learn More: Bsc Nursing 1st Year Microbiology Previous year Question and Answers
- The boiling of water inside the chamber after some time results in steam which is allowed to escape with air mixture till the cylinder becomes air free.
- The discharge tap is closed and the desired pressure inside in chamber is allowed to rise to the one chosen for autoclaving for a fixed time thus complete sterilization is achieved.
- Satisfactory autoclaving or sterilization can be achieved at 15 pounds per square inch(psi) pressure which is equivalent to 121°C of temperature and the time of operation is 15-20 min.
- At this temperature, most of the heat-resistant spores are killed which cannot be achieved by other sterilization methods.
- However, sterilization can also be done at higher temperatures, at 126°C(20 lbs pressure/inch square) for 10 min or at 133°C(30 lbs pressure/inch2) for 3 min.
- Autoclaving is ideal method of destruction of bacterial spores. It is used to sterilize culture media, rubber goods, syringes, gowns, dressing, linen, gloves,
etc.
Question 11. Categories of Biomedical waste.
Answer:
Biomedical Waste Definition: Biomedical waste means any solid or liquid waste that is generated during the diagnosis, treatment, or immunization of human beings or animals, in research activities, or in the production or testing of biological products.
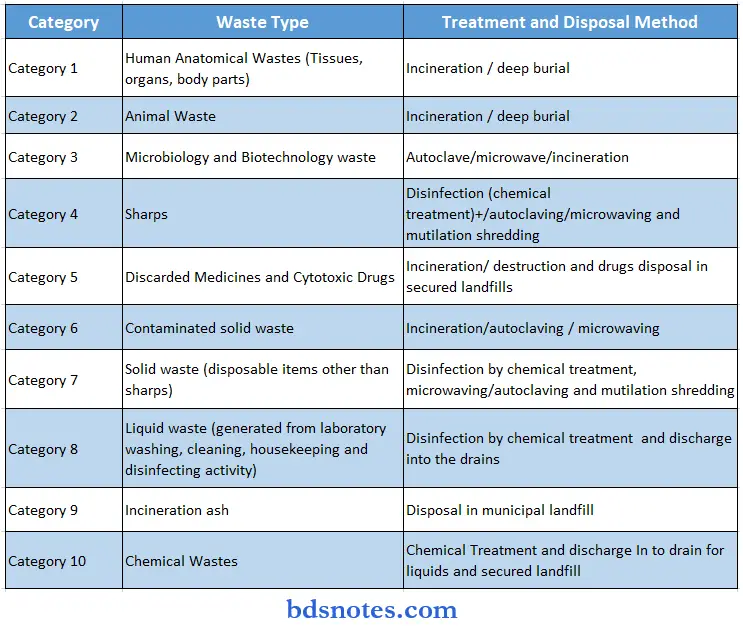
Question 12. Disposal of Biomedical waste.
Answer:
Disposal Of Biomedical Waste Definition: Biomedical waste means any solid or liquid waste that is generated during the diagnosis, treatment, or immunization of human beings or animals, in research activities, or in the production or testing of biological products.
Different methods of treatment and disposal are:
1. Incineration: Incineration is a method of treating waste that involves the combustion of the organic substances found in waste materials.
- The key difference between combustion and Incineration is that combustion includes the reaction between substances and oxygen, which produces energy, whereas incineration is the destruction of something via burning.
- However, incineration gives ash, flue gas, and heat as the final product. Three types of waste to which incineration is applied extensively are municipal solid waste, hazardous waste, and medical waste. Incineration of those three types is the focus of this discussion.
2. Autoclave: An autoclave is a machine that uses steam under pressure to kill harmful bacteria, viruses, fungi, and spores on items that are placed inside a pressure vessel.
- The items are heated to an appropriate sterilization temperature for a given amount of time.
- An autoclave is used to sterilize surgical equipment, laboratory instruments, pharmaceutical items, and other materials. It can sterilize solids, liquids, hollows, and instruments of various shapes and sizes.
3. Microwave irradiation: Microwave irradiation involves electromagnetic wave in the range of 300 MHz–300 GHz. Typical microwave ovens or microwave reactors work at a frequency of 2.45 GHz. Microwave irradiation produces efficient internal heating by direct coupling of microwave energy with the molecules of biomass.
4. Inertization: Inertization, or inerting, is an explosion protection process that uses inert gas to prevent the formation of an explosive mixture.
- Inerting systems are used to prevent: vapors from escaping into the atmosphere (contamination) and air from penetrating into the plant (oxidation). inert gases are non-combustible, non-flammable, and non-reactive to many materials.
- Examples include argon, helium, nitrogen, and neon. Some inert gases are also cryogenic in their liquid state.
5. Chemical Disinfection: Chemical disinfection consists of adding a disinfectant (generally a strong oxidant) to the water, which reacts with the organic matter and microbial organisms.
- The most frequent chemical disinfection compounds are chlorine dioxide, chlorine, and chloramines on one hand, and ozone on the other hand.
- These include alcohols, chlorine and chlorine compounds, formaldehyde, glutaraldehyde, ortho-phthalaldehyde, hydrogen peroxide, iodophors, peracetic acid, phenolics, and quaternary ammonium compounds.
6. Land Disposal Definition: The discharge, deposit, or injection of any waste onto or into the soil or other land surfaces.
- Landfills are sites designated for dumping rubbish, garbage, or other sorts of solid waste. Historically, they are the most common means of disposing of solid waste which is either buried or left to pile in heaps.
- Some landfills are well-managed and designed as part of integrated waste management.
Question 13. What is nosocomial infection? Describe various types of nosocomial infections in detail.
Answer:
Hospital-acquired infection (HAI)/nosocomial infection — is an infection that is contracted from the environment or staff of a healthcare facility.
- The term Nosocomial is taken from the Greek word Nosocomium meaning healthcare facility.
- It is also known as hospital-acquired infection.
- Nosocomial infection is one that is acquired in a hospital or health care agency.
- A hospital is one of the most likely places for acquiring an infection because it harbors high population of viral and strains of microorganisms that are usually resistant to do antibiotics.
Types of hospital Acquired Infection
- Bloodstream infection: This includes bacteria and septicemia which are generally caused by the introduction of intravascular catheter cannulas.
- Pneumonia -ventilator-associated pneumonia(VAP) in ICU patient patients with prior respiratory tract pathology smokers patients who have undergone abdominal of thoracic surgery are usually affected.
- Urinary tract infection it is usually caused by the introduction of eggs in organisms’ urinary tract catheter for urinary tract instrumentation.
- Gastrointestinal infection it can occur by the consumption of contaminated food and cause food poisoning manifested by vomiting diarrhea or dysentery.
- Skin and soft tissue infection it can occur by surgical procedures contamination of wounds and secondary infection of traumatic wound Examples of positive microorganisms
Question 14. Define hospital-acquired infection. Write a note on hospital infection control committee or program.
Answer:
Hospital-acquired infection (HAI)/nosocomial infection — is an infection that is contracted from the environment or staff of a healthcare facility.
- The term Nosocomial is taken from the Greek word Nosocomium meaning healthcare
facility. - It is also known as hospital-acquired infection. Nosocomial infection is one that is acquired in hospital or health care agency.
- This committee bears the responsibility of infection control measures with an objective of reducing the risk of HAI in the hospital. The committee discusses and decides on each matter that can have an effect on infection control.
Hospital-acquired Infection Roles And Responsibilities
- Develop and approve organization-wide infection control programs, policies, activities, and manual
- Establish standard precaution practices to be followed across the hospital
- Establish definitions and criteria for identifying and reporting of all infections among patients and personnel
- Guide departments on evidence-based infection control practices
- Set benchmark HAI rates for monitoring the effectiveness of infection control measures
- Validate methods for calculating HAI rates
- Review HAI rates periodically and recommend actions accordingly
- Develop antibiotic policy in conjunction with the pharmaco-therapeutics committee
- Develop protocol for handling of infection outbreaks and manage such situations
- Other similar matters related to infection control
Suggested members
35/17 Chairperson – Someone from top management such as CEO, Vice president or director or Medical Superintendent.
35/17 Convener or Coordinator – Infection Control Officer or Medical Microbiologist or Infectious diseases specialist
35/17 Clinical members – One representative each from all clinical specialties and super-specialties, including Anesthesiology, Critical Care, Emergency Medicine, Laboratory services, Blood Bank, Nursing Services, and Allied health specialties
Non-clinical members – Person in charge for the administration of Operation theatre, ICU, IPD, OPD, Emergency department, CSSD, Laundry, Bio-medical waste, Maintenance, Medical Equipment, and General Management
Question 15. Write down the various sources and routes or modes of transmission of infection.
Answer:
Sources of Infection Endogenous:
- § Patients’ own flora may invade the patient’s tissue during some surgical operations or instrumental manipulations
- § Normal commensals of the skin, respiratory, GI, UG tract
Sources of Infection Exogenous:
- § From another patient or staff member or environment in the hospital
- § Environmental sources: Inanimate objects, air, water, food
- § Cross infection from other patients, hospital staff (suffering from infections or asymptomatic carriers)
Modes of Transmission Of Infection:
1. Contact: Most common route of transmission
- Hands of staff: important vehicle of spread. Contact of hands and clothing of attendants
- Hands of staff Example: Staphylococcus aureus, Streptococcus pyrogens
- Inanimate objects: Improper disinfection of Instruments: endoscope, bronchoscope, cystoscope
- Inanimate objects Example: Pseudomonas aeruginosa
2. Airborne:
Droplets: Droplets of Respiratory infections: transmitted by inhalation
Dust: Dust from bedding, floors, wound exudates, and skin. Example: Pseudomonas aeruginosa, Staphylococcus aureus
Aerosols: Aerosols from nebulizers, humidifiers, and AC. Example: Legionella pneumophila
3. Oral Route: Hospital food may contain Antibiotic-resistant bacteria → may colonize the intestine → can cause infections
4. Parenteral route:
- Disposable syringes and needles
- Certain infections may be transmitted by blood transfusion, tissue donation, or contaminated blood products. Example: Hepatitis B, HIV
Question 16. Explain in detail the portals of entry and exit of microorganisms.
Answer:
Portals Of Entry (Entry Of Microbes Into Body): To cause any infection, pathogens must enter the body through certain pathways or routes called portals of entry which differ for various organisms.
Most of the pathogens can cause infection only if they enter through a particular route. The portals of entry may be:
- Alimentary tract: This tract serves as a portal of entry of the pathogenes causing typhoid, dysentery, and cholera. These pathogens are taken to the alimentary tract via ingestion of contaminated milk, food, or water through the mouth.
- Respiratory tract: This tract is a portal of entry of pathogens causing diphtheria, TB, pneumonia, etc. These pathogens have a special affinity for the respiratory tract and enter via
inhalation or through the mucous membrane of the mouth, nose to throat, tonsils, and lungs. - Urogenital tract: Some pathogens enter the body by coming in contact with the urogenital tract and are an important cause of STDs. example: pathogens causing AIDS, gonorrhea, syphilis.
- Inoculation: Some pathogens enter the body through the skin or mucous membrane through abrasions, wounds, or burns and cause severe wound infection. Example: spores of Cl.tetani enter the wound causing tetanus, Hep. B transmitted by transfusion of contaminated blood or inoculation of infected blood products.
Portals Of Exit (Exit Of Microbes From Body): The pathogens exit from the body of an infected person or carrier through certain routes or pathways called portals of exit.
The portals exist differ for different microorganisms depending upon the site or location of infection. The portal of exit may be:
- Feces
- Urine
- Sputum/saliva
- Skin and mucous membrane (secretion)
- Nose and throat secretions
- Eye secretions
- Blood
Question 17. What is asepsis? Write a detailed note on aseptic techniques.
Answer:
Asepsis Definition: Asepsis is the state of being free from disease-causing contaminants such as bacteria, viruses, fungi, and parasites or, preventing contact with microorganisms. There are two types of asepsis.
Medical asepsis, also known as the “clean technique” is aimed at controlling the number of microorganisms and is used for all clinical patient care activities. Surgical asepsis, also known as the “sterile technique” is aimed at removing all microorganisms and is used for all surgical/sterile procedures.
1. Medical asepsis: Medical asepsis is the state of being free from disease-causing microorganisms. Medical asepsis is concerned with eliminating the spread of microorganisms through facility practices. So cleaning up spills, and dirty surfaces and using disinfectant would be examples of this. Medical asepsis also includes the use of PPE (personal protective equipment), like gloves, gowns, and even masks, eye and face shields.
2. Surgical asepsis: Surgical asepsis is the absence of all microorganisms within any type of invasive procedure. The sterile technique is a set of specific practices and procedures performed to make equipment and areas free from all microorganisms and to maintain that sterility. The goal of asepsis is to prevent the contamination of the open surgical wound by isolating the operative site from the surrounding nonsterile environment.
Aseptic technique means using practices and procedures to prevent contamination from pathogens. It involves applying the strictest rules to minimize the risk of infection. Healthcare workers use the aseptic techniques in surgery rooms, clinics, outpatient care centers, and other health care settings.
Following aseptic technique helps prevent the spread of pathogens that cause infection.
- Healthcare professionals commonly use aseptic technique when they’re:
- Handling surgery equipment
- Helping with a baby’s birth by vaginal delivery
- Handling dialysis catheters
- Performing dialysis
- Inserting a chest tube
- Inserting a urinary catheter
- Inserting central intravenous (4) or arterial lines
- Inserting other draining devices
- Performing various surgical techniques
Aseptic technique benefits: Whenever your skin is opened, you’re vulnerable to infection. That’s why it’s critical for you to get prompt treatment for burns and wounds.
- Even intentional cuts during surgery put you at risk for infection. The way healthcare providers use aseptic techniques before, during, and after your procedure helps protect you from infection.
- When you need surgery or other procedures that require an aseptic technique, you’re already vulnerable to infections. You need your immune system to be at its strongest to heal. You have a better chance of recovery if you don’t have to fight off an infection.
Question 18. Write a note on biomedical waste and its management.
Answer:
Biomedical waste or hospital waste is any kind of waste containing infectious (or potentially infectious) materials. Waste sharps include potentially contaminated used (and unused discarded) needles, scalpels, lancets, and other devices capable of penetrating skin.
It may also include waste associated with the generation of biomedical waste that visually appears to be of medical or laboratory origin (for example, packaging, unused bandages, infusion kits, etc.), as well as research laboratory waste containing biomolecules or organisms that are mainly restricted from environmental release.
Biomedical waste is generated from biological and medical sources and activities, such as the diagnosis, prevention, or treatment of diseases. Common generators (or producers) of biomedical waste include hospitals, health clinics, nursing homes, emergency medical services, medical research laboratories, offices of physicians, dentists, veterinarians, home health care, and morgues or funeral homes. In healthcare facilities (i.e. hospitals, clinics, doctor’s offices, veterinary hospitals, and clinical laboratories), waste with these characteristics may alternatively be called medical or clinical waste.
Biomedical waste Management: Biomedical waste must be properly managed and disposed of to protect the environment, general public, and workers, especially healthcare and sanitation workers who are at risk of exposure to biomedical waste as an occupational hazard. Steps in the management of biomedical waste include generation, accumulation, handling, storage, treatment, transport, and disposal.
Accumulation, handling, and storage: Biomedical waste is generated from various sources. it is accumulated on those areas. So source identification is done on that site called segregation of the area. handling all waste carefully. And store for few hours till the transport vehicle comes to collect it.Store in a safe area.
Treatment, Disposal: The goals of biomedical waste treatment are to reduce or eliminate the waste’s hazards, and usually to make the waste unrecognizable. Treatment should render the waste safe for subsequent handling and disposal. There are several treatment methods that can accomplish these goals.
- It includes segregating the bio waste Biomedical waste is often incinerated. An efficient incinerator will destroy pathogens and sharps.
- Source materials are not recognizable in the resulting ash. Alternative thermal treatment can also include technologies such as gasification[8] and pyrolysis including energy recovery with similar waste volume reductions and pathogen destruction.
- An autoclave may also be used to treat biomedical waste. An autoclave uses steam and pressure to sterilize the waste or reduce its microbiological load to a level at which it may be safely disposed of.
- Many healthcare facilities routinely use an autoclave to sterilize medical supplies. If the same autoclave is used to sterilize supplies and treat biomedical waste, administrative controls must be used to prevent the waste operations from contaminating the supplies.
- Effective administrative controls include operator training, strict procedures, and separate times and space for processing biomedical waste. Microwave disinfection can also be employed for treatment of Biomedical wastes. Or By Volume reduction processess.
Question 19. Sources of infection
Answer:
Infection and immunity involve interaction between the animal body (host) and the infecting microorganisms. The lodgement and multiplication of a parasite in or on the tissues of a host constitute infection. It does not invariably result in disease.
Sources Of Infection
- Human beings
- Animals
- Insects
- Soil and water
- Food.
1. Human Beings: The most common source of infection for human beings is human beings themselves. The parasite may originate from a patient or carrier.
Humans serving as the microbial reservoir:
- Acquisition of “strep” throat through touching
- Hepatitis by blood transfusions
- Gonorrhea, syphilis, and AIDS by sexual contact
- Tuberculosis by coughing; and the common cold through sneezing.
2. Animals: Reservoir hosts: Many pathogens are capable of causing infections in both human beings and animals. Therefore, animals may act as a source of infection of such organisms. These animals serve to maintain the parasite in nature and act as reservoir and they are, therefore, called reservoir hosts.
Zoonosis: The diseases and infections, which are transmissible to man from animals are called zoonosis.
Examples of zoonotic diseases
Bacterial: Anthrax, brucellosis, Question fever, leptospirosis, bovine tuberculosis, bubonic plague, Salmonella food poisoning.
Viral: Rabies, yellow fever, cowpox, monkeypox.
Protozoal: Leishmaniasis, toxoplasmosis, trypanosomiasis, babesiosis.
Helminthic: Echinococcosis, taeniasis, trichinellosis.
Fungal: Microsporum canis, Trichophyton verrucosum.
3. Insect – Arthropod-Borne Diseases: Blood-sucking insects, such as mosquitos, ticks, mites, ies, and lice may transmit pathogens to human beings, and diseases so caused are called arthropod-borne diseases.
Insect – Arthropod-Borne Diseases Vectors: Insects that transmit infections are called vectors. Vector-borne transmission can be of two types either mechanical (external) or biological (internal).
- Mechanical vector: The disease agent is transmitted mechanically by the arthropod.
- Mechanical vector Examples: Transmission of diarrhea, dysentery, typhoid, food poisoning, and tracghoma by the house.
- Biological vectors: Biological vectors are those in whom the pathogens multiply succinctly or has undergone a developmental cycle. The interval between the time of entry of the pathogen into the vector and the vector becoming infective is called the extrinsic incubation period.
- Biological vectors Examples: Aedes aegypti mosquito in yellow fever, Anopheles mosquito in malaria.
- Reservoir hosts: Besides acting as vectors, some insects may also act as reservoir hosts (for example, ticks in relapsing fever and spotted fever). Infection is maintained in such insects by transovarial or transstadial passage.
4. Soil And Water
Soil: Some pathogens can survive in the soil for long periods.
Soil Examples
- Spores of tetanus and gas gangrene: Spores of tetanus and gas gangrene remain viable in the soil for several decades and serve as source of infection.
- Fungi and parasites: Fungi (causing mycetoma, sporotrichosis, histoplasmosis) and parasites such as roundworms and hookworms also survive in the soil and cause human infection.
Water: Water may act as the source of infection either due to contamination with pathogenic microorganisms (Shigella, Salmonella, Vibrio cholerae, poliomyelitis virus, hepatitis virus) or due the presence of aquatic vector (cyclops containing larvae of guinea worm infection).
5. Food: Contaminated food may act as source of infection of organisms causing food poisoning, gastroenteritits, diarrhea and dysentery.
Question 20. Classification of infection
Answer:
The lodgement and multiplication of a parasite in or on the tissues of a host constitute infection. It does not invariably result in disease.
Classification Of Infections: Infections may be classied in various ways
- Primary infection: Initial infection with a parasite in a host is termed primary infection.
- Reinfections: Subsequent infections by the same parasite in the host are termed reinfections.
- Secondary infection: When a new parasite sets up an infection in a host whose resistance is lowered by a preexisting infectious disease, this is termed secondary infection.
- Local infection: The term local infection (more appropriately local sepsis) indicates a condition where, due to infection or sepsis at localized sites such as appendix or tonsils, generalized effects are produced.
- Cross-infection: When in a patient already suffering from a disease, a new infection is set up from another host or another external source, it is termed cross-infection.
- Nosocomial infections: Cross-infections occurring in hospitals are called nosocomial infections (from Greek nosocomion hospital).
- Iatrogenic infection: The term iatrogenic infection refers to physician induced infections resulting from investigative, therapeutic or other procedures.
- In apparent infection: In apparent infection is one where clinical effects are not apparent.
- Subclinical infection: The term subclinical infection is often used as a synonym to in apparent infection.
- Atypical infection: Atypical infection is one in which the typical or characteristic clinical manifestations of the particular infectious disease are not present.
- Acute infection: An infection which lasts for a relatively short time. (few days to few weeks). Example: Measles.
- Chronic infection: An infection which lasts for a long time (over months and years). Example: TB.
- Autoinfection: An infection that occurs between two sites on the same host.(worms)
- Mixed infection: An infection caused by two or more organism.(bacterial vaginosis)
- Masked infection: An infection is known to occur but the infectious agent cannot be demonstrated.
- Oppurtunistic infection: An infection with organisms which are normally harmless but become pathogenic when the body’s defence mechanisms are compromised.
Question 21. Define carrier and its classification with examples.
Answer:
- Carrier: A carrier is person who harbours or lodge of the microorganisms without suffering from any ill effect’ because of it. There are several types of carriers
- Convalescent carrier: An individual who has recovered from the infectious disease but continues to harbour or lodge large numbers of pathogen.
- Healthy carrier: A healthy carrier is an individual who harbours or lodge the pathogen but is not ill.
- Incubatory carrier: An incubatory carrier is an individual who is incubating the pathogen in large numbers but is not yet ill.
- Temporary carriers: Convalescent, healthy, and incubatory carriers may harbour or lodge the pathogen for only a brief period (hours, days, or weeks) and lasts less than six months.
- Chronic carriers: They harbour the pathogen for long periods (months, years, or life).
- Contact carriers: The term contact carrier is applied to a person who acquires the pathogen from a patient.
- Paradoxical carrier: This refers to a carrier who acquires the pathogens from another carrier.

Leave a Reply