Swellings In The Suprasternal Space Of Burns
- Lipoma: Soft and lobular, edge slips under the palpating finger.
- Sequestration dermoid cyst is a midline, soft, cystic, fluctuant swelling.
- Gumma produces a firm swelling with evidence of syphilis elsewhere in the body.
- Thymic swellings and an aneurysm of the innominate or subclavian artery are the other causes.
Differential Diagnosis Of Lateral Swellings In The Neck
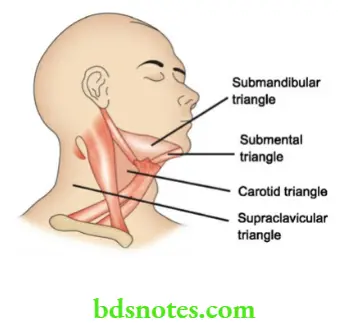
Before we discuss the swellings on the lateral side of the neck, it is essential to know the various triangles in the neck. These are discussed here.
Read And Learn More: Clinical Medicine And Surgery Notes
Triangles Of The Neck
Each side of the neck is a quadrilateral space subdivided by Sternocleidomastoid into anterior triangle and posterior triangle. They are further subdivided as follows:
Anterior triangle
- Submental triangle
- Digastric triangle
- Carotid triangle
- Muscular triangle.
Posterior triangle
- Occipital triangle
- Supraclavicular triangle.
Swellings In The Submandibular Triangle
- The submandibular triangle is a part of the anterior triangle
- This is bounded inferiorly by the anterior and posterior belly of digastric muscles with their tendon, and superiorly by the attachment of deep fascia to the mandible and to the whole length of hyoid bone.
- This triangle is covered by deep fascia.
- The floor is formed by mylohyoid muscle which arises from the mylohyoid line of the mandible, thus closing the space.
- Following are the swellings in the submandibular triangle:
-
- Enlarged submandibular lymph nodes—Common
- Submandibular salivary gland enlargement —Common
- Plunging ranula—Not uncommon
- Ludwig’s angina—Not uncommon
- Lateral sublingual dermoid cyst-Rare
- Tumours of the mandible — Rare.
Enlarged Submandibular Lymph Nodes
They form a nodular swelling which is deep to deep fascia. They are palpable only in the neck (not intraorally). The nodes can get enlarged due to the following conditions.
1. Acute lymphadenitis: Very often, poor oral hygiene or a caries tooth produces painful, tender, soft enlargement of these lymph nodes. Extraction of the tooth or with the improvement of oral hygiene, lymph nodes regress.

2. Chronic tuberculous lymphadenitis can affect these nodes along with upper deep cervical nodes. The nodes are firm and matted.
3. Secondaries in the submandibular lymph nodes arise from carcinoma of the cheek, tongue, palate. The nodes are hard with or without fixity.
4. Non-Hodgkin’s lymphoma can involve submandibular lymph nodes along with a horizontal group of nodes in the neck. The nodes are firm or rubbery in consistency.
Submandibular Salivary Gland Enlargement
Various causes of submandibular salivary gland enlargement have been discussed in the salivary gland chapter.
The common causes are chronic sialadenitis with or without a stone, tumours of the salivary gland or enlargement due to autoimmune diseases. They form irregular or nodular swelling. The diagnosis is confirmed by digital palpation of the gland.
The enlarged submandibular gland is digitally palpable because the deep lobe is deep to the mylohyoid muscle.
Differential Diagnosis Of Swellings In The Carotid Triangle
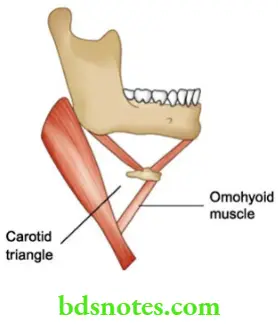
The carotid triangle has the following boundaries.
Laterally by sternomastoid muscle, superomedially by digastric muscle and stylohyoid muscle and anteromedially by omohyoid muscle.
Submandibular Salivary Gland Enlargement
- Calculus
- Chronic sialadenitis
- Cancer
- Chronic diseases—Autoimmune
A few important swellings in this triangle are as follows:
- Branchial cyst
- Lymph node swelling (cold abscess)
- Aneurysm of the carotid artery
- Enlargement of the thyroid gland
- Carotid body tumour — Rare
- Laryngocoele — Rare
- Sternomastoid tumour — Rare
- Neurofibroma vagus.
Branchial Cyst Aetiology
- The branchial cyst arises from vestigial remnants of the 2nd branchial arch.
- The cyst is lined by squamous epithelium and contains desquamated epithelial cells which slowly form a toothpaste-like material.
Branchial Cyst Clinical Features
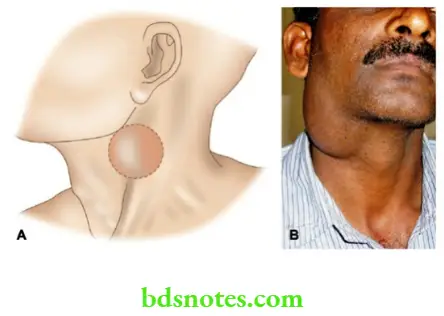
- Even though congenital, the majority of patients are young between the age group 15–25 years.
- The swelling is typically located in the anterior triangle of the neck partly under cover of the upper 1/3 of the anterior border of the sternomastoid. This can be explained because of the development of sternomastoid muscle from the myotome in the ridge of the second branchial arch.
- The swelling has a smooth surface and round borders. It is soft, cystic, fluctuant and transillumination-negative1. Otherwise, the consistency is that of a water-filled rubber bag. The swelling is very often firm due to thick inspissated content. In such situations, it is very difficult to elicit fluctuation. Mobility of the swelling is also restricted because of its adherence to the sternomastoid muscle.
- Sternomastoid contraction test: The swelling becomes less prominent.
- If contents are aspirated, it contains cholesterol crystals.
- No other lesion is found in the neck (lymph nodes).
Swellings Containing Cholesterol Crystals
- Branchial cyst
- Dental cyst
- Dentigerous cyst
- Hydrocoele
1Branchial cyst and thyroglossal cyst rarely give rise to transillumination if the contents are clear.
Branchial Cyst Treatment
Excision of the cyst with entire epithelial lining with a curved incision centred over the swelling. One must ensure that the epithelial lining should be removed completely or else recurrence will occur.
Branchial Cyst Complications
Since the wall is rich in lymphatic tissue, it can undergo secondary infection with pain and swelling. Hence, the swelling has to be excised.
Differential diagnosis
There is no differential diagnosis in a classical case of the branchial cyst. However, a few swellings have to be considered as differential diagnosis.
- A cold abscess occurs in young patients due to tuberculosis of the jugulodigastric nodes. The presence of multiple lymph nodes in the neck with or without fever gives a clue to the diagnosis.
- Lymphangioma is a brilliantly transilluminant partially compressible swelling. However, the anterior triangle is not a common site for lymphangioma.
- Lipoma can also occur in the neck, though it is an uncommon site.
Branchial Fistula
- This is always congenital and occurs due to persistent 2nd branchial cleft.
- The external opening is situated at the junction of the middle ⅓ and lower ⅓ of the sternomastoid.
- The tract from the skin passes through the fork of the common carotid artery deep to the accessory and hypoglossal nerves and opens in the anterior aspect of the posterior pillars of the tonsils. The tract is lined by squamous epithelium and discharges serous or mucous fluid. Sometimes the upper end is obliterated, resulting in a branchial sinus.
The patient may complain of a dimple, discharging mucus and the dimple becomes more obvious when the patient is asked to swallow. - Usually seen in growing adults
- Can be unilateral or bilateral, equally common in males and females
- It is also called as lateral fistula of the neck. (The thyroglossal fistula is called the median fistula of the neck.)
Branchial Cyst Treatment
A fistulogram can be done by injecting methylene blue into the external opening and the tract is defined. This is followed by an exploration of the tract. At surgery, it should be carefully dissected up to the internal opening and then excised.


Complication
Recurrent infection of the fistula.
Cold Abscess Due To Tuberculosis
- In India, this is the most common cystic swelling in the carotid triangle. The cold abscess results in caseation necrosis of the lymph nodes. This forms a soft, cystic, fluctuant swelling with negative transillumination. The presence of other lymph nodes in the neck, and sinuses in the neck gives the clue to the diagnosis.
- Loss of appetite, weakness and fever may be the other features.
Aneurysm Of The Common Carotid Artery
- Atherosclerosis is the most common cause of aneurysm. This weakens the vessel walls uniformly and produces fusiform dilatation of the blood vessel. Hypertension is another factor which adds to the aneurysm.
- The abdominal aorta is the most common of aneurysms followed by the popliteal artery.
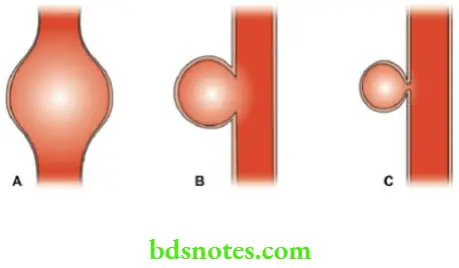
Branchial Cyst Types
- Fusiform: Atherosclerosis, hypertension.
- Saccular: Due to injury.
- False: In this condition there is a sac lined by cellular tissue which communicates with the artery through an opening in its wall.
Causes Clinical Features of Aneurysm
- Elderly patients are commonly affected.
- Evidence of atherosclerosis in the form of a thick-walled vessel is present.
- Tensely cystic (feels firm), fluctuant, transillumination negative swelling with expansile pulsation. (When the fingers are kept over the aneurysm they are not only elevated but they are separated.)
- Compressibility is positive
- On exerting pressure proximally the swelling diminishes in size — classically it happens in a case of popliteal aneurysm on compression of the femoral artery.
- Bruit/thrill is characteristic of this condition.
Aneurysm — Causes
- Congenital: Berry aneurysm in the circle of Willis
- Traumatic
- Degenerative: Atherosclerosis
- Rare causes:
- Syphilis—Endarteritis obliterans
- Mycotic—Infective emboli
- Subacute bacterial endocarditis
- Marfan syndrome
- Polyarteritis
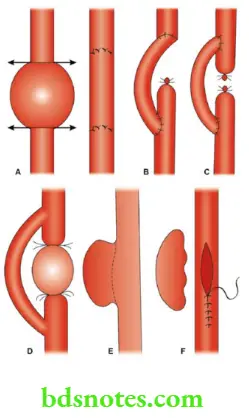
Branchial Cyst Treatment Of Aneurysm
Angiography to confirm the diagnosis followed by repair of aneurysm with PTFE graft (polytetrafluoroethylene graft.
Carotid Body Tumour (Chemodectoma)
- This is a benign tumour arising from chemoreceptors in the carotid body. They are situated in the tunica adventitia at the bifurcation of the common carotid artery.
- Hence, such a tumour is called chemodectoma.
- The function of the carotid body is the regulation of pH.
Branchial Cyst Clinical Features
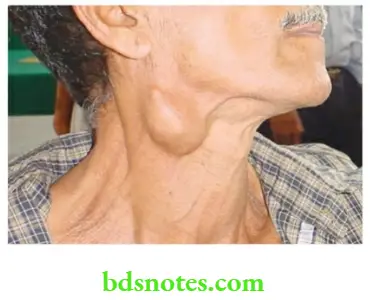
- Middle-aged or elderly patients are affected.
- The patient gives a history of painless slow-growing swelling for many years.
- Typical location: At the level of the hyoid bone, in the upper part of the anterior triangle of the neck beneath the anterior edge of the sternomastoid muscle.
- The surface is smooth or lobulated, borders are round, and there is an oval, vertically placed swelling. Consistency is firm to hard. Hence, called a classical potato tumour.
- Horner’s syndrome, unilateral vocal cord paralysis can occur due to involvement of the nerves.
- Pressure on the tumour gives rise to syncopal attack due to a decrease in the pulse rate (Carotid body syndrome).
- Moves in the transverse direction.
- The carotid artery is stretched over the swelling and so, transmitted pulsations are felt.
- Intra-oral examination shows prolapse of the ipsilateral tonsil.
Chemoreceptors: Sites
- The carotid body
- The aortic body
- Brainstem
- Pulmonary receptors
- Myocardial receptors

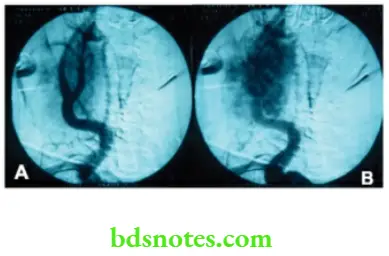
Diagnosis
Carotid angiography should be done if there are neurological symptoms such as syncopal attacks. It may demonstrate the separation of the carotid bifurcation.
Carotid Body Tumour
- A very, very rare tumour
- Rarely malignant
- Rarely bilateral
- Rarely grows fast
- Rarely do patients come early
- Rarely metastasizes
- Experience of a surgeon with this tumour is very, very rare — Rarest Of Rare
Tumours
Splaying of the carotid artery can be seen — Lyre sign.
Incision biopsy is dangerous.
Diagnosis Treatment
Excision of the tumour with reconstruction
Complication
Very rarely, it can turn into a malignant carotid body tumour with lymph nodal metastasis.
Sternomastoid Tumour
- This is not a tumour, it is a misnomer.
- Injury to the sternomastoid during birth caused the rupture of a few fibres and haematoma. Later, healing occurs with fibrosis, resulting in a swelling in the middle of the sternomastoid muscle.
- The other possible theory is that this is a congenital anomaly — short sternomastoid muscle.
Diagnosis Clinical Features
- This is seen in infants or children. Firm to hard, 1–2 cm swelling in the middle of the sternomastoid muscle.
- Tender, mobile sideways, medial and lateral borders are distinct but superior and inferior borders are continuous with the muscle.
- Many cases are associated with torticollis.
Diagnosis Treatment
- Gentle manipulation of the child’s head.
- Physiotherapy to stretch the shortened sternomastoid muscle.
- Division of lower attachment of sternomastoid from clavicle and sternum with or without removal of lump is the surgical treatment.
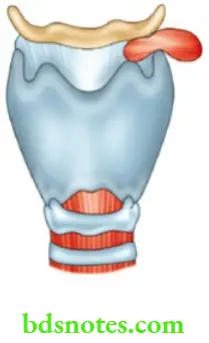
LAryngocoele
- It results in herniation of the laryngeal mucosa.
- When it enlarges within the larynx, it may displace the vocal cord, produces hoarseness and is called internal laryngoscope.
LAryngocoele Causes
- Glass blowers, musicians, wind instruments and trumpet players are commonly affected.
- Chronic cough may be one of the predisposing factors.
LAryngocoele Clinical Features
- Smooth, oval, boggy swelling which moves upwards on swallowing.
- Swelling becomes prominent when the patient is asked to cough or blow.
- Expansile cough impulse is present.
- Tympanitic note on percussion (resonant).
LAryngocoele Treatment
Excision of the sac.
Differential Diagnosis
Other cystic swellings such as branchial cysts and lymphangioma should be ruled out.
Complications
Secondary infection results in laryngopyocoele. The opening in the thyrohyoid membrane may be blocked by mucopus in such cases.

Leave a Reply