Question. 1. Define bone and alveolar bone. Describe the structure of the alveolar bone.
Answer:
Bone:
- It is a living tissue, which makes up the body’s skeleton and is one of the hardest structures of the animal body.
Alveolar bone:
- It is defined as that part of the maxilla and the mandible that forms and supports the sockets of the teeth.
Read And Learn More: BDS Previous Examination Questions and Answers
Structure of alveolar bone:
- The alveolar bone contains two parts.
- Alveolar bone proper.
- Supporting alveolar bone.
1. Alveolar bone proper:
- It is 0.1 – 0.4 mm thick
Functions:
- Surrounds the root of the teeth
- Gives attachment to principal fibers of PDL.
Parts:
Lamellated bone:
- It contains osteon which contains blood, Bessel.
Arrangement:
- Some of them are arranged parallel to the surface of the marrow space.
- While others from the Harversian system.
Read And Learn More: BDS Previous Examination Questions and Answers
Bundle bone:
- The bone directly lining the socket is called a bundle or bone.
- Principal fibers of PDL are embedded within it and constitute Sharpey’s fibers.
- They contain fewer fibrils, so they appear dark.
- Fibers are mineralized at the periphery.
- Bundle bone is formed in areas of recent bone apposition.
- It contains more calcium salt per unit area.
- Lines of rest are seen in bundle bone.
- Radiographically, it is referred to as lamina dura.
- It is opposed to an outer layer of lamellar bone.
Cribiform plate:
- Alveolar bone properly forming the inner wall of the socket is perforated by many foramina to transmit nerves and vessels, called cribriform plate.
Interdental petunia:
- It is a bone between the teeth composed entirely of cribriform plate.
- It contains the perforating nutrient canals – Zuckerkandl and Hirschfeld.
2. Supporting alveolar bone:
- The bone that surrounds the alveolar bone properlysupportsrt to the socket is called supporting alveolar bone.
It consists of
Cortical plates:
- It forms the outer and inner plates of the alveolar processes.
- It consists of surface layers of fine-fibered lamellar bone supported by compact Harversian system bone.
- It is thinner in the maxilla and thickest on the buccal aspect of mandibular premolars and molars.
- They are continuous with compact layers of the maxilla and mandible body.
- In the maxilla, the outer cortical plate is perforated by small openings for blood and lymphatics, while in the mandible it is dense.
Spongy bone:
- It is bone occupying the central part of the alveolar process.
- It fills the area between the cortical plates and the alveolar bone properly.
- It consists of bone disposed of in lamellae with Harversian systems occurring in the large trabeculae.
- They are surrounded by marrow, rich in adipose cells and pluripotent mesenchymal cells.
Question 1. Write about age changes and clinical considerations of the mandible.
Answer:
Age changes:
1. In infants and children:
- Two halves of mandible – fuses during 1st year of life.
- Mental foramen – opens below the sockets for the two deciduous molar teeth.
- Mandibular canal – runs near the lower border.
- Angle-obtuse (140 degrees).
- Coronoid process – large and projects upwards.
2. In adults:
- Mental foramen – opens midway between the upper and lower borders.
- Mandibular canal – runs parallel to the mylohyoid line.
- Angle – 110 or 120 degrees.
- Ramus – almost vertical.
3. In old age:
- Alveolar border- absorbed as teeth fall out.
- Height of body of mandible – reduced
- Mental foramen – close to the alveolar border.
- Mandibular canal – close to the alveolar border
- Angle – obtuse (140 degrees)
- Ramus – oblique.
Clinical Considerations:
- Commonly fracture site is a canine socket as it is weak.
- The next common fracture of the mandible occurs at the angle and neck of the mandible.
- Bone is resorbed on the side of pressure and apposed on the side of tension.
- On the pressure side, there is an increase in the level of cAMP in cells.
- At sites of tension, osteoblasts are activated to produce osteoid which mineralizes to form bone.
- During the healing of fractures or extraction wounds, an embryonic type of bone is formed which is replaced by mature bone.
Question 2. Osteoblast and osteoclast.
Answer:
Osteoblast:
Origin:
- Pluripotent stem cells of mesenchymal origin.
- Morphology:Mononucleated cell
- Basophilic
- Cuboidal or slightly flattened.
- Abundant and well-developed organelles
- The cells contact one another by adherents and gap junctions.
- They contain prominent bundles of actin, myosin, and cytoskeleton proteins.
Functions:
- Formation of new bone.
- Regulation of bone remodeling and mineral metabolism.
- Mineralization of osteoid.
- Act as a barrier that controls ion flux into and out of bone.
- Control mineral homeostasis and ensure bone vitality.
- The primary site for mineral exchange between blood and bone.
- Secrete a variety of cytokines that regulate cell metabolism and members of BMP and growth factors.
- Recognize the resorptive signal and transmit it to the osteoclast.
- Regulation:It is controlled by hormones, proteins, and bone cells.
Osteoclast:
- Origin:Derived from hemopoietic cells of the monocyte-macrophage lineage.
- Morphology:Multinucleated, large cell.
- Size: 40-100 μm in diameter (approx.).
- Cytoplasm – shows acid phosphatase
- Organelles.
- Extensive mitochondrial, Golgi complex.
- Sparse rough endoplasmic reticulum.
- They occupy a hollow-out depression called Howship’s lacunae.
- Adjacent to the tissue surface, the osteoclast cell membrane shows deep folds called ruffled borders.
- At the periphery of this border, the plasma membrane is apposed closely to the bone surface and the adjacent cytoplasm is devoid of cell organelles.
Functions:
- Resorbs bone by removing the mineralized matrix of bone.
- Regulation:Estrogen – suppresses the production of bone-resorbing cytokines.
- Vitamin D3 – promotes the differentiation of osteoclasts.
- Parathyroid hormone – stimulates the maturation and action of osteoclasts.
- Calcitonin – a potent inhibitor of osteoclast activity.
- TNFα- stimulates differentiation of osteoclast progenitors into osteoclast.
Question 3. Describe the histology and functions of alveolar bone.
Answer:
Histology of alveolar bone:
- Bone has a dense outer sheet of compact bone and a central medullary cavity filled with red or yellow bone marrow that is interrupted by a network of bone trabeculae.
- Surrounding the outer surface of every compact bone is a connective tissue membrane, the periosteum which has two layers.
1. Outer layer:
- Consists of a dense, irregular connective tissue termed the fibrous layer.
2. Inner layer:
- Consist of bone cells, their precursors, and a rich blood supply.
- The internal surfaces of compact bone are covered by an essentially cellular membrane, the endosteum.
Bone cells:
1. Osteoblasts:
- Mononucleated cells with abundant organelles and prominent cytoskeleton.
- It is derived from pluripotent stem cells of mesenchymal origin.
- They secrete the organic matrix of bone called osteoid.
- They regulate bone remodeling and mineral metabolism.
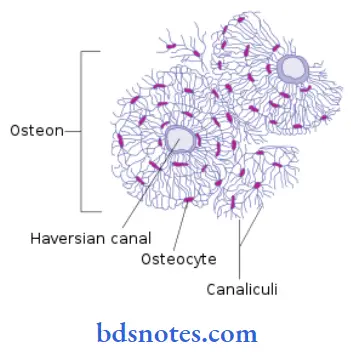
2. Osteocytes:
- As osteoid is formed, some of the osteoblasts become embedded in it and form osteocytes.
- After their formation, they reduce in size.
- They contact their adjacent osteocytes and osteoblast through canaliculi.
- They participate in the local degradation of bone.
3. Osteoclasts:
- Multinucleated, large cell, derived from monocyte.
- They resorb bone.
- They occupy hollow-out depressions called Howship’s lacunae.
Functions of alveolar bone:
- It supports the roots of teeth.
- It surrounds the root of the tooth and gives attachment to the principal fibers of PDL.
- It allows the movement of teeth for better occlusion.
- It helps to absorb and distribute occlusal forces.
- It supports lips and cheeks and enhances esthetics.
- Supplies nutrition to PDL through blood vessels passing through them.
- Organizes eruption of teeth.
- Supports the primary teeth and protects developing permanent teeth.
Question 4. Types of bone
Answer:

Question 5. Sharpey’s fibers
Answer:
- Sharpey’s fibers are contained in bundle bone
- Arranged parallel to the root
- Sternum
- Ribs
- Scapula
- Clavicle
- Vertebrae
- Facial bones
- Pelvic bones
- Bones of trunk and extremities
- Mandible
- Clavicle
- They are embedded into the cementum on one side and into the alveolar bone on another side
- Fibers in primary acellular cementum are fully mineralized while those in cellular cementum and bone are partly mineralized
- Their mineralized part appears as a projecting covered with mineral clusters
- Few of them pass uninterrupted through the alveolar bone to continue as principal fibers of PDL
- It passes through alveolar bone only when it consists entirely of compact bone
- It consists of noncollagenous proteins – osteopontin and bone sialoprotein
Question 6. Theories of calcification
Answer:
1. Nucleation theory
- Proposed by Neumann
- According to it, the nucleus is formed in relation to collagen which is effective in the aggregation of calcium and phosphate ions
- Due to this addition of hydroxyapatite crystals into saturated surrounding fluids, these crystals grow spontaneously
- Nucleation sites may be
- Ground substance
- Composed of sulfated glycosaminoglycans and proteoglycans
- Collagen
- Contains initial mineral deposits at discrete sites or on fibrils
- Mitochondria
- Has an indirect role in calcification as they are the earliest storage sites of calcium and phosphates in the form of amorphous calcium phosphate
2. Role of matrix vesicles
- Matrix vesicles are small membrane-bound structures lying free in matrix
- They are rich in phospholipids, especially phosphatidyl serine which has a high affinity to calcium ions
- Vesicles also contain annexin which forms calcium channels
Calcification:
- The extracellular matrix contains high levels of calcium and phosphate concentration
- Calcium channels present on matrix vesicles lead to the entry of calcium and phosphate into it
- When a certain thickness is reached, these hydroxyapatite crystals are released into the extracellular matrix
- These released crystals serve as templates for the formation of crystalline arrays
3. Role of alkaline phosphatase
- Alkaline phosphatase participates in the process of calcification
- This enzyme is present in matrix vesicles of chondrocytes, osteoblasts, and odontoblasts
- It hydrolyses organic phosphate-containing substrates and increases inorganic phosphate concentration
- This inorganic phosphate contributes to the formation of hydroxyapatite crystals
Question 7. Alveolar bone proper
Answer:
- It is 0.1-0.4mm thick
Functions:
- Surrounds the root of the teeth
- Gives attachment to principal fibers of PDL
Parts:
- 1. Lamellated bone:
- It contains osteon which contains blood vessel
- Some of them are arranged parallel to the surface of marrow space while others form a haversian system
2. Bundle bone:
- The bone directly lining the socket is referred to as bundle bone
- Principal fibers of PDL are embedded within it and constitute Sharpey’s fibers
- They contain fewer fibrils
- Fibers are mineralized at the periphery
- Formed in areas of recent bone apposition
Cribiform plate:
- Alveolar bone properly forming the inner wall of socket is perforated by many foramina to transmit nerves and vessels called the cribriform plate
Question 8. Regulation of serum calcium level
Answer:
Calcium level is regulated by
- Calcitriol
- It is the active form of vitamin D
Mechanism:
Induces synthesis of calcium-binding protein
↓
This increases calcium absorption by the intestine
↓
This increases calcium level
↓
It also promotes calcification &remodeling of bone
↓
Parathyroid hormones
↓
Secreted by Parathyroid glands
Mechanism:
Binds to a membrane receptor protein
↓
Activates adenylate cyclase
↓
Liberates cAMP
↓
Increases intracellular calcium
↓
Action on bone
Stimulates pyrophosphatase& collagenase
↓
Causes decalcification of bone
↓
Results in bone resorption
↓
Action on the kidney
↓
Stimulates 1-Hydroxylation of 25-hydroxycholecalciferol
↓
Promotes production of Calcitriol
↓
Action on intestine
↓
Promotes synthesis of Calcitriol
↓
Increases calcium absorption
Calcitonin
- Secreted by parafollicular cells of the thyroid gland
Mechanism:
Increases osteoblastic activity
↓
Promotes calcification
↓
Decreases bone resorption
↓
Increases calcium excretion
↓
This decreases blood calcium level
Question 9. Composition of bone
Answer:
1. Cells
- Osteoblast
- Cuboidal cell
- Contains
- Rough endoplasmic reticulum
- Large Golgi apparatus
- Secretory vesicles
Functions:
- Synthesizes osteoid and collagen
- Regulates mineralization
Precursor:
- Progenitor cells
- Osteoclasts
- Multinucleated giant cells
- Precursor- Blood-borne monocytes
Functions:
- Resorption of bone
- Secretes hydrolytic enzymes
- Osteocytes
- These extend processes from lacunae to canaliculi
Functions:
- Canaliculi bring oxygen and nutrients to osteocytes
2. Extracellular matrix
- Inorganic
- Calcium
- Hydroxyl
- Phosphate
- Carbonate
- Citrate
- Sodium
- Magnesium
- Fluorine
3. Organic
- Osteocalcin
- Osteonectin
- BMP
- Proteoglycans
- Glycoproteins
Question 10. Factors affecting calcium metabolism in the body
Answer:
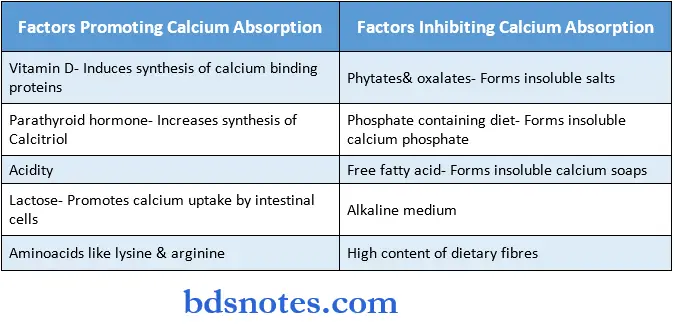
Question 1. Alveolar bone:
Answer:

Definition:
- Factors Inhibiting Calcium Absorption
- Phytates& oxalates- Forms insoluble salts
- Phosphate-containing diet- Forms insoluble calcium phosphate
- Free fatty acid- Forms insoluble calcium soaps Alkaline medium
- The high content of dietary fibers
- It is defined as that part of the maxilla and the mandible that forms and supports the socket of the teeth.
Structure:
- It contains two parts.
- Alveolar bone proper
- Supporting alveolar bone
- Lamellated bone
- Cortical plates
- Bundle bone
Question 2. Howship’s laucane.
Answer:
- Osteoclasts are found in a baylike depression called Howship’s lacunae.
- They are often shallow troughs with an irregular shape, reflecting the activity and the mobility of osteoclasts during active and the mobility of osteoclasts during active resorption.
- After the dissolution of the mineralized component, Howshiop’s lacunae are excavated into the bone.
- Following osteoclast-mediated resorption, the Howship’s lacunae remain covered with an undigested demineralized collagen matrix.
- On the mesial alveolar wall of a drifting tooth, Howhsip’s lacunae containing osteoclasts are present.
- This indicates active reporting on the mesial wall of the drifted tooth.
Question 4. Reversal line.
Answer:
- The scalloped outline of Howhsip’s locate that turns their convexity towards the old bone remains visible on a darkly stained cementing line called the reversal line.
- It is a thin layer of glycoproteins comprising at least bone sialoprotein and osteopontin.
- It acts as a cohesive, mineralized layer between the old bone and the new bone to be secreted.
- On its top, osteoblasts begin to lay down the new bone matrix, mineralizing it from the outside in.
- They appear during the reconstruction of the alveolar bone.
Question 5. Spongy bone.
Answer:
- It is bone occupying the central part of the alveolar process.
- It fills the area between the cortical plates and the alveolar bone proper.
- Radiographically, it is classified into 2 parts.
1. Type 1:
- The interdental and inter radicular trabeculae are regular and horizontal in a ladder-like arrangement.
- Most often seen in the mandible.
2. Type 2:
- Shows irregularly arranged, numerous, delicate interdental and inter radicular trabeculae.
- It is more common in the maxilla.
Question 7. Lamina dura.
Answer:
- Radiographically the alveolar bone proper is seen as a radiopaque white line.
- Periosteum
- Outer circumference lamella
- Osteocyle
- Concentric lamella
- Interstitial lamella
- Haversian canal
Question 12. Osteoblast
Answer:
- Cuboidal cell
- Contains
- Rough endoplasmic reticulum
- Large Golgi apparatus
- Secretory vesicles
Functions:
- Synthesizes osteoid and collagen
- Regulates mineralization
Precursor:
- Progenitor cells
Question 13. Calcium.
Answer:
Sources of calcium:
- Milk & milk products are regarded as the best sources of calcium
Other good sources of calcium are:
- Beans, leafy vegetables, fish, cabbage, egg yolk.
Functions of calcium:
- Development of bone & teeth
- Calcium is required for the formation of hydroxyapatite
- Bones serve as a reservoir of calcium
- Muscle contraction
- Calcium ions react with troponin C & trigger muscle contraction
- Activates ATPase
- Increases interaction between actin & myosin
- Blood coagulation
- Calcium is coagulation factor IV
- Nerve transmission
- It is involved in the transmission of nerve impulse
- Membrane integrity & permeability
- It influences the membrane structure
- Activation of enzymes
- It activates ATPase, lipase & succinate dehydrogenase
- Binds with calmodulin to activate certain enzymes
- It acts as a second messenger for certain hormonal actions
- Causes release of insulin, PTH, calcitonin
- Involved in endocytosis, exocytosis & cell motility
- Involved in cell contact & cell adhesion
- Acts on the myocardium & prolongs systole
Question 14. Normal serum calcium level
Answer:
Normal Serum Levels:
- Calcium-9-11 mg/dl

Leave a Reply