Bleeding Disorders
Question 1. Write short note on hemophilia.
Or
Write briefly on hemophilia.
Or
Answer briefly on hemophilia.
Answer. It is a hereditary disorder of blood coagulation, characterized by excessive hemorrhage due to prolonged bleeding time.
It is the X-linked genetic disorder of coagulation.
Hemophilia Types
Following are the types of hemophilia, i.e.
- Hemophilia A or Classic Hemophilia: Deficiency of factor VIII or antihemophilic factor is the cause of hemophilia A. It is recessive X-linked.
Females are always carriers and males are sufferers. - Hemophilia B or Christmas Disease: A deficiency of factor IX is the cause of hemophilia B.
Read And Learn More: General Surgery Question And Answers
Hemophilia Clinical Features
- The most common manifestation is hemorrhage in the joint.
- Because of repeated hemorrhage knee joint becomes nonfunctional hemarthroses take place.
- Bleeding in muscles takes place.
- Bleeding from GIT occurs in the form of esophageal varices.
- Bleeding from the genitourinary tract occurs in the form of hematuria.
- A simple cut or injury may lead to profuse bleeding.
- The first symptom is seen in the form of large bruises and hematomas on the hips which regress as the child learns to walk.
Hemophilia laboratory diagnosis
Bleeding time is normal but coagulation time is prolonged.
Hemophilia Treatment
Hemophilia A
The main aim is to raise the factor VIII level, which can arrest bleeding.
- Replacement therapy: Varies from of replacement therapy are available like plasma, cryoprecipitate, and factor VIII
concentrates. - Give 30% amount of factor VIII, because it is very expensive.
- Any major operation or tooth extraction requires a 100% concentration of factor VIII.
- Hypovolemia, allergic reaction, and development of factor VIII antibodies are complications of factor VIII concentration.
To avoid this complication, cryoprecipitate from animal origin should be given in between human cryoprecipitate.
Hemophilia B
Fresh frozen plasma or Factor IX concentrates should be given to the patient.
Question 2. Describe different types of hemorrhage and management of hemorrhage.
Answer. Hemorrhage is the escape of blood from a blood vessel.
Types Of Hemorrhage
Depending upon the nature ofthe vessel involve:
Arterial hemorrhage:
- Bright red, jet out.
- Pulsation of the artery can be seen.
- It can be easily controlled as it is visible.
Venous hemorrhage:
- Dark red.
- It never gets out but oozes out.
- Difficult to control because the vein gets retracted, nonpulsatile.
Capillary hemorrhage:
- The red color, never jets out, slowly oozes out.
- It becomes significant, if there are bleeding tendencies.
Depending upon the timing of the hemorrhage:
- Primary hemorrhage: Occurs at the time of surgery.
- Reactionary hemorrhage: Occurs after 6 to 12 hours of surgery.
Hypertension in the postoperative period, and violent sneezing, coughing, or retching are the usual causes. - Secondary hemorrhage: Occurs after 5 to 7 days of surgery.
It is due to infection which eats away the suture material, causing sloughing of the vessel wall.
Depending upon the duration of the hemorrhage:
- Acute hemorrhage: Occurs suddenly, e.g. esophageal varices bleeding.
- Chronic hemorrhage: Occurs over some time, e.g. hemorrhoids/piles.
- Acute or chromic hemorrhage: It is more dangerous as bleeding occurs in individuals who are already hypoxic, which may get worsened faster.
Depending upon the nature of bleeding:
- External hemorrhage or reversal hemorrhage, e.g.epistaxis, haematemesis.
- Internal hemorrhage or concealed hemorrhage, e.g.splenic rupture following injury.
Based on the possible intervention
- Surgical hemorrhage: Can be corrected by surgical intervention
- Non-surgical hemorrhage: It is diffuse and oozes due to coagulation abnormalities and disseminated intravascular coagulation.
Management of Hemorrhage
Hemorrhage General management:
- Hospitalization
- Care of critically ill patients starts with A, B, and C (Airways, breathing, circulation).
- Oxygen should be administered.
- Intravenous line: Urgent intravenous administration of isotonic saline to restore the blood volume to normal.
- Colloids such as gelatins or hetastarch have also been used.
Hemorrhage Specific measures:
Hemorrhage Conservative
- By local pressure and packing:
- Pressure is applied with tight dressing, applying digital pressure, or cloth pegs for epistaxis.
Use of double-balloon in the esophagus and stomach to control the bleeding from esophageal varices. - Packing employing rolls of the wide gauge is an important stand-by in operative surgery.
Elevation of part: As in bleeding varicose ulcer.
- Rest: Absolute rest.
- Sedation: With diazepam.
- Treatment of shock: Treatment of hypovolemia by restoration of blood volume by blood transfusion and or saline, dextrose, etc.
Hemorrhage Operative:
- Clamping the bleeding vessels with catgut, thread, or silk.
- Coagulation by thermocautery or diathermy.
- By local application of adrenaline swabs.
- Application of silver clips as in neurosurgery.
- Under running or transfusion of vessels by needle and suture.
- Application of crushed piece of muscle at the site of bleeding.
- Bone wax or bismuth iodoform paraffin paste (BIPP) is used for oozing from bone.
- Repair of a vascular defect by patches of vein or Dacron mash.
- Excision of the bleeding organ: Splenectomy.
- Restoration of blood volume after hemorrhage
- Resuscitation from hemorrhage includes restoration of the circulating volume.
So Ringer lactate is preferred over the normal saline. Isotonic crystalloid or colloid solutions can be used for volume replacement in hemorrhage. - Blood transfusion: For restoring the circulating volume and replacing coagulation factors and oxygen-carrying capacity many blood products are available.
By crystalloid solution, hypovolemia is corrected.
Packed RBCs restore intravascular volume and oxygen-carrying capacity.
Platelet transfusions can be done for significant thrombocytopenia and continued hemorrhage
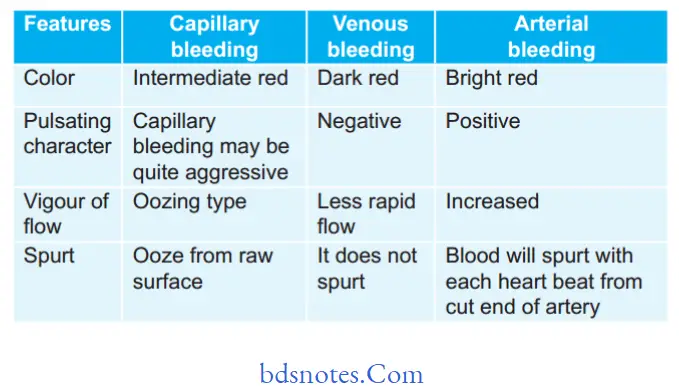
Question 3. Enumerate the difference between capillary, venous, and arterial bleeding.
Answer.
Question 4. Write a short note on a reactionary hemorrhage.
Answer.
Reactionaryhemorrhagemayfollowprimaryhemorrhage within 24 hours (usually 4–6 hours) and is mainly due to rolling (Slipping) of a ligature, dislodgment of a clot, or cessation of reflex vasospasm.
The precipitating circumstances are the rise of blood pressure and the shifting of the venous system on recovery from shock, and restlessness, coughing, and vomiting which raise the venous pressure, e.g. reactionary venous hemorrhage within a few hours of thyroidectomy.
Question 5. Give a brief account of bleeding disorders, their etiology, and management in dental practice.
Answer. Bleeding disorders: Bleeding disorders or hemorrhagic diatheses are a group of disorders characterized by defective hemostasis with abnormal bleeding.
Etiology Of Bleeding Disorders
Bleeding Disorders Vascular Defects:
Bleeding disorders caused by vascular defects may be caused by structural malformation of vessels.
Hereditary disorders of connective tissue and acquired connective tissue disorders.
Vascular defects rarely cause serious bleeding.
Bleeding into the skin or mucous membrane immediately alters trauma but ceases within 24 to 48 hours.
The vascular defects are hereditary hemorrhagic telangiectasia, Henoch-Schönlein purpura
Bleeding Disorders Platelet Disorder:
It can be of two types:
- Reduction in number: Thrombocytopenic purpura.
If the total number of circulating platelets falls below 50,000 per mm3 of blood the patient can have bleeding. In some cases the total platelet count is reduced by an unknown mechanism, this is called primary or idiopathic thrombocytopenic purpura (ITP).
Chemicals, radiation, and various systemic diseases, (e.g. leukemia) may have a direct effect on the bone marrow and may result in secondary thrombocytopenia. - Defect in quality: Non-thrombocytopenic purpura e.g. von Willebrand’s disease, Bernard-Soulier disease, Glanzmanns thrombasthenia.
Von-Willebrand’s disease (pseudo hemophilia) is the most common inherited bleeding disorder.
Unlike hemophilia, it can occur in females.
This is a disease of both coagulation factors and platelets.
It is caused by an inherited defect involving platelet adhesion.
Platelet adhesion is affected because of a deficiency of Von Willebrand`s factor.
Various drugs such as carbamazepine, aspirin, methyl dopa, and phenytoin can also lead to platelet disorders.
Bleeding Disorders Coagulation Defects
Hemophilia A: It is the most common coagulation defect.
It is inherited as an X-linked recessive trait.
The hemostatic abnormality in hemophilia A is caused by a deficiency/defect of factor VIII.
Until recently, factor VIII was thought to be produced by endothelial cells and not by the liver as most of coagulation factors.
The defective gene is located on the X chromosome.
Hemophilia B (Christmas disease): Factor IX is deficient or defective. It is inherited as an X-linked recessive trait. Like
Hemophilia A, the disease primarily affects males and the clinical manifestations of the two are identical.
Disseminated intravascular coagulation (DIC): It is a condition that results when the clotting system is activated in all or a major part of the vascular system.
Despite wide spread firin production, the major clinical problem is bleeding not thrombosis.
DIC is associated with many disorders such as infection, obstetric complications, cancer, and snake bites.
Management of Bleeding disorders
Hereditary Hemorrhagic telangiectasia
It is transmitted as an autosomal dominant trait and is characterized by bleeding from mucous membranes.
Bleeding Disorders Management
- In patients having repeated attacks of epistaxis septal dermoplasty should be done.
In septal dermoplasty, mucosa gets removed and skin grafting is done. - If spontaneous hemorrhages are present or nasal bleeding is present, it is controlled by giving pressure packs.
- Sclerosing agents i.e. sodium tetradecyl sulfate, were injected intralesionally to stop bleeding.
- Electrocautery is done. It helps in arresting bleeding.
Bleeding Disorders Idiopathic Thrombocytopenic Purpura (ItP)
Bleeding Disorders Steroid Treatment Protocol
Initial steroid treatment protocol for ITP: Initial steroid treatment protocol l mg/kg/day prednisolone, PO for 2–6 weeks.
subsequent steroid treatment protocol for ITP: Prednisolone dose is individualized for every patient.
Usually, the dose of prednisolone is tapered to less than l0 mg per day for 3 months and then withdrawn.
Splenectomy is done, if discontinuation of prednisolone causes a relapse.
Follow the ’rule of twos’ for major dental treatment and provide extra steroids before surgery, if the patient is currently on steroids or has used steroids for 2 weeks longer within the past 2 years.
Minor surgery
- Hemostasis after minor surgery is usually adequate if platelet levels are above 50,000 cells/mm3.
- Platelets can be replaced or supplemented by platelet transfusions; though sequestration of platelets occurs rapidly.
Platelet transfusion is indicated for established thrombocytopenic bleeding. - When given prophylactically platelets should be given half before surgery to control capillary bleeding and half at the end of the operation to facilitate the placement of adequate sutures.
- Platelets should be used within 6–24 hours after collection and suitable preparations include platelet-rich plasma (PRP), which contains about 90% of the platelets from a unit of fresh blood, and platelet-rich concentrate (PRC), which contains about 50% of the platelets from a unit of fresh whole blood.
- PRC is thus the best source of platelets. Platelet infusions carry the risk of isoimmunization, infection with bloodborne viruses, and, rarely, graft-versus-host disease.
- Where there is immune destruction of platelets (e.g. in ITP), platelet infusions are less effective.
- The need for platelet transfusions can be reduced by local hemostatic measures and the use of desmopressin or tranexamic acid or topical administration of platelet concentrates.
- Absorbable hemostatic agents such as oxidized regenerated cellulose (Surgicel), synthetic collagen (instant) or microcrystalline collagen (Avitene) may be put in the
socket to assist clotting in the post-extraction socket. - Drugs that affect platelet function, such as gentamicin, antihistamines, and aspirin should be avoided.
Major surgery
For major surgery, platelet levels over 75,000 cells/mm3 are desirable.
Bleeding Disorders Hemophilia
It is a hereditary disorder of blood coagulation characterized by excessive hemorrhage due to increased coagulation time. It is of two types, i.e. Hemophilia A and hemophilia B.
Bleeding Disorders Management
- Local anesthesia is contraindicated. So intrapulpal anesthesia, intraligamentary anesthesia should be used.
Sedation with diazepam or NO2–O2 sedation can be given. - Endodontic procedures should be carried out and care should be taken not to do instrumentation beyond apex.
If hemorrhage is present it should be controlled by 1:1000 aqueous epinephrine on paper point. - Restorative treatments can be carried out by proper application of rubber dam to avoid trauma to the gingiva and other soft tissues.
In case, if rubber dam is not present an epinephrine-impregnated hemostatic cord is kept in the gingival sulcus before the preparation of the crown or inlay margin. - Complete dentures and removable partial dentures can be given to hemophilic patients and are well tolerated by them.
The patient has to take care of proper maintenance of hygiene of the prosthesis. - Conservative periodontal treatment should be done rather than attempting periodontal surgeries.
- In case, if oral surgical procedures are to be done local
hemostatic agents should be used, pressure surgical packs should be employed, and sutures and topical thrombin should be used.
After removal of tooth socket is packed with a mechanical splint.
Postoperative use of anti-fibrinolytic agents is used
to support clot maintenance. - In cases of Hemophilia A, Human freeze-dried factor VIII concentrate or new recombinant factor VIII is used.
- In hemophilia B, human dried factor IX concentrate is supplied as a powder which is to be mixed with distilled water and administered IV
Bleeding Disorders Von Willebrand disease
- It is the most common inherited bleeding disorder.
It is inherited as autosomal dominant but a severe form of disease may be inherited as a sex-linked recessive trait. - It is caused due to a deficiency or defect in the Von Wille brand Factor.
- Types of Von-Willebrand diseases are Type I, Type II A and II B, and Type III.
Bleeding Disorders Management
- Surgical procedures can be performed in patients with mild Von Willebrand disease by using DDAVP and EACA.
Patients with severe Von Willebrand disease require cryoprecipitate and Factor VIII concentrate. - Bleeding should be controlled by using local measures such as pressure packs, gel foam with thrombin, tranexamic acid, etc.
- Aspirin and NSAIDs are avoided and acetaminophen can be given to patients.
- In majority of patients with Von Willebrand disease, the hemostatic defect is controlled with desmopressin via nasal spray.
- Type I Von Willebrand disease is treated with desmopres sin while Type II A and B, and Type III require clotting factor replacement.
Bleeding Disorders Disseminated Intravascular Coagulation
- Correction of hemodynamic instability by flid therapy, transfusion of packed cells, or whole blood.
- Factor replacement: This is the specific therapy, in this fresh frozen plasma, cryoprecipitate, and platelet concentrate transfusions are essential.
Fresh-frozen plasma is given at the dose of 15 mL/Kg. The platelet is transfused at the dosage of 0.1 unit/Kg.
Question 6. Write a short note on the treatment of hemangioma.
Answer. Hemangioma is a benign tumor containing hyperplastic endothelium with cellular proliferation with increased mast cells.
Treatment Of Capillary Hemangioma
- They are treated by wait and watch policy commonly allows for spontaneous regression.
- Diode laser, surgical excision, and reconstruction may need to be ligated after wide exposure before achieving complete extirpation.
Sclerotherapy/Cryotherapy/CO2 snow therapy causes unpleasant scarring. - Preoperative embolization facilitates surgical excision and reduces operative blood loss.
When once embolization is done surgery should be done as early as possible otherwise recurrence occurs and much more worry formation of enlarged collaterals can occur. - Rapidly growing hemangioma may need systemic/oral and intra-lesional steroid therapy.
- Anti-angiogenic interferon 2a may be useful.
- Life-threatening platelet trapping may be controlled by cyclophosphamide chemotherapy.
- Hemangioma with drug-resistant CCF can be treated with radiotherapy.
Treatment Of Cavernous Hemangioma
- Sclerosant therapy: It is the initial fist line therapy.
It causes aseptic thrombosis and fibrosis of the cavernous hemangioma with less vascularity and smaller size.
It is directly injected into the lesion. Sodium tetradecyl Sulphate hypertonic saline is used.
Often multiple injections are needed to achieve the complete required effect.
Later excision of the lesion is done. - Ligation of the feeding artery and often at a later stage excision is done once the hemangioma shrinks.
- Therapeutic embolization.
- lf small and located in an accessible area, excision is the initial therapy.
- LASER ablation: Diode-pulsed LASER is becoming popular because of good control of bleeding.
Question 7. Describe hemorrhage—its types, causes, clinical features, and management.
Or
Write a long answer on the cause of hemorrhage and its management.
Answer. Hemorrhage is the escape of blood from the blood vessel.
Hemorrhage Causes
- Hemorrhage occurs due to road accidents and injuries
- Gunshot wounds
- During surgeries such as thyroid surgery, circumcision, and hydrocele surgery.
- Due to erosion of the carotid artery by cancer.
- During inguinal block dissection.
- In bleeding disorders such as hemophilia.
Hemorrhage Clinical Features
- The patient becomes pallor and thirsty. At times, cyanosis is also present.
- There is the presence of tachycardia and tachypnea
- The patient feels air hunger.
- Skin is cold and clammy due to vasoconstriction.
- The patient has a dry face, dry mouth, and goose skin appearance.
- There is the presence of rapid thready pulse and hypotension
- Oliguria is present.
Hemorrhage Signs of Hemorrhage
- Pulse > 100/min
- Systolic blood pressure < 100 mm Hg
- Diastolic blood pressure drop on sitting or standing > 10 mm Hg
- Pallor/sweating
- Shock index, i.e. ratio of pulse rate to blood pressure >1
Question 8. Discuss briefly hemangioma.
Answer. Hemangioma is a benign tumor containing hyperplastic endothelium with cellular proliferation with increased mast cells.
Hemangioma Classification
Capillary hemangioma:
- Salmon patch
- Strawberry hemangioma
- Port-wine stain.
Cavernous hemangioma.
Hemangioma Clinical Features
- It is the most common tumor in children.
- It has biphasic growth showing initial rapid growth with gradual involution over 5 to 7 years.
- It is more common in girls.
- It is commonly seen in skin and subcutaneous tissue but can occur anywhere in the body like the liver, brain, lungs, and other organs.
- It grows rapidly in the first year and 70% is involved in 7 years.
- The early proliferative lesion is bright red and irregular; the deep lesion is bluish-colored. Involution causes color fading, softness, and shrinkage leaving a crepe paper-like area.
- Commonly it is central; common in the head and neck region.
- Often large hemangiomas may be associated with visceral anomalies. Head and neck hemangioma is associated with ocular and intracranial anomalies; sacral with spinal dysraphism.
- Multiple cutaneous hemangiomas may be associated with hemangioma of the liver causing hepatomegaly, cardiac failure (CCF), and anemia.
- Ulceration, bleeding, airway block, and visual disturbances are common complications.
- A definite even though rare, but important life-threatening complication is platelet trapping and severe thrombocytopenia presenting as ecchymosis, petechiae, intracranial hemorrhage, and massive gastrointestinal bleed.
Question 9. Define hemorrhage, its types, causes, investigations, and measures to control hemorrhage.
Answer. Hemorrhage is defined as the escape of blood from the cardiovascular system to the surface of the body or into the body tissues or cavities.
Hemorrhage Causes
- Trauma
- Infections
- Local irritants
- Congenital malformations
- Surgical (intraoperative/postoperative)
- Hemorrhage due to abnormalities in clotting factors:
Hemorrhage Clotting factor deficiencies
- Hereditary: Hemophilia A, Haemophilia B,
Thrombocytopenia. - Anticoagulant, antiplatelet, or fibrinolytic therapy:
- Warfarin, coumarin, heparin, enoxaparin, aspirin,clopidogrel etc.
- Liver disease.
Dysfunction of clotting—multiple myeloma:
Hemorrhage due to abnormalities in platelets
Hemorrhage Deficiencies:
- Idiopathic thrombocytopaenia purpura
- Secondary thrombocytopaenia purpura
- Leukemia.
Thrombocytosis
Dysfunction: Thrombocytopenia.
Hemorrhage due to systemic disease
- Viral infection
- Scurvy
- Allergy.
Investigations
Patients with the above-mentioned causes may be advised to be subjected to an investigation before any oral surgical procedure.
Hemorrhage Investigations are:
- Clotting time
- Bleeding time
- Prothrombin time and International normalized ratio
- Activated partial thromboplastin time
- Factors assay.
Hemorrhage Investigations For Measuring Blood Loss
- Hb% and PCV estimation
- Blood volume estimation using the radioiodine technique or microhematocrit method
- Measurement of CVP or PCWP
- Investigations specific for cause, i.e. ultrasonography of abdomen, Doppler and often angiogram in vascular injury, Chest X-ray in hemothorax, CT scan in major injuries, CT scan head in head injuries.
Hemorrhage Measures to Control Hemorrhage
Hemorrhage Mechanical Methods
- Pressure: Firm pressure is applied over the bleeding site for 5 minutes.
- Hemostat: It is applied at bleeding points and leads to direct occlusion of the bleeding vessel
- Sutures and ligation: For severed blood vessels ligature is done. For large pulsating arteries, suturing is done.
Hemorrhage Chemical Methods
- Adrenaline: It leads to vasoconstriction of bleeding capillaries
- Thrombin: Converts fibrinogen into fibrous clot
- Surgicel: Acts by forming acid products from partial dissolution which coagulate plasma protein
- Surgical fibrillar: It is modified surgical and is used on irregular surfaces and inaccessible areas
- Oxycel: Platelet plugs in its meshwork and forms the clot
- Gelatine sponge Or Gelfoam/surgical
- Microfirillar collagen (Avitene)
- Fibrous glue
- Styptics and astringents: They precipitate protein and arrest bleeding
- Alginic acid
- Natural collagen sponge: It activates coagulation factors
XI and XIII and help in clotting - Fibrin sponge: It stimulates coagulation forming normal clots and also acts as a temporary plug over small injured blood vessels
- Bone wax: It is used in cases of bleeding from bone or chipped edges of bone. It is softened with fingers and applied to the bleeding site
- Ostene: a new water-soluble bone hemostatic agent.
Hemorrhage Thermal Agents
- Electrocautery/surgical diathermy: Small capillaries and bleeding vessels are coagulated by diathermy.
- Monopolar diathermy
- Bipolar diathermy
- Cryosurgery
- Lasers: Coagulate small blood vessels.
Question 10. Write a short note on hemophilia—its types and management.
Answer. Types of Hemophilia

Question 11. Define and describe the differentiating features of the cirsoid aneurysm and strawberry hemangioma.
Answer.

Question 12. Enumerate differences between primary, reactionary, and secondary hemorrhage.
Answer.

Question 13. Write a short note on capillary hemangioma.
Answer. Capillary hemangioma is of three types i.e.
- Salmon patch
- Strawberry hemangioma
- Port-wine stain.
Capillary Hemangioma Salmon Patch
- It is present at the time of birth.
- It commonly occurs at the nape of the neck, face, scalp, and limbs.
- The lesion involves a wide area of skin.
- It is caused due to the area of persistent fetal dermal circulation.
- It regresses with age and disappears completely.
Capillary Hemangioma Strawberry Hemangioma
- The child is normal at birth, but between 1 to 3 weeks lesions appear as red marks which increase in size to 3 months.
- This is a true capillary hemangioma.
- The lesion is 20 times more common than port-wine stain.
- The lesion is seen more commonly in white girls
- Its male-to-female ratio is 1:3.
- The lesion occurs most commonly in the head and neck region.
- On palpation, the lesion is compressible and warm with a bluish surface.
- The lesion involves skin, muscles, and subcutaneous tissues.
- The lesion begins to disappear one year of age and it completely regresses in 7 to 8 years.
Capillary Hemangioma Port-wine Stain
- It occurs at birth and persists throughout the life.
- It presents as smooth, flat, reddish blue or purplish.
- The lesion is common in the head, neck, and face.
- Eventually surface of the lesion becomes nodular and keratotic.
- It results from a defect in the maturation of sympathetic innervations of skin causing localized vasodilatation of intradermal capillaries.
- It requires cosmetic coverage. Excision, grafting, or LASER ablation.
Capillary Hemangioma Treatment Of Capillary Hemangioma
- They are treated by wait and watch policy commonly allows for spontaneous regression.
- Diode laser, surgical excision, and reconstruction may need to be ligated after wide exposure before achieving complete extirpation.
Sclerotherapy/Cryotherapy/CO2 snow therapy causes unpleasant scarring. - Preoperative embolization facilitates surgical excision and reduces operative blood loss. When once embolization
done surgery should be done as early as possible otherwise recurrence occurs and much more worry formation of enlarged collaterals can occur. - Rapidly growing hemangioma may need systemic/oral and intralesional steroid therapy.
Antiangiogenic interferon 2a may be useful. - Life-threatening platelet trapping may be controlled by cyclophosphamide chemotherapy.
- Hemangioma with drug-resistant CCF can be treated with radiotherapy.
Question.14. Write a short note on coagulation.
Answer. It is the spontaneous arrest of the bleeding.
Following are the factors which are involved in the mechanism of coagulation of blood:
- Factor I—Fibrinogen
- Factor II—Prothrombin
- Factor III—Thromboplastin (Tissue factor)
- Factor IV—Calcium ions
- Factor V—Labile factor
- Factor VI—Presence not approved
- Factor VII—Stable factor
- Factor VIII—Anti-hemophilic factor
- Factor IX—Christmas factor
- Factor X—Stuart-Prower factor
- Factor XI—Plasma thromboplastin antecedent
- Factor XII—Hageman factor
- Factor XIII—Fibrin-stabilizing factor
- Factor XIV—Prekallikrein
- Factor XV—Kallikrein
- Factor XVI—Platelet factor.
Coagulation Clotting occurs in three Stages
1. Formation of prothrombin activator.
2. Conversion of prothrombin into thrombin.
3. Conversion of firinogen to firin.
Formation of prothrombin activator: The prothrombin activator is formed in two ways:
Coagulation Extrinsic pathway
- Factor III initiates this pathway after injury to damage tissues.
After the injury, these tissues release thromboplastin which contains protein, phospholipid, and glycoprotein which act as proteolytic enzymes. - The glycoprotein and phospholipid component of thromboplastin converts factor X into activated factor X, in the presence of factor VIII.
- Activated factor X reacts with factor V and phospholipid content of tissue thromboplastin to form a prothrombin activator in the presence of calcium.
- Factor V is activated by thrombin formed from prothrombin. This factor V now accelerates the formation of the prothrombin activator.

Coagulation Intrinsic pathway: It occurs in the following sequence:
- During injury, the blood vessel is ruptured, the endothelium is damaged and collagen beneath the endothelium is exposed.
- When factor XII comes in contact with collagen, it is converted to active factor XII.
- The active factor XII converts inactive factor XI to active factor XI in the presence of kininogen.
- The activated factor XI activates factor IX in the presence of calcium ions.
- Activated factor IX activates factor X in the presence of factor VIII and calcium.
- When platelet comes in contact with the collagen of the damaged blood vessels, it releases phospholipids.
- Now, active factor X reacts with platelet phospholipid and factor V to form prothrombin activation in the presence of calcium ions.
- Factor V is activated by the positive feedback method.
Coagulation Conversion of prothrombin into thrombin: The Prothrombin activator converts prothrombin into thrombin in the presence of calcium by a positive feedback mechanism.
This accelerates the formation of extrinsic and intrinsic prothrombin activators.
Coagulation Conversion of fibrinogen to fibrin: During this, the soluble fibrinogen is converted to fibrin by thrombin.
The fibrinogen is converted to activated fibrinogen due to the loss of two pairs of polypeptides.
The first form of firing contains loosely arranged strands which are modified later into tight aggregate by factor XIII in the presence of calcium ions.
Question 15. Classify hemorrhages. Management of hypovolemic shock. Complications of blood transfusion.
Answer.
Classification of Hemorrhage
Depending upon the nature of the vessel involved:
Arterial hemorrhage:
- Bright red, jet out.
- Pulsation of the artery can be seen.
- It can be easily controlled as it is visible.
Venous hemorrhage:
- Dark red.
- It never gets out but oozes out.
- Difficult to control because the vein gets
retracted, nonpulsatile.
Capillary hemorrhage:
- The red color, never jets out, slowly oozes out.
- It becomes significant if there are bleeding tendencies.
Depending upon the timing of the hemorrhage:
- Primary hemorrhage: Occurs at the time of surgery.
- Reactionary hemorrhage: Occurs after 6 to 12 hours of surgery. Hypertension in postoperative period, violent sneezing, coughing, or retching are the usual causes.
- Secondary hemorrhage: Occurs after 5 to 7 days of surgery. It is due to infection which eats away the suture material, causing sloughing of the vessel wall.
Depending upon the duration of the hemorrhage:
- Acute hemorrhage: Occurs suddenly, e.g. esophageal varices bleeding.
- Chronic hemorrhage: Occurs over some time, e.g. hemorrhoids/ piles.
Depending upon the nature of bleeding:
- External hemorrhage or reversal hemorrhage,e.g. epistaxis, haematemesis.
- Internal hemorrhage or concealed hemorrhage,e.g. splenic rupture following injury.
Based on the possible intervention
- Surgical hemorrhage: Can be corrected by surgical intervention
- Non-surgical hemorrhage: It is diffused and oozes due to coagulation abnormalities and disseminated intravascular coagulation.
Complications of Blood transfusion
The following are the complications of blood transfusion:
- Febrile reactions: It is the most common complication due to impurities like pyrogens in the blood or the infusion set.
- Headaches, fever, chills, rigors, tachycardia, and nausea are the features.
- Transfusion is temporarily stopped or the flow is slowed down with the administration of the antipyretic drug to reduce fever.
- Often transfusion of that unit needs to be discontinued.
- Allergic reaction: Urticaria and allergy to specific proteins in the donor’s plasma can occur.
- Usually, it is mild and is treated with steroids and antihistaminics.
- In severe urticaria that unit of blood is discarded; new washed RBCs and platelets are used.
- Acute hemolytic reactions: It is the most dangerous complication. It is due to ABO incompatibility.
- Usually, it is nonfatal but occasionally can be fatal.
- It is commonly due to technical errors at different levels. It amounts to criminal negligence in a court of law.
- Transfusion-related graft versus host disease: This very serious, very rare complication occurs due to recognition and reaction against host tissues by infused donor lymphocytes. lt is common in immunosuppressed, lymphoma, and leukemic patients.
- Any type of blood product including leukocyte-reduced blood can cause the condition.
- Features are pancytopenia, toxic epidermal necrosis, and liver dysfunction with more than 90% mortality. It is difficult to treat.
- Congestive cardiac failure: It occurs if especially large quantities of whole blood are transfused in chronic severe anemia, pregnancy, elderly patients, in patients who have cardiac problems.
Question 16. Write briefly on the Rhesus (Rh) blood group.
Answer. The Rhesus blood group was discovered by Landsteiner and Weiner in 1940.
- Rh antigen system has three closely linked gene loci, coding for D antigen (there is no d antigen), C and/or c antigen, and E and/or e antigen. Thus, the antigens produced are C. D, E. c and e.
- An individual may have similar or different sets of these three Rh antigens on each chromosome; for example, CDE/cde, cde/cde, or CdE/cdE (each person inherits one trio gene from each parent).
- Individuals who are positive for D antigen are considered Rh—positive (85% of the population) and those who lack it are Rh—negative.
- Individuals with a weak variant of D antigen called the Du variant, are also considered Rh—positive.
- Alloimmunization, i.e. formation of an antibody against an antigen occurs if a person is exposed to an Rh antigen that is not on the patient’s RBCs.
- The majority of clinically important antibodies that produce a transfusion reaction are warm-reacting (IgG) antibodies (eg, anti-D, anti-Kell) rather than cold-reacting (IgM) antibodies.
Rh incompatibility or erythroblastosis fetalis or hemolytic disease of newborn: When a mother is Rh negative and the fetus is Rh positive the fist child does not undergo Rh incompatibility.
This is because Rh antigen cannot pass from fetal blood into the mother’s blood due to the placental barrier but during the delivery of a child Rh antigen from fetal blood may leak into the mother’s blood due to placental detachment and the mother develops Rh antibody in her blood.
When the mother conceives for the second time and if the fetus is Rh positive the Rh antibody crosses the mother’s placental barrier and enters fetal blood and causes fetal agglutination of fetal RBCs which leads to hemolysis.
Due to excessive hemolysis children suffer from severe anemia, hydrops fetalis, and kernicterus.
Rhesus (Rh) blood group Treatment
Exchange blood transfusion should be done soon after birth,i.e. small quantities of infant’s blood successively from intra venous catheter and replacing an equal volume of compatible Rh-negative blood. So the infants ‘ positive RBCs prone to destruction are removed from circulation.
Rhesus (Rh) blood group Prevention
Destruction of Rh-positive fetal cells in maternal blood is brought about by administering a single dosage of anti-Rh antibody in the form of Rh immunoglobulin soon after the birth of a child.
This prevents active antibody formation by the mother.
Question 17. Describe the differentiating features of primary and reactionary hemorrhage.
Answer.
The differentiating features of primary and reactionary hemorrhage.


Leave a Reply