Diseases Of Blood
Question. Discuss in short Neutropenia.
Answer. The presence of abnormally small number of neutrophils in the blood usually less than 1500 to 2000 per micro liter.
Causes Of Neutropenia
- Starvation and *debility.
- Overwhelming infections and toxemia in older people.
- Infections: Typhoid, measles, malaria, kalaazar, hepatitis,inflenza, HIV and miliary TB.
- Hypersplenism, liver cirrhosis.
- Bone marrow failure: In aplastic anemia, leukemia and myelofiroma
- Drugs: Sulfonamides, antibiotic, analgesics, antithyroids,anticonvulsants, etc.
- Anaphylactic shock.
Read And Learn More: General Medicine Question And Answers
Clinical Manifestations Of Neutropenia
- Females are more commonly affcted as compared to males
- Early manifestations of agranulocytosis are may be in form of sore throat or pain.
- There may be fever going up to 130°F, sometimes coming with rigor chills, body ache and pain and extreme degree of prostration.
- In large number of cases ulceromembranous lesions appear on throat, tonsils, gum, tongue and genitalia
- These are often covered with grayish black exudates and may become gangrenous.
- Lymph gland generally cervical groups and in some, there are generalized lymphadenopathy
- Liver and spleen may become enlarged.
- As disease progresses severe toxemia develops and patient may go into shock.
Investigations Of Neutropenia
- Peripheral blood film show complete absence of neutrophils.
- Bone marrow is normocellular and show decrease mature neutrophils.
Management Of Neutropenia
- Firstly, the cause is removable which is identifible.
- Secondly, the infection is controlled and patient is put on isolation ward and barrier nursing is done.
- Antibacterial drugs such as penicillin 5 mega units IM or IV 4 hourly or ciproflxacin 500 mg IV 4 hourly is started immediately.
- In addition metrogyl 500 mg every 6 hourly to take care of infection
- Anabolic steroids are also given.
- In cases where toxemia is severe corticosteroids are employed, i.e. injection dexamethasone 4 mg IV 6 hourly.
- Granulocytes transfusion is given to tide over crisis. This is given daily for 5 to 7 days.
Question. Write short note on Bleeding Disorders in Dental Practice.
Or
Write short note on bleeding disorder.
Answer. Bleeding disorders: Bleeding disorders or hemorrhagic diatheses are a group of disorders characterized by defective hemostasis with abnormal bleeding.
Bleeding disorders
Idiopathic Thrombocytopenic Purpura
Idiopathic Thrombocytopenic Purpura Etiology
- Impaired platelet production
- Accelerated platelet destruction
- Splenic sequestration
- Dilution loss
Idiopathic Thrombocytopenic Purpura Oral Manifestations
- Excessive bleeding after tooth extraction.
- Extensive spontaneous gingival bleeding may be seen.
- Petechiae do not blench on pressure
Idiopathic Thrombocytopenic Purpura Management
- Corticosteroids that is prednisolone 60 mg/dL.
- Splenectomy, if there is no response to prednisolone to prednisolone in 3–4 days.
- Local hemostatics.
Hemophilia
Hemophilia Etiology
- It is a hereditary disorder.
- It occurs due to the defiiency to reduce activity of factor
- VIII in hemophilia A or factor IX in hemophilia B.
Hemophilia Oral Manifestations
- Prolonged bleeding after tooth extraction hematoma of flor of mouth and larynx with subsequent respiratory embarrassment.
- Physiological process of tooth eruption may be associated with severe and prolonged hemorrhage.
Hemophilia
Hemophilia Management
- It is done by fresh blood transfusion when bleeding is in the large mass.
- Factor VIII concentrate is employed in case of hemophilia A and factor IX concentrate is employed in case of hemophilia B.
- A hemophilic will require treatment before any dental procedure. Such patient is managed by IV infusion or cryoprecipitate or factor VIII combined with aminocaproic acid 4 to 6 g QDS.
- For any major surgery or periodontal surgeries or extraction of tooth hemophilic patient should be hospitalized.
Infusion of factor VIII concentrate is given before surgery and is continued for 48 to 72 hours. Antibiotic should also be given to the patient von Willebrand’s disease
Hemophilia Etiology
Hereditary coagulation disorder occurring due to qualitative or quantitative defects in von Willebrand factor.
Hemophilia Oral Manifestations
- Gingival bleeding and postextraction bleeding
- Disease may be discovered after dental extraction.
Hemophilia Management
- Mild episodes of bleeding can be treated with desmopressin which increases vWF level which leads to secondary increase in Factor VIII.
- For more serious bleeds during dental procedure hemostasis is achieved by Factor VIII concentrate which contain considerable quantities of vWF in addition to factor VIII.
Hereditary Hemorrhagic telangectasia
It is transmitted as autosomal dominanttraitand is characterized by bleeding from mucous membrane.
Hereditary Hemorrhagic telangectasia Management
- In patient having repeated attcks of epistaxis septal dermoplasty should be done. In septal dermoplasty,involved mucosa get removed and skin grafting is done.
- If spontaneous hemorrhages are present or nasal bleeding is present during dental procedure, it is controlled by giving pressure packs.
- Sclerosing agents, i.e. sodium tetradecyl sulphate if injected intra lesionally stop bleeding.
- Electrocautery is done. It helps in arresting bleeding.
Disseminated Intravascular Coagulation
It is a condition that results when the clottng system is activated in all or a major part of vascular system.
Despite widespread firin production the major clinical problem is bleeding not thrombosis.
Disseminated intravascular coagulation (DIC) is associated with a number of disorders such as infection, obstetric complications, cancer and snakebite.
Disseminated Intravascular Coagulation Management
- Correction of hemodynamic instability by flid therapy,transfusion of packed cells or whole blood.
- Factor replacement: This is the specifi therapy, in this freshfrozen plasma, cryoprecipitate, platelet concentrate transfusions are essential. Freshfrozen plasma is given at the dose of 15 mL/kg. Platelet is transfused at the dosage of 0.1 unit/kg.
Question. Write differential diagnosis of skin bleed.
Answer. Differential Diagnosis of skin Bleed
- Staphylococcal scalded skin syndrome
- Bacterial skin infection
- Viral skin disease: Measles, rubella
- Dermatitis
- Lichen planus
- Fungal skin infection
- Squamous cell carcinoma
- Urticaria
- Tick bite
- Spirochetal infection
- Hypersensitivity and inflmmatory diseases
- Hemoptysis
- Acne and related disorders
- Iron defiiency anemia
- Cancer of skin (Melanoma, Kaposi’s sarcoma)
- Rheumatoid arthritis
- Non-Hodgkin’s lymphoma
- Parasitic infection
- Vitamin C defiiency
- Benign tumor
- Acute leukemia
- Cellulitis
- Disseminated intravascular coagulation.
Question. Write short note on leukemia.
Answer. Leukemia is defied as clone of malignant cells derived from myeloid or lymphoid stem cells.
Etiology Of Leukemia:-
- Genetic factors such as familial, identical twins, congenital disorders.
- Environmental factors, i.e. atomic radiation and pollution Ionizing radiations
- Retroviruses
- Chemical agents, i.e. alkylating agents, cytotoxic drugs.
Types Of Leukemias
Acute Leukemia
- Acute lymphoblastic leukemia
- Acute myeloid leukemia
Chronic Leukemia
- Chronic lymphatic leukemia
- Chronic myeloid leukemia.
Clinical Features Of Leukemia:-
- Anemia
- Fatigue and lethargy
- Fever
- Bone and joint pain
- Combination of pallor, petechiae or purpura is present.
- Mucus membrane is bleeding
- Hepatomegaly, splenomegaly and renomegaly is present.
- There is tenderness over other bones.
Investigations Of Leukemia:-
- Bone marrow picture shows hypercellular reaction is present with premature and primitive cells.
- There is presence of biochemical changes with presence of
- Philadelphia chromosome.
- Peripheral blood fim show normocytic normochromic picture with an abundance of neutrophil, myelocyte,metamyelocyte.
White cell counts are elevated
Treatment Of Leukemia:-
- Chemotherapy, bone marrow transplantation or both should be done.
- New regimes are derived regularly and are tailored to specifi illness
- Treatment is given in several phases, with a period of induction chemotherapy to induce remission followed by maintenance and consolidation phases.
- This multiphase treatment is designed for further deplete malignant cells from bone marrow to achieve complete cure.
Question. Briefl describe Acute Leukemia.
Or
Describe the etiology, clinical features and management of acute leukemia.
Answer. Acute leukemia is defied as an uncontrolled growth of immature hemopoietic cells at the exposure normal marrow tissue.
Etiology Of Acute Leukemia
- Radiation: Association between radiationinduced genetic damage to the hemopoietic progenitors and development of myelodysplasia and acute leukemia is seen after nuclear disease.
- Chemical and drugs: Chronic benzene exposure and use of cytotoxic and immunosuppressive agents.
- Oncogens and cytogenic abnormalities
- Genetic factors, i.e. genetic disorders such as Down’s syndrome, Klinefelter’s syndrome, etc.
- Viruses: Infection by human lymphotrophic virus (HTLV1).
Clinical Features Of Acute Leukemia
- Symptoms due to anemia, i.e. tiredness, weakness and marked pallor.
- Hemorrhagic manifestation: Petechiae, bleeding from gums and nose, persistent bleeding after tooth extraction.
- Infection: It causes infective lesions of mouth and throat, i.e.
ulceration of mouth and pharynx, herpes simplex infection of face and infection of respiratory tract such as bronchitis and pneumonia. - Symptoms of cellular hyperviscosity
- There are tissue deposits of leukemic cells causing gum hypertrophy which is common in myelomonocytic and monocytic variety of AML.
- Lymphadenopathy and splenomegaly are common in acute lymphoid leukemia.
- Signs of organ infitration are present, i.e.
- CNS: Meningeal involvement occurs in children with acute lymphocytic leukemia.
- Skin: Bluish nodules or dusky red patches are present.
- Kidneys: Presence of kidney failure.
- Other sites: Testes, ovary, liver, gut and serous membranes such as pleura and peritoneum.
- Bone pain are present i.e. tenderness of sternum, osteolytic bone lesions and pathologic fractures may occur.
- Constitutional symptoms, i.e. fever, malaise and prostration.
- Roth’s spot, i.e. presence of white central retinal hemorrhages in acute myeloid leukemia
Management Of Acute Leukemia
Chemotherapy Of Acute Leukemia
- Induction phase: Initial high dose chemotherapy in order to reduce leukemic cells below the levels of morphogenic detection
Treatment Regimen for Acute Lymphoblastic Leukemia
- Vincristine 1.4 mg/m2 IV weekly for 4 weeks.
- Prednisolone 60 mg/day for 4 weeks.
- L- Asparaginase 50–200 ku/kg IV for 4 weeks.
- Daunorubicin 30 mg/m2 IV daily for two weeks.
Treatment Regimen for Acute Myeloid Leukemia
- Daunorubicin IV alternate days 3 doses.
- Cytosine arabinoside IV BD for 10 days
- Thioguanine oral BD for 10 days.
- In this, blood transfusion and platelet transfusion are required.
- CNS prophylaxis: Intra thecal methotrexate is given in acute lymphoblastic leukemia
- Consolidation: Another dose of chemotherapy to reduce leukemic burden
In Acute Lymphoblastic Leukemia
- IV daunorubicin
- IV cytosine arabinoside
- IV Etoposide
- Methotrexate, 6 thioguinine
- Dexamethasone
In Acute Myloid Leukemia
- High dose IV Cytosine arabinoside is given
- Maintenance: Low dose chemotherapy for 18 months to 2 years
In Acute Lymphoblastic Leukemia
- Oral Prednisolone
- IV Vincristine
- Oral 6 mercaptopurine
- Oral Methotrexate
In Acute Myeloid Leukemia
Post remission therapy is given, i.e. myeloablative therapy followed by bone marrow transplantation in relapse or those with highrisk chromosomal changes.
Bone marrow transplantation Of Acute Leukemia
In Acute Lymphoblastic Leukemia
Allogenic bone marrow transplantation is an option in acute lymphocytic leukemia patients entering first remission who have an HLA identical sibling, provided the sibling is fi and is less than 55 years.
In Acute Myeloid Leukemia
In adult patienthigh dose chemotherapy with autologus transplantation of hemopoietic stem cells derived from peripheral blood or bone marrow can be done.
Supportive Care Of Acute Leukemia
- Hemoglobin level should not allow falling below
8 g/dL by transfusing 4 units of packed RBCs. This is done to avoid anemia. - If bleeding is present, then there is transfusion of pooled or single donor platelets.
- Good nursing, prophylactic gastrointestinal tract decontamination, antibiotics and attntion to flid balance are given to prevent infections.
- If disseminated intravascular coagulation is present, then firinogen replacement, platelet transfusion twice daily and anticoagulants are given.
- Pneumocystis jiroveci pneumonia is a risk during the treatment of acute lymphocytic leukemia maintenance therapy.
- Hyperuricemia is prevented by adequate hydration and pretreatment with allopurinol which should be continued till peripheral blood is cleared of blast cells.
Hereditary Blood Disorders
Question. Write short note on chronic myeloid leukemia.
Answer. Chronic myeloid leukemia is a clonal disorder of pluripotent stem cell.
The most important characteristic feature of chronic myeloid leukemia is demonstration of Philadelphia chromosome in leukemic blast cells.
Clinical Features Of Chronic Myeloid Leukemia:-
Common Features Of Chronic Myeloid Leukemia:-
- Nonspecific: Loss of weight, fatigue, malaise, excessive perspiration.
- Splenomegaly: Size of spleen is enlarged
- Bleeding, excessive menstrual or other bleeding.
- Anemia
- Bone pain: It is due to extension of hemopoiesis through long bones.
Rare Features Of Chronic Myeloid Leukemia:-
- Splenic infarction
- Leukostasis
- Gout
- Retinal hemorrhage
- Fever.
Etiology Of Chronic Myeloid Leukemia:-
Chronic myeloid leukemia results from translocation of genetic material between chromosome 9 and 22.
The translocation result in production of abnormal tyrosine kinase that makes affcted cell immortal.
Investigations Of Chronic Myeloid Leukemia:-
- Peripheral blood: WBC count is 10–500 × 10 9/L, with excess of neutrophils, myelocytes and blasts. Basophilia and eosinophilia are prominent and thrombocytosis is common.
- Bone marrow is hypercellular with marrow firosis and gaucher like cells. High myeloid to erythroid ratio, i.e. 15 to 20 : 1.
- Neutrophil alkaline phosphatase is low.
- Serum vitamin B12 is increased.
- Serum uric acid is increased.
Hereditary Blood Disorders
Treatment Of Chronic Myeloid Leukemia:-
Chronic Phase Of Chronic Myeloid Leukemia:-
- Tyrosine kinase inhibitor therapy with Imatinib 400 mg OD as fist line.
- Othersecond generation: Tyrosine kinase inhibitor advocated in fist line therapy.
- Ponatinib used in case of resistant to fist and second generation Tyrosine kinase inhibitor.
- Zinatinib is now used in cases of very high counts.
- Allogenic stem cell transplant with HLAatchedrelated or unrelated donor, in case of Tyrosine kinase inhibitor intolerance
- Omacetaxine can also be given.
- Alphainterferon therapy can be given to maintain remission in chronic phase of disease in patient less than 70 years of age. It is given either intramuscularly or subcutaneously in dose of 3 to 9 mega units daily, then dose is reduced and majority of patients tolerate the dose of 3 mega units/3 times a week without any side effct.
Advanced Phase Disease Of Chronic Myeloid Leukemia:-
- Treatment oflymphoid blast crisis is done: Treatment similar to Acute lymphoblastic leukemia is done.
- Myeloid crisis: Prognosis is poor and few of drugs used in treatment of AML offr more than temporary relief.
Question. Write short note on oral manifestation of leukemia.
Answer. Oral Manifestations of Leukemia Oral Manifestations of acute leukemia
- Bleeding from gingiva is present. Gingiva becomes boggy,edematous and red in color.
- Presence of paresthesia of lower lip.
- Crustation over lips is seen.
- Mobility of permanent teeth is present.
- Oral mucosa appears pale with ulceration along with petechiae and ecchymosis.
Oral Manifestations Of Chronic Leukemia
- Gingival hypertrophy is present. Ulceration of gingiva with necrosis is present.
- Tongue is dark and is swollen.
- Presence of mobility of teeth is seen.
- Necrosis of PDL is seen
- Alveolar bone destruction is also present.
Question. Write short note on splenomegaly.
Or
Write short answer on splenomegaly.
Answer. Splenomegaly is defined as the enlargement of the spleen. Spleen can be mildly, moderately and massively enlarged.
Classifiation of Splenomegaly as Per its Size:-
- Mild splenomegaly: In it spleen is mildly enlarged and weighs up to 500 gm.
- Moderate splenomegaly: In it the spleen is moderately enlarged weighs up to 500 to 1000 gm.
- Massive splenomegaly: In it the spleen is massively enlarged and weighs up to greater than 1000 gm.
Causes Of Splenomegaly:-
Infections Of Splenomegaly:-
- Bacterial: Septicemia, typhoid, infective endocarditis, TB,syphilis.
- Viral: Hepatitis, infectious mononucleosis.
- Protozoan: Malaria and kalaazar
- Parasitic: Hydatid.
Circulatory Of Splenomegaly:-
- Congestive cardiac failure
- Portal hypertension
- Hepatic or portal vein thrombosis
- Splenic vein obstruction.
Hematological Of Splenomegaly:-
- Hemolytic disorders: Hereditary spherocytosis, elliptocytosis, pyruvic kinase defiiency, etc.
- Hematological malignancies: Acute leukemia, chronic myeloid leukemia and lymphomas
- Myeloproliferative disorders: Polycythemia vera
- Inflmmatory and collagen disorders: Acute rheumatic fever, lupus erythematosus
- Granulomatous disorders: Sarcoidosis and berylliosis
- Metabolic storage diseases, i.e. Gaucher’s disease
- Splenomegaly ofunknown etiology: Tropical splenomegaly,nontropical splenomegaly.
Hereditary Blood Disorders
Question. Describe briefly causes of splenomegaly.
Or
Enumerate the causes of splenomegaly.
Or
Enumerate fie causes of splenomegaly.
Answer.
Splenomegaly is defined as the enlargement of the spleen. Spleen can be mildly, moderately and massively enlarged.
Classifiation of Splenomegaly as Per its Size
- Mild splenomegaly: In it spleen is mildly enlarged and weighs up to 500 gm.
- Moderate splenomegaly: In it the spleen is moderately enlarged weighs up to 500 to 1000 gm.
- Massive splenomegaly: In it the spleen is massively enlarged and weighs up to greater than 1000 gm.
Causes Of Splenomegaly
Infections Of Splenomegaly
- Bacterial: Septicemia, typhoid, infective endocarditis, TB,syphilis.
- Viral: Hepatitis, infectious mononucleosis.
- Protozoan: Malaria and kalaazar
- Parasitic: Hydatid.
Circulatory Of Splenomegaly
- Congestive cardiac failure
- Portal hypertension
- Hepatic or portal vein thrombosis
- Splenic vein obstruction.
Hematological Of Splenomegaly
- Hemolytic disorders: Hereditary spherocytosis, elliptocytosis, pyruvic kinase defiiency, etc.
- Hematological malignancies: Acute leukemia, chronic myeloid leukemia and lymphomas
- Myeloproliferative disorders: Polycythemia vera
- Inflmmatory and collagen disorders: Acute rheumatic fever, lupus erythematosus
- Granulomatous disorders: Sarcoidosis and berylliosis
- Metabolic storage diseases, i.e. Gaucher’s disease
- Splenomegaly ofunknown etiology: Tropical splenomegaly,nontropical splenomegaly.
Question. Enumerate the causes of cervical lymphadenopathy.
Or
Enumerate the causes of generalized lymphadenopathy.
Or
Enumerate the causes of lymphadenopathy.
Answer.
1. Infectious Diseases:
1. Viral infections:
- Infectious hepatitis
- Infectious mononucleosis
- AIDS
- Rubella
- Varicella
- Herpes zoster.
2. Bacterial infections:
- Streptococci
- Staphylococci
- Salmonella
- Brucella
- Listeria monocytogenes.
3. Fungal infections:
- Coccidioidomycosis
- Histoplasmosis
- Chlamydial Infections
- Lymphogranuloma venereum
- Trachoma.
4. Mycobacterial infections:
- Tuberculosis
- Leprosy
- Parasitic infestations
- Microfiariasis
- Toxoplasmosis.
5. Spirochetal diseases
- Syphilis
- Yaws
- Leptospirosis.
2. Immunologic Diseases:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Dermatomyositis
- Serum sickness
- Drug reactions: Phenytoin, hydralazine
- Primary biliary cirrhosis
- Chronic active hepatitis.
3. Malignant Disorders:
1. Haematologic disorders:
- Hodgkin’s lymphoma
- Myeloid leukaemia—blastic crisis
- Chronic lymphatic leukaemia
2. Metastatic tumours:
- Melanoma
- Kaposi’s sarcoma
- Tumours
- Lung
- Breast
- Prostate
- Kidney
- Head and neck
- Gastrointestinal tract.
4. Endocrine disease:
- Hyperthyroidism.
5. Lipid Storage disease:
- Gaucher’s disease
- NiemannPick disease.
6. Miscellaneous disorders:
- Sarcoidosis
- Amyloidosis
- Sinus histiocytosis.
Question. Describe the clinical and diagnostic features of Chronic Myeloid Leukemia.
Answer.
Chronic Myeloid Leukemia Common Features
- Nonspecific: Loss of weight, fatigue, malaise, excessive perspiration.
- Splenomegaly: Size of spleen is enlarged
- Bleeding, excessive menstrual or other bleeding.
- Anemia
- Bone pain: It is due to extension of hemopoiesis through long bones.
Chronic Myeloid Leukemia Rare Features
- Splenic infarction
- Leukostasis
- Gout
- Retinal hemorrhage
- Fever.
Chronic Myeloid Leukemia Diagnostic Features
Diagnosis is based on the clinical fidings and investigations.
Chronic Myeloid Leukemia Investigations
- Normocyticnormochromic anemia
- Mean WBC count is 220 × 109/L (range 9.5 to 600 × 109/L) or (2-6 lakhs/µL.)
- Mean platelet count is 445 × 109/L (range 162–2000 × 109/L)
Leucocyte alkaline phosphatase: Absent in granulocytes in CML - Plasma uric acid and alkaline phosphatase are increased Serum B 12 level is increased due to increase in transcobalamin III which is present in neutrophil granules.
- Bone marrow shows increased cellularity especially myeloid and megakaryocytic. Marrow and blood show basophilia, eosinophilia and monocytosis.
- Disease acceleration is denoted by
Blasts 10–19% in blood or bone marrow
- Basophils > 20% in blood or bone marrow
- Platelets < 100,000/µL unrelated to therapy or = 10,00,000/µL. unresponsive to therapy
- Increasing splenic size
- Increasing WBC count unresponsive to therapy
- Cytogenetic clonal evolution
- Progressive anemia.
Blastic crisis is established by:
- Blasts > 20 % in bone marrow or peripheral blood smear
- Extramedullary blast formation.
- Large foci or clusters of blasts in bone marrow.
All patients have evidence of translocation by cytogenetics,florescent in situ hybridization, or by molecular methods.
Question. Write short note on approach to investigate a case of Lymphadenopathy.
Or
How will you investigate a case of Lymphadenopathy?
Or
Write short answer on Lymphadenopathy.
Answer. History
- Age: Tuberculous lymphadenitis in childhood,secondary carcinoma in old age.
- Occupation: Tularemia in hunters and butchers; sporotrichosis in farmers and gardeners.
- Duration
- Acute swelling of a few days duration mostly pyogenic.
- Subacute lymphadenitis of 3–4 weeks duration may be due to streptococcal infection, tuberculosis, secondary syphilis, infectious mononucleosis or tularemia.
- Chronic lymphadenopathies include tuberculosis,lymphomas, leukemia, primary lymphatic tumours and secondary carcinoma. History of previous radiation treatment or operative removal.
Lymphadenopathy Physical examination
local
1. Number ofglands: Single gland may appear to be affcted for some time in tuberculosis, Hodgkin’s and secondary carcinoma. Multiple in tuberculosis, Hodgkin’s disease, leukemia.
2. Site:
- Neck usual site for tuberculous lymphadenitis, lymphosarcoma, and most other lymphadenopathies.
- Inguinal gland enlargements may be due to syphilis, lymphogranuloma inguinale or chancroid.
- The infraclavicular glands are seldom so enlarged as to be palpable except in secondary cancer or Hodgkin’s disease.
- Supratrochlear (epitrochlear) lymphadenopathy in non
- Hodgkin’s lymphoma, chronic lymphocytic leukemia, infectious mononucleosis, secondary
syphilis, sarcoidosis, IV drug abuse. - Hilar and superior mediastinal lymphadenopathy in tuberculosis, histoplasmosis, sarcoidosis,pneumoconiosis, malignancy and cryptococcosis.
3. Character: Discrete in Hodgkin’s disease and leukemia,primary tumors of lymphatic tissue and so called “lymphadenoid” form of tuberculous lymphadenitis.
Moveable, discrete and painless in sarcoidosis. Mattd together in tuberculosis and lymphogranuloma.
4. Cold abscess: In tuberculosis, lymphogranuloma, tularemia and sporotrichosis. Tuberculous glands may break through to give a typically indolent ulcer with undermined edges.
5. Primary cause: In the area drained by the enlarged glands; e.g. scalp if occipital or posterior auricular glands, fauces and pharynx in upper anterior cervical group, etc. Healed scar at portal of entry, scar of operative removal, or of radiation treatment.
Lymphadenopathy Systemic
1. Skin:
- Cutaneous tumors mostly on the face, usually in chronic lymphatic leukemia. Sometimes generalized erythroderma, polymorphic rashes and purpura.
- Rash of secondary syphilis.
- Painless papules without surrounding erythema may be found on face, arms and legs in sarcoidosis.
- Eruption of lupus erythematosus.
2. Lungs: Pulmonary or mediastinal tuberculosis, lesions of sarcoidosis or metastatic or primary deposits in carcinoma.
3. Abdomen: Abdominal glands may be palpable in tuberculosis. Enlargement of spleen and liver in leukemia and Hodgkin’s disease.
4. Genitalia: Scar of primary sore of syphilis, or “chancre” in lymphogranuloma.
5. Icterus: Jaundice with lymphadenopathy may be met with in viral hepatitis (cervical glands), lymphoma, acute lymphocytic leukemia, disseminated TB.
6. (f) Temperature: Raised in Hodgkin’s disease, infectious mononucleosis and tularemia.
Lymphadenopathy Investigations
- Blood picture: For diagnosis of leukemia and infectious mononucleosis. Positive ANA and reduced complement C4 levels in SLE.
- Special tests: Serologic tests for syphilis. PaulBunnell or monospot test for infectious mononucleosis,Agglutination reaction and animal inoculation in tularemia. Autoantibodies in SLE.
- Liver biopsy useful in sarcoidosis and infectious mononucleosis. Serological tests for HIV infection.
- Radiography of lungs and gastrointestinal tract. Skeletal changes in Boeck’s sarcoid and sporotrichosis (multiple small areas of decalcifiation).
- Biopsy: Needle aspiration biopsy is useful for initial evaluationofsuperfiiallymphadenopathy. Itis howevernot helpful in diagnosis of lymphomas and other hematologic malignancies. Lymphnode biopsy tissue should be processed for culture of appropriate organisms, frozen in
liquid nitrogen for lymphocyte typing or special studies for malignant cell types, and for routine histological studies. - CT scan of abdomen in lymphoma.
- Lymphangiography of value in diagnosing site, extent,and, in certain cases, even the nature of primary lymph node enlargement.
Question. How will you investigate a case of Anemia?
Answer. Every case of anemia should have the following investigations to detect degree and cause of anemia:
- Hemoglobin count decreases.
- RBC count, packed cell volume, mean corpuscular volume and mean corpuscular hemoglobin concentration (MCHC).
- Total leukocyte count and
diffrential leukocyte count. - Peripheral blood fim for type of anemia and shape of RBCs and presence of any abnormal cells.
- Clottng time and bleeding time inhemolytic anemia.
- Blood platelets.
Bone marrow examination is done, when cause of anemia requires further investigation, especially to detect type of erythropoiesis.
Anemia Other Investigations
- Stools for parasites: Test for presence of blood and stools is done in patients suspected to chronic blood loss.
- Urine for albumin, bile salt, pigments and urobilinogen
- Gastric analysis: Histamine fast achlorhydria in pernicious anemia and megaloblastic anemia.
- Studies for detecting steatorrhea and malabsorption studies.
- Schilling test for vitamin B12 absorption in megaloblastic and dimorphic anemias.
- F IGLU test is done to assess folic acid defiiency. 15 gram of histidine hydrochloride is given by mouth and the urine in which it is excreted it is collected over next eight hours.
Normal excretion is 1–17 mg
Question. Enumerate the causes of Iron Defiiency Anemia. How will you treat iron defiiency anemia?
Answer.
Following are the causes of iron-defiiency anemia:
1. Due to increased blood loss:
- Gastrointestinal: Peptic ulcer, piles, hookworm manifestation, carcinoma of stomach, acute erosive gastritis, ulcerative colitis
- Lung: Due to hemoptysis
- Renal: Hemoglobinuria and hematuria
- Uterine: Menorrhagia, postmenopausal uterine bleeding.
- Nose: Epistaxis
2. Due to increased body demands:
- In adolescence
- During prematurity
- In pregnancy and lactation.
3. Due to inadequate dietary intake:
- In low socioeconomic status
- In elder patients with loss of teeth
- Anorexia of pregnancy.
4. Decreased absorption:
- In achlorhydria
- In patients with malabsorption
- In cases with gastrectomy.
Treatment of Iron Defiiency Anemia
- Oral iron therapy: Ferrous sulphate 200 mg TID is given in between the meals. If after taking the drug, there is any abdominal pain, nausea, vomiting or constipation, the salt is changed to ferrous gluconate or ferrous fumarate.
Oral iron therapy should be given for 6 months. Iron absorption is enhanced by combining iron salts with hydrochloric acid, ascorbic acid, succinic acid, fructose, cysteine, isonine and cobalt. Administration of iron after food minimizes gastric upset. - Parenteral iron therapy: Iron sorbitol ciric acid complex 1.5 mg/Kg body weight is given as IM or Iron dextran in 5% glucose is given as IV A small test dose should be given IV before giving total dose. Total dose of iron should not exceed 2.5 g
- Blood transfusion: Packed red cells are transfused.
Question. Discuss causes of bleeding.
Answer.
- Bleeding can be the result of inability to form a temporary clot or the inability to form a defiitive clot.
- Inability to form a temporary clot results from inadequate platelet count, i.e. thrombocytopenia or abnormal platelet function, i.e. thrombocytopathy.
- Inability to form a definitive clot results from abnormalities in clottng factor.
- Disseminated intravascular coagulation and hemophilia results in bleeding.
- Idiopathic thrombocytopenic purpura
- Aplastic anemia
- Leukemia.
Question. Write short note on massive splenomegaly.
Answer. A clinically palpable spleen is called splenomegaly and it may be mild, moderate and massive.
When weight of spleen is over 1000 g, it is massive.
Causes
- Chronic myeloid leukemia
- Chronic malaria
- Kalaazar
- Myelofirosis
- Hairy cell leukemia
- Banti’s disease (tropical splenomegaly)
- Myeloid metaplasia
- Gaucher’s disease
- Hepatic vein obstruction.
Question. Write short note on diffrential diagnosis of massive splenomegaly.
Answer. When there is enlargement of spleen with its weight greater than 1000 g, it is known as splenomegaly.
massive splenomegaly Differential Diagnosis
Cirrhosis of liver:
- Symptoms and signs ofhepatocellular failure: Spider nevi,liver palms, alopecia, gynecomastia and testicular atrophy in males, icterus, Foetor hepaticus. Palpable enlarged liver.
- Evidence ofportal hypertension: Ascites, prominent veins on abdomen, hematemesis, piles.
- Diagnosis by liver biopsy demonstration of oesophageal varices by barium swallow, laparoscopy and scanning.
Infections, subacute and chronic:
Chronic malaria:
- History of fever with rigors with classical features of the attck like cold stage, hot stage, sweating stage.
- Spleen very large and fim.
- Liver may be enlarged.
- Severe anemia.
- Malarial parasites in peripheral blood or sternal marrow.
- Leucopenia.
- Therapeutic test with adequate dose of antimalarial drug during fever.
Kalaazar:
- Residence in endemic area.
- Splenomegaly: which may be massive.
- Recurrent fever: Double rise of temperature in 24
hours may be seen. - Liver enlarged but not grossly like spleen.
Anaemia. - Loss of hair and pigmentation of skin.
- Generalized lymphadenopathy especially in children. Nodes are soft, nontender.
- Other features are cough, hemorrhagic features
- LD bodies—on stained material from bone marrow or splenic aspirate.
Sub-acute infective endocarditis:
- Unexplained fever.
- Presence of cardiac murmur.
- Presence of petechiae, anemia, peripheral emboli,
clubbing of figers. - Red cells in urine.
- Positive blood culture.
Brucellosis:
- History of ingestion of raw milk, or occupation hazard in veterinary surgeons, laboratory personnel or slaughter house workers.
- Patient not toxic inspite of high fever.
- Spleen of moderate size, rarely massive.
- Liver may be enlarged, particularly, if spleen is very large.
- Back pain common.
- Culture of organism from blood or bone marrow.
- Complement fiation and anti-human globulin tests in chronic infection.
Tuberculous splenomegaly: In rare cases, tuberculous enlargement ofspleen occurs with litte involvement of other organs.
Blood picture shows anemia, leucopenia or thrombocytopenia either single or in combination.
Weakness, lassitude, loss of weight and often pyrexia.
Bleeding may occur. Xray of spleen may demonstrate areas of calcifiation.
Question. Write short note on Purpura.
Answer. Any rash in which blood cells leak into the skin or mucusmembrane, usually at multiple sites.
Purpuric rashes are often associated with disorders of coagulation or thrombosis.
Pin point purpuric lesions are called as petechiae, large hemorrhage into the skin are called as ecchymoses.
Types Of Purpura
- Allergic purpura: Any of a group of purpuras caused by a variety of agents, including bacteria, drugs and food.
- Anaphylactic purpura or Henöch-Schönlein purpura: A form of small vessel vasculitis that affcts children more commonly than adults, it is marked by abdominal pain, polyarticular joint disease and purpuric lesions of the lower extremities.
- Idiopathic thrombocytopenic purpura or hemorrhagic purpura:
It is hemorrhagic autoimmune disease in which there is destruction of circulating platelets, caused by autoantibodies that bind with antigen on the platelet membrane.
Symptoms
- Bleeding from nose, the gums or the gastrointestinal tract.
- Physical fidings include petechiae, especially on the lower extremities and ecchymoses.
laboratory Findings
Platelet count is usually less than 100, 000 per cumm.
Treatment
- If patient are asymptomatic and platelet count is about 40,000 per cumm, treatment is unnecessary.
- For symptomatic patients, treatment regimen include high dose corticosteroid, IV immunoglobulin, splenectomy.
Question. Write short note on Thrombocytopenia.
Or
Write short answer on thrombocytopenia.
Answer. Thrombocytopenia means decreased platelet count, i.e. less than 1,50,000 per cumm.
Etiology
Impaired platelet production:
- Due to impaired platelet production:
- Bone marrow failure:
- Aplastic anemia
- Leukemia
- Megaloblastic anemia
- Myelofirosis
- Marrow infitration.
- Selective suppression of platelet production Drugs such as sulpha drugs, rifampicin, thiazides, etc.
Increased consumption or destruction of platelets.
- Disseminated intravascular coagulation
- Thrombotic thrombocytopenic purpura
- Idiopathic thrombocytopenic purpura
- Gramnegative septicemia
- Viral infection.
Increased splenic sequestration.
- Hypersplenism
- Lymphoma
- Liver diseases.
Clinical Features
- As the count of platelets is above 1 lakh per cumm of blood, patient remain asymptomatic and bleeding time is also normal.
- As count of platelets is in between 50,000 and 1 lakh per cu mm of blood, bleeding is increased. At this stage, bleeding occur with severe trauma.
- As count of platelets reaches below 50,000, bruising is present along with purpura. At this stage, bleeding occur along with minor trauma.
- Platelet count less than 20,000 per cu mm of blood causes spontaneous bleeding.
Question. Describe drug treatment of AML.
Answer. Drug treatment
- Induction of remission
Daunorubicin IV alternate days 3 doses.
Cytosine arabinoside IV BD for 10 days - Thioguanine oral BD for 10 days.
- Consolidation phase: Repeat cycle of drugs used for inducing remission, consolidation phase ranges upto 2 years.
- Cranial prophylaxis: Not required since cranial involvement only in few cases.
- Maintenance phase: Generally maintenance therapy is not required since intensive treatment in remission and consolidation phase sufficient to give relief. If relapse occurs use of ablative therapy supported by allogenic or autologous bone marrow transplantation.
Question. Write short note on thalassemia.
Answer.
- Thalassemias are genetic disorders of hemoglobin synthesis in which there is reduced production of one or more chains of hemoglobin.
- This results in a relative excess production of either a chains or b chains, which without their partner chains are unstable and precipitate in RBCs or their precursors.
- The inclusion bodies produced by this process increase the rigidity of RBCs and result in their destruction, either in the marrow or the circulation or both. Hence the anaemia of thalassemia results from ineffctive erythropoiesis due to intramedullary RBC destruction, and a shortened RBC survival caused by haemolysis.
- Thalassemias are classified according to the particular globin chain that is ineffctively produced.
- In alpha thalassemia there is reduced rate of chain synthesis.
Beta thalassemias are associated with synthesis of beta chains. - Beta thalassemias is divided into two forms i.e. thalassmias minor and thalassemia major
Thalassemia Clinical Features
- Onset: Affcted children fail to thrive from about third month and become progressively more anaemic.
- Increasing pallor is present
- Splenomegaly: Haern siderosis with extramedullary haematopoiesis
- Facies: Frontal bossing due to thickening of cranial bones and prominent cheek bones due to overgrowth of zygomatic bones.
- Mild haemolytic jaundice
- Increased susceptibility to infections
- Hepatomegaly: Due to extramedullary haemopoiesis in fist 3-4 years. Later on further enlargement due to haemosiderin deposits in Kupffr cells.
- Cardiac involvement: Myocardial haemosiderin may result in arrhythmias and cardiac failure.
- Endocrines:
- Stunted growth from growth hormone defiiency
- Delayed puberty due to hypothyroidism
- Hypoparathyroidism can cause osteoporosis and fractures
- Diabetes mellitus due to iron deposits in Islet of Langerhans
Thalassemia Investigations
Hematological:
- Anemia: It is moderate-to-severe with 10 to 12 g/dL.
RBCs are microcytic hypochromic. Target cells are present and basophilic stippling is common. Also presence of tear drop, elliptical, fragments in red cells and at times red cell with HowellJolly body. - Reticulocytosis is present.
- Leucocytosis with few metamyelocytes and myelocytes
Biochemical:
- Reduced serum haptoglobins
- Bilirubin (unconjugated) increased and urine urobilinogen increased
- Iron status
- Serum iron and ferritin markedly increased.
- Total iron binding capacity (TIBC) is reduced.
Bone marrow:
- Erythroid hyperplasia with reversed M : E ratio
- Normoblastic erythropoiesis
- Ineffctive erythropoiesis — Some normoblasts die in the marrow without maturing into red cells
- Myelopoiesis and Megakaryopoiesis
- Increased bone marrow iron
Thalassemia Other special tests:
- HbF levels are high.
- Hb electrophoresis: Bands of both HbA and HbF in β-thalassemia.
- Global chain synthesis: α-β globin chain synthesis ratio altered (normal l : l) due to lack ofsynthesis ofβ chains.
- DNA analysisuseful for predicting disease severity and diagnosis.
- Liver spectrometry for detecting hemosiderosis of liver.
Thalassemia Management
- Blood transfusions should be done to keep level of hemoglobin between 9–11 gm%, if infant’s Hb. 6–7 gm% and failure to thrive. Transfusions are given every 2 to 4 weeks.
- Chelating agent such as desferrioxamine as S.C. infusion using a syringe driver pump/infuser.
- Splenectomy: Hypersplenism due to splenomegaly causes neutropenia and increased need for blood transfusion.
Splenectomy reduces severity of neutropenia and subsequent infections. Splenectomy should be done as late as possible. - Bone marrow transplantation: Indication for bone marrow transplantation in cases where matched siblings are available in a family, if not available, to look for a matched related donor. This is curative for the patient.
- Folic acid supplements should be given to the patient.
Question. Write causes of Hemolytic Anemia.
Answer.
Hemolytic anemia is a reduction in number of circulating red cells from there premature destruction.
Hemolytic Anemia Etiological Classifiation
1. Acquired or E xtracorpuscular
1. Immunohemolytic anemia:
- Autoimmunohemolytic anemia
- Warm antibody autoimmune hemolytic anemia
- Cold antibody autoimmune hemolytic anemia
- Drug induced immunohemolytic anemia
- Iso immune hemolytic anemia.
2. Mechanical trauma: Microangiopathic hemolytic anemia
3. Direct toxic effct: Malaria, bacteria, infection and other agents
4. Acquired red cell membrane abnormalities: Paroxysmal nocturnal hemoglobinuria.
5. Splenomegaly.
2. Hereditary or Intracorpuscular
1. Abnormalities ofred cell membrane:
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Hereditary stomatocytosis.
2. Disorders ofred cell interior:
- Red cell enzyme defect:
- Defects in HMP shunt: G6PD defiiency
- Defects in glycolytic pathway: Pyruvate kinase defiiency.
3. Disorders ofhemoglobin:
- Structurally abnormal hemoglobin, sickle syndrome and other hemoglobinopathies.
- Reduced globin chain synthesis: Thalassemias.
Hemolytic Anemia Clinical Features
- There is presence of high fever, toxemia, marked*prostration, shock and hemoglobinuria
- Acute renal failure may develop
- Chronic form includes jaundice varying from mild to severe form, mongoloid faces, splenomegaly, chronic leg ulcers and pigment stones in gallbladder.
Investigations or diagnosis for Hemolytic anemia
Test of Increased red cell Breakdown
- Blood fim shows normocytic normochromic or dimorphic anemia.
- Unconjugated serum bilirubin is raised
- Urine urobilinogen is raised but bilirubinuria is absent
- Serum hepatoglobin is reduced
- Plasma LDH is increased
- There is evidence of intravascular hemolysis i.e. hemoglobinaemia, hemoglobinuria, metnemoglobinaemia,hemosiderinuria.
Test Of Increased Red Cell Production
Reticulocyte count get increased
- Blood film shows macrocytosis, polychromasia and presence of normoblasts
- Bone marrow examination shows erythroid hyperplasia with raised iron store.
- X ray of bones show expansion of marrow space in bones such as skull.
Test Of Damage To Red Cells
- Blood fim show microspherocytes and fragmented RBCs.
- Osmotic fragility is increased.
- Electrophoresis test is done for abnormal hemoglobin
- Estimation of Hemoglobin A2 should be done
- Estimation of Hemoglobin F should be done
- Test for sickling is done
- Screening test for G6PD defiiency is done
Test For Shortened Red Cell Survivor
- Chromium labeled method show short red cell life span.
Treatment Of Hemolytic Anemia
- Patients with compensated hemolytic process need no treatment.
- Mainly management is general and specifi.
- Folic acid 5mg is given routinely and lifelong in patients with inherited hemolytic disorders
- Patients having hereditary spherocytosis may undergo splenectomy if they have moderate to severe disease or have experienced episodes of hemolytic crisis or gall stones.
Question. Describe various bleeding disorders and their management in detail.
Or
Write notes on bleeding disorders.
Answer.
Etiology Of Bleeding Disorders
Vascular Defects
- Bleeding disorders caused by vascular defects may be caused by structural malformation of vessels.
- Hereditary disorders of connective tissue and acquired connective tissue disorders.
- Vascular defects rarely cause serious bleeding.
- Bleeding into skin or mucous membrane starts immediately alter trauma but ceases within 24 to 48 hours.
- The vascular defects are hereditary hemorrhagic telangectasia, HenochSchönlein purpura.
Platelet Disorder:
It can be of two types:
- Reduction in number—Thrombocytopenic purpura. If the total number of circulating platelets falls below 50,000 per mm3 of blood the patient can have bleeding.
In some cases,the total platelet count is reduced by unknown mechanism,this is called primary or idiopathic thrombocytopenic purpura (ITP).
Chemicals, radiation and various systemic disease (e.g. leukemia) may have direct effct on the bone marrow and may result in secondary thrombocytopenia. - Defect in quality: Nonthrombocytopenic purpura, e.g.von Willebrand’s disease, Bernard-Soulier disease,Glanzmann’s thrombasthenia von Willebrand’s disease (pseudohemophilia) is the most common inherited bleeding disorder. Unlike hemophilia, it can occur in females. This is a disease of both coagulation factors and platelets. It is caused by an inherited defect involving platelet adhesion. Platelet adhesion
is affcted because of a defiiency of von Willebrand`s factor. - Various drugs such as carbamazepine, aspirin, methyl dopa, phenytoin can also lead to platelet disorders.
Coagulation Defects
- Hemophilia A: It is the most common coagulation defect. It is inherited as Xlinked recessive trait.
The hemostatic abnormality in hemophilla A is caused by a defiiency/defect of factor VIII.
Until recently, factor VIII was thought to be produced by endothelial cells and not by the liver as most of coagulation factors.
The defective gene is located on the Xchromosome. - Hemophilia B (Christmas disease): Factor IX is defiient or defective.
It is inherited as Xlinked recessive trait.
Like HemophiliaA, the disease primarily affcts males and the clinical manifestations of the two are identical. - Disseminated intravascular coagulation (DIC): It is a condition that results when the clotting system is activated in all or a major part of vascular system.
Despite widespread firinproductionthe major clinical problem is bleeding not thrombosis.
DIC is associated with a number of disorders such as infection, obstetric complications, cancer and snakebite.
Management of Bleeding disorders
Hereditary Hemorrhagic telangectasia
It is transmittd as autosomal dominanttraitand is characterized by bleeding from mucous membrane.
Management
- In patient having repeated attacks of epistaxis septal dermoplasty should be done. In septal dermoplasty, involved mucosa get removed and skin grafting is done.
- If spontaneous hemorrhages are present or nasal bleeding is present, then it is controlled by giving pressure packs.
- Sclerosing agents,, i.e. sodium tetradecyl sulphate, if injected intralesionally stop bleeding.
- Electrocautery is done. It helps in arresting bleeding.
Idiopathic thrombocytopenic Purpura (ItP)
Steroid Treatment Protocol
- Initial steroid treatment protocol forITP: Initial steroid treatment protocol l mg/kg/day prednisone, PO for 2-6 weeks.
- Subsequent steroid treatment protocol for ITP: Prednisone dose is individualized for every patient.
Usually, the dose of prednisone is tapered to less than l0 mg per day for 3 months and then withdrawn.
Splenectomy is done, if discontinuation of prednisone causes a relapse. - Follow the ’rule of twos’ for major dental treatment and provide extra steroids prior to surgery, if the patient is currently on steroids or has used steroids for 2 weeks longer within the past 2 years.
Idiopathic thrombocytopenic Purpura Minor Surgery
- Hemostasis after minor surgery is usually adequate, if platelet levels are above 50,000 cells/mm3.
- Platelets can be replaced or supplemented by platelet transfusions; though sequestration of platelets occurs rapidly. Platelet transfusion is indicated for established thrombocytopenic bleeding.
- When given prophylactically platelets should be given half before surgery to control capillary bleeding and half at the end of the operation to facilitate the placement of adequate sutures.
- Platelets should be used within 6–24 hours after collection and suitable preparations include platelet rich plasma (PRP), which contains about 90% of the platelets from a unit of fresh blood and plateletrich concentrate (PRC), which contains about 50% of the platelets from a unit of fresh whole blood.
- PRC is thus the best source of platelets. Platelet infusions carry the risk of isoimmunization, infection with bloodborne viruses and, rarely, graftversushost disease
- Where there is immune destruction of platelets (e.g. in ITP), platelet infusions are less effctive.
- The need for platelet transfusions can be reduced by local hemostatic measures and the use of Desmopressin or tranexamic acid or topical administration of platelet concentrates.
- Absorbable hemostatic agents such as oxidized regenerated cellulose (Surgical), synthetic collagen (lnstat) or microcrystalline collagen (Avitene) may be put in the socket to assist clottng in postextraction socket.
- Drugs that affct platelet function, such as gentamicin, antihistamines and aspirin should be avoided.
Idiopathic thrombocytopenic Purpura Major Surgery
For major surgery platelet levels over 75,000 cells/mm3 are desirable.
Von Willebrand Disease
- It is the most common inherited bleeding disorder. It is inherited as autosomal dominant but a severe form of disease may be inherited as a sexlinked recessive trait.
- It is caused due to the deficiency or defect in Von Willebrand factor.
- Types of Von-Willebrand diseases are: Type I, Type II A and II B, Type III
Von Willebrand Disease Management
- Surgical procedures can be performed in patients with mild von Willebrand disease by using DDAVP and EACA.
Patients with severe Von Willebrand disease requires cryoprecipitate and Factor VIII concentrate. - Bleeding should be controlled by using local measures such as pressure packs, gelfoam with thrombin, tranexamic acid, etc.
- Aspirin and NSAIDs are avoided and acetaminophen can be given to patients.
- In majority of patients with von Willebrand disease hemostatic defect is controlled with desmopressin via nasal spray.
- Type I vonWillebrand disease is treated withdesmopressin while Type II A and B and Type III require clottng factor replacement.
Disseminated Intravascular Coagulation Management
- Correction of hemodynamic instability by flid therapy,transfusion of packed cells or whole blood.
- Factor replacement: This is the specifi therapy, in this fresh frozen plasma, cryoprecipitate, platelet concentrate transfusions are essential. Freshfrozen plasma is given at the dose of 15 mL/kg. Platelet is transfused at the dosage of 0.1 unit/kg.
Question. Discuss causes, diagnosis and management of iron Defiiency Anemia.
Answer.
Iron Defiiency Anemia Causes/ Etiology
1. Due to increased blood loss:
- Gastrointestinal: Peptic ulcer, piles, hookworm manifestation,
- Carcinoma of stomach, acute erosive gastritis, ulcerative colitis
- Lung: Due to hemoptysis
- Renal: Haemoglobinuria and hematuria
- Uterine: Menorrhagia, post menopausal uterine bleeding.
- Nose: Epistaxis
2. Due to increased body demands:
- In adolescence
- During prematurity
- In pregnancy and lactation.
3. Due to inadequate dietary intake:
- In low socioeconomic status
- In elder patients with loss of teeth
- Anorexia of pregnancy.
4. Decreased absorption:
- In achlorhydria
- In patients with malabsorption
- In cases with gastrectomy.
Iron Defiiency Anemia Management
- Proper physical and mental rest.
- Good nourishing diet with supplementation of foods rich in iron.
- Oral iron therapy: Ferrous sulphate 200 mg TID is given in between the meals. If after taking the drug, there is any abdominal pain, nausea, vomiting or constipation, the salt is changed to ferrous gluconate or ferrous fumarate. Oral iron therapy should be given for 6 months.
- Parenteral iron therapy: Iron sorbitol ciric acid complex 1.5 mg/kg body weight is given as IM or Iron dextran in 5% glucose is given as IV
Iron Defiiency Anemia Diagnosis
It is based on the clinical signs and symptoms and investigations
Iron Defiiency Anemia Clinical Signs And Symptoms
Symptoms
- Tiredness
- Weakness
- Lethargy
- Loss of appetite headache and bodyache
- Inability to concentrate
- Giddiness
- Breathlessness
- Epigastric discomfort.
Iron Defiiency Anemia Signs
- Pallor
- Palpitation
- Angular stomatitis
- Atrophic gastritis
- Flattning or spoon-shaped nails, i.e. platonychia and koilonychia
- Tongue is pale and smooth
- Glossitis
- Hepatosplenomegaly
- PlummerVinson syndrome, i.e. dysphagia and cricoid webs.
Iron Defiiency Anemia Investigations
Blood picture and red cell indices
- Hemoglobin: Fall on hemoglobin concentration.
- Red cells: The RBCs in blood fim are hypochromatic
and microcytic and there is anisocytosis, poikilocytosis and elliptocytosis - Reticulocyte count: Normal or reduced.
- Absolute values: MCV, MCH and MCHC are decreased.
- Leukocytes: Usually normal
- Platelets: Usually normal but raised if bleeding is cause of anemia
- ESR: value of ESR is low
Bone marrow fidings:
- Marrow cellularity: The marrow cellularity is increased due to erythroid hyperplasia.
- Erythropoiesis: Normoblastic erythropoiesis.
- Marrow iron is defiient.
Biochemical fidings:
- Serum iron level is low.
- Total iron binding capacity is high.
- Serum ferritin is very low.
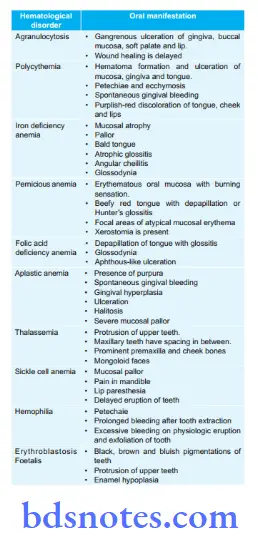
Question. Write notes on oral manifestations of Hematological Disorder.
Answer. Following are the oral manifestations of hematological disorders:

Question. Classify anemia and discuss Nutritional Anemias.
Answer. Classifiation of Anemia
Etiological Classifiation of Anemia(By lea and Febiger, 1981)
1. Loss of blood:
- Acute posthemorrhagic anemia
- Chronic posthemorrhagic anemia.
2. Excessive destruction of red blood corpuscles:
1. Extracorpuscular causes:
- Antibodies
- Infections like malaria
- Splenic sequestration and destruction
- Associated diseases like lymphomas
- Drugs, chemical and physical agents
- Trauma to RBC.
2. Intracorpuscular hemolytic diseases:
Hereditary
- Disorders of glycolysis
- Faulty synthesis or maintenance of reduced glutathione
- Qualitative or quantitative abnormalities in the synthesis of globulin
- Abnormalities in RBC membrane
- Erythropoietic porphyria.
Acquired
- Paroxysmal nocturnal hemoglobinuria
- Lead poisoning
Impaired blood production resulting from defiiency of substances essential for erythropoiesis:
- Iron defiiency
- Defiiency ofvarious B vitamins: Vitamin B12 and folic acid (pernicious anemia and megaloblastic anemia); pyridoxine responsive anemia
- Protein defiiency
- Possibly ascorbic acid defiiency.
Inadequate production of mature erythrocytes:
Defiiency of erythroblast
1. Atrophy ofbone marrow: Aplastic anemia
- Chemical or physical agents
- Hereditary
- Idiopathic.
2. Isolated erythroblastopenia
- Thymoma
- Chemical agents
- Antibodies.
Infitration ofbone marrow:
- Leukemia, lymphomas
- Multiple myeloma
- Carcinoma, Sarcoma
- Myelofirosis.
Endocrine abnormalities:
- Myxedema
- Addison’s disease
- Pituitary insuffiency
- Sometimes hyperthyroidism.
- Chronic renal failure.
Chronic inflmmatory disease: - Infectious
Noninfectious including granulomatous and collagen disease. - Cirrhosis of liver.
Morphological Classifiation of Anemia
Based on the red cell size, hemoglobin content and red cell indices, anemias are classifid into 3 types:
1.Microcytic, hypochromic: MCV, MCH, MCHC are all reduced, e.g. in iron defiiency anemia and in certain noniron defiient anemias (sideroblastic anemia, thalassaemia,anemia of chronic disorders).
2.Normocytic, normochromic: MCV MCH, MCHC are all normal, e.g. after acute blood loss, hemolytic anemias,bone marrow failure, anemia of chronic disorders.
3.Macrocytic: MCV is raised, e.g. in megaloblastic anemia due to defiiency of vitamin B12 or folic acid.
Nutritional Anemias
Following are the nutritional anemias:
- Iron defiiency anemia
- Macrocytic anemia.
1. Due to increased blood loss:
- Gastrointestinal: Peptic ulcer, piles, hookworm manifestation,
- Carcinoma of stomach, acute erosive gastritis, ulcerative colitis
- Lung: Due to hemoptysis
- Renal: Haemoglobinuria and hematuria
- Uterine: Menorrhagia, post menopausal uterine bleeding.
- Nose: Epistaxis
2. Due to increased body demands:
- In adolescence
- During prematurity
- In pregnancy and lactation.
3. Due to inadequate dietary intake:
- In low socioeconomic status
- In elder patients with loss of teeth
- Anorexia of pregnancy.
4. Decreased absorption:
- In achlorhydria
- In patients with malabsorption
- In cases with gastrectomy.
Macrocytic Anemia
Macrocytosis is the rise in mean cell volume or red cells above the normal range. It is due to vitamin B12 defiiency or folic acid defiiency.
Macrocytic Anemia Etiology
1. Vitamin B12 defiiency
- Inadequate intake:
- In strict vegetarians
- In poor diet.
Due to malabsorption:
- Gastric:
- Pernicious anemia
- Congenital intrinsic factor defiiency
- Gastrectomy.
- Small intestinal disease:
- Topical and Nontopical sprue
- Crohn’s disease
- Fish tapeworm.
- Increased requirement
- In pregnancy.
Macrocytic Anemia Folic acid defiiency
1. Inadequate intake
- Infancy
- Old age
- Poverty
- Alcoholism
- Kwashiorkor.
2. Malabsorption
- Coeliac Disease
- Topical sprue
- Congenital folate malabsorption.
3. Increased utilization or loss
1. Physiological
- Prematurity
- Pregnancy and lactation.
2. Pathological
- Blood disorders
- Malignancy
- Dialysis.
3. Antifolate Drugs
- Methotrexate
- Pyrimethamine
- Trimethoprim
- Anticonvulsant drugs.
Macrocytic Anemia Clinical Features
- Due to anemia: Shortness of breadth, anemia and pallor.
- Gastrointestinal: Diarrhea, loss of weight and apetite
- Neurological: Vitamin B12 neuropathy and neural tube defects due to defiiency of folic acid.
- Gonadal dysfunction: It is due to deficiency of both Vitamin B12 and folic acid
- Epithelial cell changes: Glossitis and other epithelial surfaces show cellular abnormalities.
Macrocytic Anemia Investigations
1. Vitamin B12 Defiiency:
- Hemoglobin levels are decreased below normal range.
- Mean corpuscular volume is raised.
- Peripheral blood fim examination reveals macrocytosis, poikilocytosis and hypersegmentation of the neutrophils
- Bone marrow examination reveals hypercellular marrow with megaloblastosis, giant metamyelocytes and platelets
- Serum iron and serum ferritin levels are raised.
- Schilling’s test is positive.
2. Folic acid defiiency:
- Serum folate levels are low
- Red cell folate levels are low
- Figlu test is positive.
Macrocytic Anemia Treatment
Vitamin B12 Defiiency:
- Hydroxycobalamine 1000 µg IM is given, i.e. 6 injections in 2 to 3 weeks.
- Since rapid regeneration of blood deplete marrow iron stores, so ferrous sulphate 200 mg daily is given after starting the therapy.
- Maintenance dose of 500–1000 μg IM is given for every 3 months.
Folic acid defiiency:
- InitiallyFolicacid 5 mgdailyorallyfor4months isgiven.
- Maintenance dose is 5 mg folic acid once a week.
Question. Write Hodgkin’s lymphoma under following headings:
- Hodgkin’s lymphoma Clinical Features
- Hodgkin’s lymphoma Investigations
- Hodgkin’s lymphoma Staging
- Hodgkin’s lymphoma Treatment
Answer. Hodgkin’s disease is a clinically and histologically distinct chronic lymphoproliferative disorder of unknown etiology.
Hodgkin’s lymphoma Clinical Features
Hodgkin’s lymphoma Local Signs
- Lymphadenopathy: Superfiial lymph nodes in neck are fist to enlarge at fist one side and then other. On palpation, lymph nodes are painless, leathery and discrete. In advanced cases there is a pyramidal swelling with base at clavicle and apex at angle of the jaw.
- Splenomegaly: Moderate enlargement is present.
- Hepatomegaly: Moderate and nontender
Hodgkin’s lymphoma Systemic Symptoms
- Presence of cachexia and loss of weight
- Fever is present. It can be of mild grade or undulant for several days or can be continuous.
- Night sweats are present
- Anemia can be present
- Generalized or refractory pruritus
Hodgkin’s lymphoma Features due to Metastatic Growth
- In skin: pruritus, erythema, herpes zoster
- In bones: localized pain and tenderness
- Nervous system: Paresthesia and pain
- Respiratory tract: Paralysis of larynx, Collapse of lung,pleural effsion
- Gastrointestinal: Jaundice and ascites
- Genitourinary: Hematuria, retention of urine and pain in back
Due to Immunologic changes
- Lowering of resistance to infection
- Homolytic anemia
Hodgkin’s lymphoma Investigations
1. Blood test:
- Non-specifi anemia of chronic disease is common
- Lymphopenia is present.
- ESR is elevated
2. Lymph node biopsy:
- Show presence of reedsternberg cells.
3. Imaging:
- Chest Xray to look for mediastinal lymph nodes and pleural effsion.
- CT is valuable in detecting intrathoracic and abdominal lymphadenopathy. It can also detect presence or absence of bone marrow involvement after chemotherapy.
- Bone marrow: Aspiration biopsy is indicated in stage II disease and higher staging.
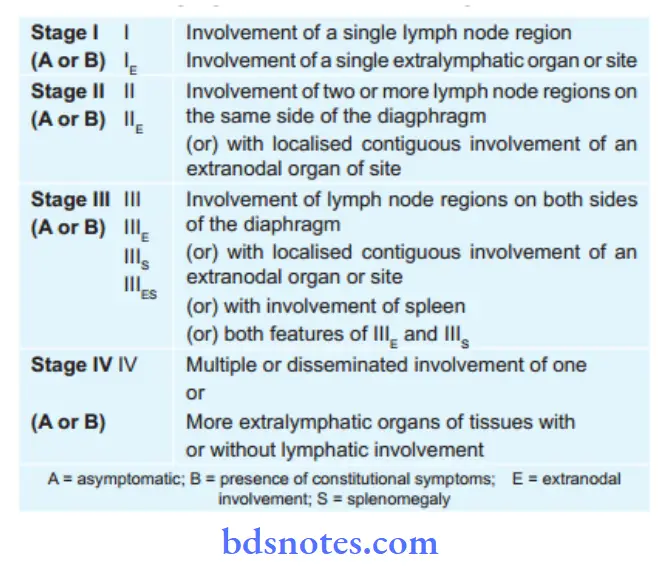
Hodgkin’s lymphoma Staging
Ann Arbor Staging Classifiation of Hodgkin’s Disease
Hodgkin’s lymphoma Treatment
Hodgkin’s lymphoma Treatment stage I and II
- Mainly radiotherapy is given, i.e. external high cobalt radiotherapy
- Above the diaphragm, Y fild therapy is given.
- Below the diaphragm, mantle or inverted Y fild therapy is given
- Chemotherapy should also be given.
- Involved fild radiation therapy is given to all sites ofbulky disease postABVD
Hodgkin’s lymphoma Treatment Stage III And Iv
- Mainly chemotherapy is given
- Drugs used are MOPP combination, i.e.
- Mustine—6 mg/m2 IV daily on days 1 and 8
- Oncovine—1.4 mg/m2 IV daily on days 1 and 8
- Procarbazine—100 mg/m2 orally on days 1–14
- Prednisolone—40 mg/m2 orally on days 1–14
- Give 6 courses with 2 weeks rest between the end of one course and beginning of next.
- ABVD combination is popular these days, i.e.
- Adriamycin: 25 mg/m2 IV on days 1 and 15
- Bleomycin: 10 mg/m2 IV on days 1 and 15
- Vinblastine: 6 g/m2 IV on days 1 and 15
- Dacarbazine: 150 mg/m2 I.V. on days 1 to 5
- Alternating MOPP with ABVD gives excellent response.
Question. Write short note on agranulocytosis.
Answer. It is defied as an acute disease marked by a defiit or absolute lack of granulocytic WBCs, i.e. neutrophils,basophils and eosinophils.
1. Endocrinal causes like hyperpituitarism, hypoadrenalism.
2. Agranulocytosis due to drugs: This is a very important cause and is related to dosage of drugs as well as sensitivity reaction. The main drugs are:
- Anticancer drugs
- Anti-inflmmatory drugs
- Phenothiazines and tranquilizers
- Sulfonamides and cotrimoxazole
- Antithyroid drugs
- Antidiabetic drugs
- Antihistaminics
- Antiepileptic drugs
- Antimicrobial agents
Clinical Manifestations
- Females are more commonly affcted than males
- Early manifestations of agranulocytosis are may be in form of sore throat or pain.
- There may be fever going up to 130°F, sometimes coming with rigor chills, body ache and pain and extreme degree of prostration.
- In large number of cases ulceromembranous lesions appear on throat, tonsils, gum, tongue and genitalia
- These are often covered with grayish black exudates and may become gangrenous.
- Lymph gland generally cervical groups and in some, there are generalized lymphadenopathy
- Liver and spleen may become enlarged.
- As disease progresses severe toxemia develops and patient may go into shock.
The diagnosis of agranulocytosis is based on clinical history and physical examination.
- Person with history of sore throat, fever with rigor and chills, body ache and extreme degree of prostration (absolute exhaustion).
- In large number of cases ulceromembranous lesions are present on throat, tonsil, gums, tongue and genitalia. The lesions are covered with grayish black exudates and become gangrenous.
- Confirmation of diagnosis is made by laboratory investigations.
- Peripheral blood fim shows complete absence of neutrophils.
- Bone marrow is hypocellular and there is depletion of myeloid elements.
Clinical Features Of Acute Leukemia
Following are the clinical features of acute leukemia:
1. Due To Bone Marrow Failure
- Constitutional symptoms: Fever, malaise and prostration
Due to anemia: Tiredness, fatigue, pallor, weakness and dyspnea. - Bleeding manifestations: Bruises, Petechiae, bleeding from gums and nose, purpura, gastrointestinal, renal and bleeding in nervous system.
- Infections: Infective lesions of oral cavity and throat, ulcers in oral cavity and pharynx, herpes simplex infection, Infections of respiratory tract such as bronchitis and pneumonia, infections of skin such as cellulitis and boils.
2. Due To Organ Infitration
- CNS: Hemorrhage, meningeal infitration and multiple cranial nerve palsies.
- Skin: Bluish nodules or dusky red patches.
- Kidneys: Renal failure
- Heart: Cardiomyopathy and pericarditis
- Fundus: Roth spots and papilledema
- Testes: Swelling present in acute lymphoid leukemia
- Bony tenderness is present especially in sternum
- Presence of hepatosplenomegaly and lymphadenopathy.
Due To Leukemic Cells
- Tissue deposits of leukemic cells leads to gum hypertrophy.
- Symptoms of cellular hyperviscosity are headache,confusion, fis, focal neurological signs and coma.
- In promyelocytic variant of acute myeloid leukemia the release of cytoplasmic granular contents activates coagulation and firinolytic systems which leads to acute hemostatic failure.
Folic Acid
Folic acid is a combination of glutamic acid, para-aminobenzoic acid and pteridine nucleus.
Folic acid Sources
Sources of folic acid are yeast, fresh green vegetables, cereals,liver, kidney, meat.
Folic acid Daily Requirement
50 to 100 μg.
Deficiency of Folic Acid
Deficiency of folic acid leads to megaloblastic anemia, glossitis,diarrhea, weight loss and weakness.
Folic acid Indications
- In megaloblastic anemia caused due to folate defiiency,folic acid is given in dose of 1–5 mg/day and is continued till 3–4 months.
- In pregnancy due to increase demand, it is given 0.5 mg/day from fist trimester.
- Folic acid antagonizes methotrexate toxicity.
Common Coagulation Disorders.
Write Down The Clinical Features, Investigations And Management Of Idiopathic Thrombocytopenic Purpura.
Coagulation disorders deal with disruption of the body’s ability to control blood clottng.
Common Coagulation Disorders are:
- Hemophilia, orhemophiliaA (FactorVIIIdefiiency),an inherited coagulation disorder. This genetic disorder is carried by females but most often affcts males.
- Christmas disease, also known as hemophilia B or
Factor IX defiiency, is less common than hemophilia
A with similar in symptoms. - Disseminated intravascular coagulation disorder,also known as consumption coagulopathy, occurs as a result of other diseases and conditions. This disease accelerates clottng, which can actually cause hemorrhage.
- Thrombocytopenia is the most common cause of coagulation disorder. It is characterized by a lack of circulating platelets in the blood. This disease also includes idiopathic thrombocytopenia.
- Von Willebrand’s disease is a hereditary disorder with prolonged bleeding time due to a clottng factor defiiency and impaired platelet function. It is the most common hereditary coagulation disorder.
- Hypoprothrombinemia is a congenital defiiency of clottng factors that can lead to hemorrhage.
- Other coagulation disorders include factor XI deficiency, also known as hemophilia C, and factor VII defiiency. Hemophilia C afflts one in
100,000 people and is the second most common bleeding disorder among women. Factor VII is also called serum prothrombin conversion accelerator (SPCA) defiiency. One in 500,000 people may be afflted with this disorder that is often diagnosed in newborns because of bleeding into the brain as a result of traumatic delivery.
Idiopathic Thrombocytopenic Purpura
It is considered to be the autoimmune disease of platelets.
Idiopathic Thrombocytopenic Purpura Clinical Features
Acute Idiopathic Thrombocytopenic Purpura
- It is seen commonly in children who are recovering from the viral disease.
- Onset of the disorder is sudden and symptoms are seen 2 to 3 weeks after the viral infection with appearance of purpura or at times epistaxis.
Chronic Idiopathic Thrombocytopenic Purpura
- This is seen during 2nd to 4th decades of life.
- It has female predilection.
- Patient has purpura or epistaxis.
- There is presence of ecchymoses and menorrhagia
- Internal bleeding can also be present.
- Splenomegaly can be present.
Chronic Idiopathic Thrombocytopenic Purpura Investigations
- Bleeding time becomes prolonged.
- Platelet count get decreased
- Bone marrow examination reveals increase in the number of megakaryocytes indicating peripheral destruction of platelets.
Chronic Idiopathic Thrombocytopenic Purpura Management
Chronic Idiopathic Thrombocytopenic Purpura In children
- Mild idiopathic thrombocytopenic purpura requires no treatment.
- In moderatetosevere idiopathic thrombocytopenic purpura prednisolone, 2 mg/kg daily oral administration is advised.
- Platelet transfusion can be given.
After giving steroidal therapy, if bleeding persist - immunoglobulins should be given.
Chronic Idiopathic Thrombocytopenic Purpura In adults
- In adults prednisolone should be given 1 mg/kg as standard regimen and is continued for 2 to 4 weeks, after this drug should be slowly withdrawn.
- If bleeding is high platelet infusion should be done.
- IV immunoglobulin should be given, i.e. 1 g/kg. This is to be given in the patients who are not responding to prednisolone therapy.
- If patient has more than two remissions of the disease splenectomy should be done.
Treatment of Anemias
Treatment of Anemias Etiology
1. Due to increased blood loss:
- Gastrointestinal: Peptic ulcer, piles, hookworm manifestation,
- Carcinoma of stomach, acute erosive gastritis, ulcerative colitis
- Lung: Due to hemoptysis
- Renal: Haemoglobinuria and hematuria
- Uterine: Menorrhagia, post menopausal uterine bleeding.
- Nose: Epistaxis
2. Due to increased body demands:
- In adolescence
- During prematurity
- In pregnancy and lactation.
3. Due to inadequate dietary intake:
- In low socioeconomic status
- In elder patients with loss of teeth
- Anorexia of pregnancy.
4. Decreased absorption:
- In achlorhydria
- In patients with malabsorption
- In cases with gastrectomy.
1. Anemias – Vitamin B12 defiiency
- Inadequate intake:
- In strict vegetarians
- In poor diet.
Anemias – Due to malabsorption:
- Gastric:
- Pernicious anemia
- Congenital intrinsic factor defiiency
- Gastrectomy.
- Small intestinal disease:
- Topical and Nontopical sprue
- Crohn’s disease
- Fish tapeworm.
- Increased requirement
- In pregnancy.
Folic Acid Defiiency
1. Inadequate intake
- Infancy
- Old age
- Poverty
- Alcoholism
- Kwashiorkor.
2. Malabsorption
- Coeliac Disease
- Topical sprue
- Congenital folate malabsorption.
3. Increased utilization or loss
1. Physiological
- Prematurity
- Pregnancy and lactation.
2. Pathological
- Blood disorders
- Malignancy
- Dialysis.
3. Antifolate Drugs
- Methotrexate
- Pyrimethamine
- Trimethoprim
- Anticonvulsant drugs.
1. Acquired or E xtracorpuscular
1. Immunohemolytic anemia:
- Autoimmunohemolytic anemia
- Warm antibody autoimmune hemolytic anemia
- Cold antibody autoimmune hemolytic anemia
- Drug induced immunohemolytic anemia
- Iso immune hemolytic anemia.
2. Mechanical trauma: Microangiopathic hemolytic anemia
3. Direct toxic effct: Malaria, bacteria, infection and other agents
4. Acquired red cell membrane abnormalities: Paroxysmal nocturnal hemoglobinuria.
5. Splenomegaly.
2. Hereditary or Intracorpuscular
1. Abnormalities ofred cell membrane:
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Hereditary stomatocytosis.
2. Disorders ofred cell interior:
- Red cell enzyme defect:
- Defects in HMP shunt: G6PD defiiency
- Defects in glycolytic pathway: Pyruvate kinase defiiency.
3. Disorders ofhemoglobin:
- Structurally abnormal hemoglobin, sickle syndrome and other hemoglobinopathies.
- Reduced globin chain synthesis: Thalassemias.
Treatment of Anemias Clinical Features
Anemias Symptoms
- Tiredness
- Weakness
- Lethargy
- Loss of appetite
- Headache and bodyache
- Inability to concentrate, giddiness
- Breathlessness
- Epigastric discomfort.
Anemias Signs
- Pallor
- Palpitation
- Angular stomatitis
- Atrophic gastritis
- Flattning or spoon-shaped nails, i.e. platynychia and koilonychia
- Tongue is pale and smooth
- Glossitis
- Hepatosplenomegaly
- PulmmerVinson syndrome, i.e. dysphagia and cricoid webs.
- Due to anemia: Shortness of breadth, anemia and pallor.
- Gastrointestinal: Diarrhea, loss of weight and apetite
- Neurological: Vitamin B12 neuropathy and neural tube defects due to defiiency of folic acid.
- Gonadal dysfunction: It is due to deficiency of both Vitamin B12 and folic acid
- Epithelial cell changes: Glossitis and other epithelial surfaces show cellular abnormalities.
- There is presence of high fever, toxemia, marked*prostration, shock and hemoglobinuria
- Acute renal failure may develop
- Chronic form includes jaundice varying from mild to severe form, mongoloid faces, splenomegaly, chronic leg ulcers and pigment stones in gallbladder.
Anemias Approach To Diagnosis
Anemias Diagnosis
It is based on the clinical signs and symptoms and investigations
Anemias Clinical Signs And Symptoms
Anemias Investigations
Blood picture and red cell indices
- Hemoglobin: Fall on hemoglobin concentration.
- Red cells: The RBCs in blood fim are hypochromatic and microcytic and there is anisocytosis, poikilocytosis and elliptocytosis
- Reticulocyte count: Normal or reduced.
- Absolute values: MCV, MCH and MCHC are decreased.
- Leukocytes: Usually normal
- Platelets: Usually normal but raised if bleeding is cause of anemia
- ESR: value of ESR is low
Bone marrow fidings:
- Marrow cellularity: The marrow cellularity is increased due to erythroid hyperplasia.
- Erythropoiesis: Normoblastic erythropoiesis.
- Marrow iron is defiient.
Biochemical fidings:
- Serum iron level is low.
- Total iron binding capacity is high.
- Serum ferritin is very low.
Anemias Treatment
- Proper physical and mental rest.
- Good nourishing diet with supplementation of foods rich in iron.
- Oral iron therapy: Ferrous sulphate 200 mg TID is given in between the meals. If after taking the drug, there is any abdominal pain, nausea, vomiting or constipation, the salt is changed to ferrous gluconate or ferrous fumarate. Oral iron therapy should be given for 6 months.
- Parenteral iron therapy: Iron sorbitol ciric acid complex 1.5 mg/kg body weight is given as IM or Iron dextran in 5% glucose is given as IV
- Blood transfusion: Packed red cells are transfused.
Vitamin B12 Defiiency:
- Hydroxycobalamine 1000 µg IM is given, i.e. 6 injections in 2 to 3 weeks.
- Since rapid regeneration of blood deplete marrow iron stores, so ferrous sulphate 200 mg daily is given after starting the therapy.
- Maintenance dose of 500–1000 μg IM is given for every 3 months.
Folic acid defiiency:
- InitiallyFolicacid 5 mgdailyorallyfor4months isgiven.
- Maintenance dose is 5 mg folic acid once a week.
Iron Defiiency Anemia Underfollowing Headings
- Iron metabolism
- Investigations
- Treatment
Iron metabolism: Average diet consists of 10–15 mg of iron out of which 5–10% is normally absorbed.
Iron required for hemoglobin synthesis is derived from two primary sources, i.e. ingestion of food containing iron and recycling of iron from senescent red cells.
Iron is absorbed from duodenum and upper jejunum in ferrous form (Fe2+) and plays role in absorption.
Iron absorbs better from heme diet. Iron from heme is released in mucosa of small intestine after absorption for its utilization.
Iron is consumed from the diet and recycling of iron released is done by catabolism of hemoglobin derived from destroyed senescent red cells.
Transfer of iron to bone marrow is by ironbinding globulin, i.e. transferrin. Iron is stored in reticuloendothelial cells, hepatocytes and skeletal muscle cells as two iron protein complexes, i.e. ferritin which is water soluble and hemosiderin which is water insoluble. Iron is also present in myoglobin and cytochrome enzymes.
Total of 0.5–2 mg of iron is absorbed daily by normal human male or nonmenstruating female.
Out of which 0.5–1 mg of iron is lost in sweat, urine, stool and in mensis. 2 mg of iron is utilized in pregnancy. 0.5 mg is utilized in growth and lactation women.
Write short note on clinical features and diagnosis of acute myeloid leukemia.
Answer.
Clinical Features of acute Myeloid leukemia
- It occurs in adults and it age ranges from 15–40 years.
- It comprises of 20% of childhood leukemia.
- Symptoms due to anemia, i.e. tiredness, weakness and marked pallor.
- Hemorrhagic manifestations: Petechiae, bleeding from gums and nose, persistent bleeding after tooth extraction.
- Infection: It causes infective lesions of mouth and throat,i.e. ulceration of mouth and pharynx, herpes simplex
infection of face and infection of respiratory tract such as bronchitis and pneumonia. - Symptoms of cellular hyperviscosity
- There are tissue deposits of leukemic cells causing gum hypertrophy which is common in myelomonocytic and monocytic variety of AML.
- Lymphadenopathy and splenomegaly are present
- Signs of organ infitration are present, i.e.
Skin: Bluish nodules or dusky red patches are present.
Kidneys: Presence of kidney failure.
Other sites: Testes, ovary, liver, gut and serous membranes such as pleura and peritoneum. - Bone pain are present, i.e. tenderness of sternum, osteolytic bone lesions and pathologic fractures may occur.
- Constitutional symptoms, i.e. fever, malaise and prostration.
- Roth’s spot, i.e. presence of white central retinal hemorrhages in acute myeloid leukemia
Diagnosis of acute Myeloid leukemia
- Peripheral blood picture shows increase in number of typical or atypical myeloblasts. Auer rods may be found in cytoplasm.
- Bone marrow aspirate shows more than 30% blast cells. Marrow is entirely replaced by myeloblasts and promyelocytes.
- There is presence of low to high WBC count.
- Thrombocytopenia is moderate.
- Cytochemical stains: Myeloperoxidase and Sudan black are positive.
Define and classify anemia. Discuss clinical features, investigation and treatment of hemolytic anemia.
Answer.
It is defied as an acute disease marked by a defiit or absolute lack of granulocytic WBCs, i.e. neutrophils,basophils and eosinophils.
Clinical Manifestations
- Females are more commonly affcted than males
- Early manifestations of agranulocytosis are may be in form of sore throat or pain.
- There may be fever going up to 130°F, sometimes coming with rigor chills, body ache and pain and extreme degree of prostration.
- In large number of cases ulceromembranous lesions appear on throat, tonsils, gum, tongue and genitalia
- These are often covered with grayish black exudates and may become gangrenous.
- Lymph gland generally cervical groups and in some, there are generalized lymphadenopathy
- Liver and spleen may become enlarged.
- As disease progresses severe toxemia develops and patient may go into shock.
Hemolytic anemia is a reduction in number of circulating red cells from there premature destruction.
Etiological Classifiation
1. Acquired or E xtracorpuscular
1. Immunohemolytic anemia:
- Autoimmunohemolytic anemia
- Warm antibody autoimmune hemolytic anemia
- Cold antibody autoimmune hemolytic anemia
- Drug induced immunohemolytic anemia
- Iso immune hemolytic anemia.
2. Mechanical trauma: Microangiopathic hemolytic anemia
3. Direct toxic effct: Malaria, bacteria, infection and other agents
4. Acquired red cell membrane abnormalities: Paroxysmal nocturnal hemoglobinuria.
5. Splenomegaly.
2. Hereditary or Intracorpuscular
1. Abnormalities ofred cell membrane:
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Hereditary stomatocytosis.
2. Disorders ofred cell interior:
- Red cell enzyme defect:
- Defects in HMP shunt: G6PD defiiency
- Defects in glycolytic pathway: Pyruvate kinase defiiency.
3. Disorders ofhemoglobin:
- Structurally abnormal hemoglobin, sickle syndrome and other hemoglobinopathies.
- Reduced globin chain synthesis: Thalassemias.
Clinical Features
- There is presence of high fever, toxemia, marked*prostration, shock and hemoglobinuria
- Acute renal failure may develop
- Chronic form includes jaundice varying from mild to severe form, mongoloid faces, splenomegaly, chronic leg ulcers and pigment stones in gallbladder.
Write short answer on Megaloblastic Anemia.
Answer. Megaloblastic anaemias are characterized by macrocytic blood picture (MCV > 100 fl and megaloblastic bone marrow.
causes of megaloblastic anemia
1. Due to Vitamin B12 defiiency
1. Inadequate intake: In strict vegetarians, poor quality diet,in elderly
2. Impaired absorption
Gastric
- Pernicious anaemia
- Congenital intrinsic factor defiiency
- Gastrectomy
Small intestinal disease
- Bacterial overgrowth
- Crohn’s disease and resection of terminal ileum
- Tropical sprue and nontropical sprue
- Selective ileal malabsorption of B12 .
- Fish tapeworm disease
- Coeliac disease (folic defiiency more common)
Miscellaneous — HIV infection, severe pancreatic disease, drugs
3. Increased requirement: In pregnancy and disseminated cancer
2. Due to folic acid defiiency
- Inadequate intake: In malnutrition, Old age, Poverty,Alcoholism, Goat‘s milk, Kwashiorkor
- Impaired absorption: Coeliac disease, Dermatitis
herpetiformis, Tropical sprue, Congenital folate malabsorption and Oral contraceptives - Increased requirement: Infancy, pregnancy and hyperplastic marrow due to haemolytic anaemia
- Impaired utilization: Folic acid antagonists, methotrexate,pyrimethamine, trimethoprim, anticonvulsant drugs
- Increased loss (combined folic acid and vitamin B12 deficiency): Tropical sprue, Non—tropical sprue and haemodialysis
Megaloblastic Anemia Clinical Features
1. Due to anaemia: Shortness of breath, dyspnoea, pallor and in older subjects angina or cardiac failure.
2. Gastrointestinal: Diarrhoea, loss of appetite and weight.
Sore tongue due to glossitis and angular cheilosis. Mild jaundice may give the patient a lemon yellow tint.
3. Neurological
- Vitamin B12 neuropathy: Due to symmetrical damage to peripheral nerves and posterior and lateral columns of spinal cord, the legs being more affcted than arms.
Psychiatric abnormalities and visual disturbances may occur (from folate defiiency). - Neural tube defects: Folic acid supplements during pregnancy have been shown to reduce incidence of spina bifia, encephalocele and anencephaly in the foetus.
4. CVS disease — Raised serum homocysteine concentrations have been associated with arterial obstruction and venous thrombosis.
5. Gonadal dysfunction — Deficiency of either B12 or folic acid may cause sterility, which is reversible with appropriate vitamin supplements.
6. Knuckle pigmentation
Megaloblastic Anemia Laboratory diagnosis
1. Blood Film
1. Macrocytosis: Hemoglobin content in red cells is proportionately increased hence normal MCHC.
2. Peripheral smear: It shows
- Oval macrocytes
- Anisopoikilocytosis.
- Few tear drop cells and normocytes.
- Few nucleated RBCs.
- Macrocytes without central pallor.
- Evidence of dyserythropoiesis: basophilic stippling, Cabot ring and
3. HowellJolly bodies.
4. Haemoglobin is decreased.
5. Hypersegmented neutrophils may be the first evidence of megaloblastic anaemia.
6. Iron ferritin level increases.
2. Bone marrow
- Hypercellularity with marked erythroid hyperplasia.
- Megaloblasts are larger than normoblasts and have sieve like nuclear chromatin. Evidence of dyserythropoiesis.
- Myelopoiesis — Giant metamyelocytes and giant band forms with abnormal nuclear shapes.
- Megakaryocytes with hyperlobulation and immature nucleus.
- Dimorphic anaemia — Macrocytes and hypochromic microcytes in cases of combined B12/Folate and iron defiiency.
3. Biochemical estimations
- Serum folate levels: Decrease determined by isotope dilution method, microbiologic assay.
- Serum vitamin B12 levels — Decrease determined by isotope dilution technique or microbiological assay
- Increased levels of methylmalonic acid in serum and urine in B12 defiiency.
- FIGLU excretion in urine in excess in folic acid defiiency.
- Deoxyuridine suppression test for defiiency of both vitamin B12 and folate.
- Schillings test of vitamin B12 absorption. Radioactive vitamin B12 is used to assess intrinsic factor and
Vitamin B12 to distinguish megaloblastic anaemia due to intrinsic factor defiiency (pernicious anaemia) from other causes of B12 defiiency. - Serum homocysteine levels increased in folateand B12 defiiency.
Diagnosis Of Megaloblastic Anaemia
- Oval macrocytes in peripheral smear.
- Hypersegmented neutrophils.
- Megaloblastic erythropoiesis in bone marrow.
- Response to B12/Folate therapy.
Megaloblastic Anemia Treatment
1. Vitamin B12 defiiency
- Initially: Hydroxycobalamin 1000 µg IM, 6 injections in 2-3 weeks.
- Maintenance dose is 5001000 mcg IM every three months for life.
- For patients sensitive to B12 injections or those who refuse injections, oral B12 (cyanocobalamin) in large daily doses (100 µg or more).
2. Folate defiiency
- Initially folic acid 5 mg daily orally for at least 4 months. Folic acid in such big doses should not be given until B12 defiiency has been excluded, since folic acid may precipitate B12 neuropathy in a severely defiient B12 patient.
- Maintenance: Need depends on whether the underlying cause can be reversed, e.g. glutenfree diet in coeliac disease.
Mechanism of coagulation
Blood coagulation occurs in three major stages:
- Stage 1: Activation of StuartPrower factor (formation of prothrombin activator)
- Stage 2: Formation of thrombin from prothrombin
- Stage 3: Formation of firin from firinogen
Activation Of Stuart-Prower Factor (Factor X)
Activation of StuartPrower factor or factor X is the key to blood coagulation. Factor Xa is called prothrombin activator as it activates prothrombin to form thrombin. Therefore, this process is also called prothrombin activation.
This is achieved by two pathways: the intrinsic pathway and the extrinsic pathway.
Intrinsic Pathway
Intrinsic mechanism of prothrombin activation occurs in four steps:
step 1 (activation of factor XII)
Activation of intrinsic pathway starts with contact of Hageman factor with a negatively charged surface or exposed collagen of the injured vessel wall.
1. High molecular weight kininogen and kallikerin act as cofactors to facilitate the activation of factor XII
2. Exposed collagen stimulates platelet adhesion and aggregation before initiating blood coagulation.
step 2 (activation of factor XI)
Activated factor XII (XIIa) converts factor XI to its active form (XIa). This step is accelerated in the presence of high molecular
weight kininogen.
step 3 (activation of factor IX )
Factor XIa then converts factor IX to IXa, which is accentuated by factor VIIa. Calcium accelerates this process.
step 4 (activation of factor X)
Final step in activation of prothrombin activator is activation of factor X. Factor IXa causes activation of factor X to Xa, the activated Stuart prower factor. The membrane phospolipid, calcium and activated factor VIII act as cofactors for the activation of Stuart prower factor is crucial in Stage 1.
Formation of factor VIIIa is the key to the process of activation of factor X
Extrinsic Pathway
Extrinsic pathway of blood coagulation occurs in three steps:
step 1 (release of tissue thromboplastin)
Key to the clotting mechanism is the release of tissue thromboplastin from the injured tissue. As tissue thromboplastin is the tissue factor which is viewed as extrinsic to circulating blood, this system of blood coagulation is called extrinsic system of clottng.
step 2 (activation of vII)
Tissue thromboplastin converts factor VII to its active form (VIIa). This is the key step in extrinsic mechanism. Factor VIIa directly activates not only factor X, but also factor IX. Thus it also inflences intrinsic mechanism of activation of factor X.
step 3 (activation of X)
Factor VIIa converts X to Xa. This process is accelerated in the presence of calcium, platelet phospholipid and tissue thromboplastin.
Pathogenesis of hemophilia
- Haemophilia is caused by quantitative reduction of factor VIII in 90% of cases, while 10% cases have normal or increased level of factor VIII with reduced activity.
- Factor VIII is synthesized in hepatic parenchymal cells and regulates the activation of factor X in intrinsic coagulation pathway.
- Factor VIII circulates in blood complexed to another larger protein, von Willebrand’s factor (vWF), which comprises 99% of the factor VIII— vWF complex.
- Normal haemostasis requires 25% factor VIII activity.
Though occasional patients with 25% factor VIII level may develop bleeding, most symptomatic haemophilic patients have factor VIII levels below 5%.
Coagulation Clinical Features
- At birth: Newborn with hemophilia is usually healthy,though bleeding from cord and cephalohematoma may occur.
- In infant: Hemophilia is asymptomatic till 6 to 12 months,when bruising becomes more obvious. Bleeding from the mouth is common.
- During childhood: In severly affected individuals,spontaneous bleeding may occur in joint and muscles,including psosas muscle.
- In adults: Frequency of spontaneous bleeding decreases,but joints may already have been damaged. Intracranial hemorrhage is a lifethreatening complication. Spontaneous bleeds are common in mildly affcted individuals, but after injury bleeding occurs till appropriate therapy has begun.

Leave a Reply