Benign And Malignant Tumors Of Oral Cavity
Question.1. Enumerate white lesions of orofacial region. Describe etiology, histopathology and clinical features of leukoplakia.
Or
Enumerate white lesions of oral cavity. Describe leukoplakia in detail.
Answer. The white lesions of oral cavity/orofacial region are as follows:
- Hereditary condition:
- Leukoedema
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- Keratosis follicularis
- Ptylosis syndrome.
- Leukoplakia and malignancies:
- Chronic cheek biting
- Friction or trauma-associated leukoplakia
- Tobacco associated leukoplakia
- Carcinoma in situ
- Squamous cell carcinoma
- Verrucous carcinoma.
Read And Learn More: Oral Pathology Question And Answers
- Dermatosis:
- Lichen planus
- Lupus erythematous.
- Inflammation:
- Mucous patches of syphilis
- Candidiasis
- Koplik spots of measles.
- Miscellaneous conditions:
- Oral submucous firosis
- Papilloma
- Lipoma
- Hairy tongue
- Geographic tongue
- Fordyce’s granules.
Leukoplakia is defied as “a white patch or plaque that cannot be characterized, clinically or pathologically as any other disease and is not associated with any other physical or chemical causative agent except the use of tobacco”.
Axell et al, 1984 Leukoplakia is defied as a predominantly white lesion of the oral mucosa that cannot be characterized as any other defiable lesion. WHO (1997)
Leukoplakia should be used to recognize white plaques of questionable risk having excluded (other ) known diseases or disorders that carry no increased risk for cancer.
Warnakulasuriya et al (2008).
Etiology Of Leukoplakia
The common predisposing factors of leukoplakia are:
- Tobacco: It is used by large number of people in various forms such as smoking of cigarett, cigar, biddies and pipes.
All these types of tobacco habits are important for development of leukoplakia.
It is believed that during smoking a large amount of tobacco end products are produced in oral cavity.
The products in association with heat cause severe irritation to oral mucus membrane and finally result in development of leukoplakia. - Alcohol: Alcohol leads to the entry of carcinogen into exposed cells and thus alters oral epithelium as well as its metabolism.
- Candidiasis: Chronic candidal infections are associated with leukoplakia.
- Dietary deficiency: Deficiency of vitamin A causes metaplasia and hyperkeratinization of epithelium which may result in development of leukoplakia.
- Syphilis: Syphilitic infections play minor role in causation of leukoplakia.
- Hormonal imbalance: Imbalance or dysfunction of both male and female sex hormones causes keratogenic changes in oral epithelium. These changes lead to the development of leukoplakia.
Modifid Classifiation of Leukoplakia
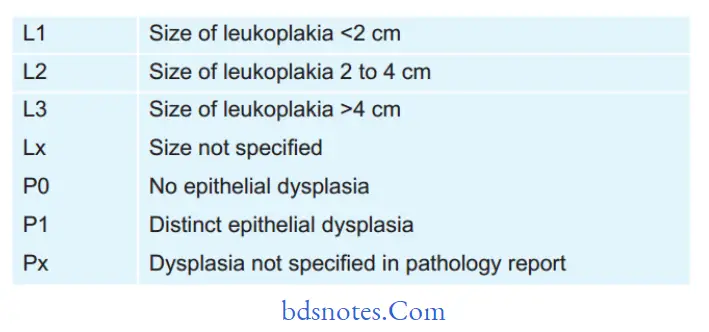
Oral Leukoplakia Staging System
Stage 1 L1P0
Stage 2 L2P0
Stage 3 L3P0 Or L1L2P1
Stage 4 L3P1
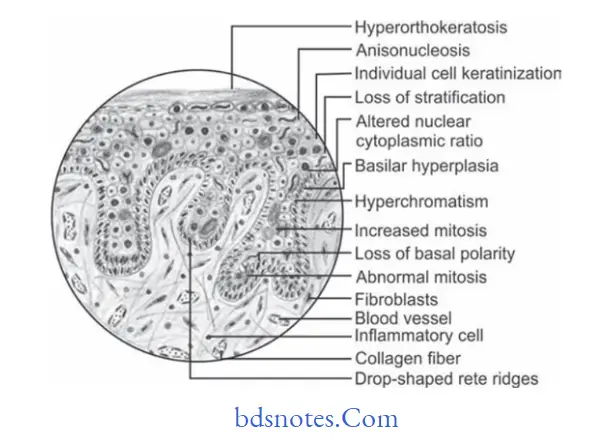
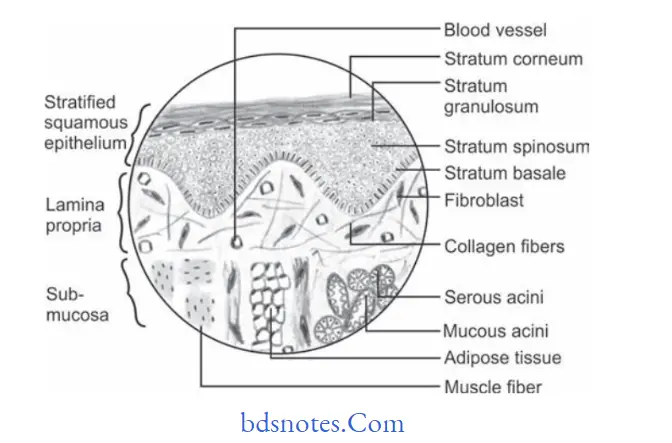
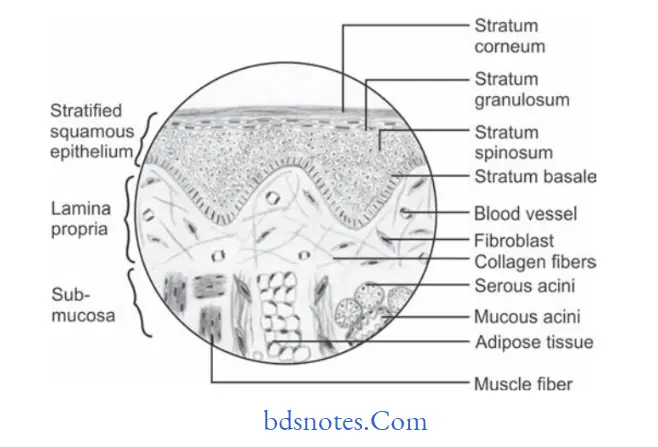
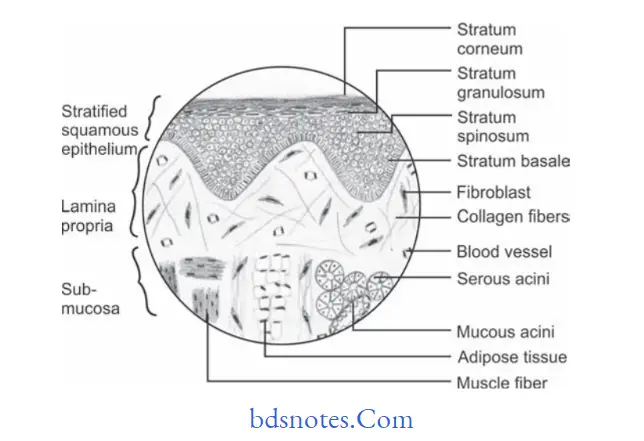
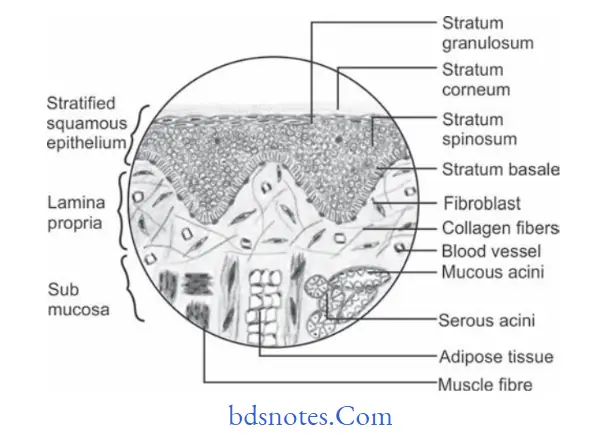
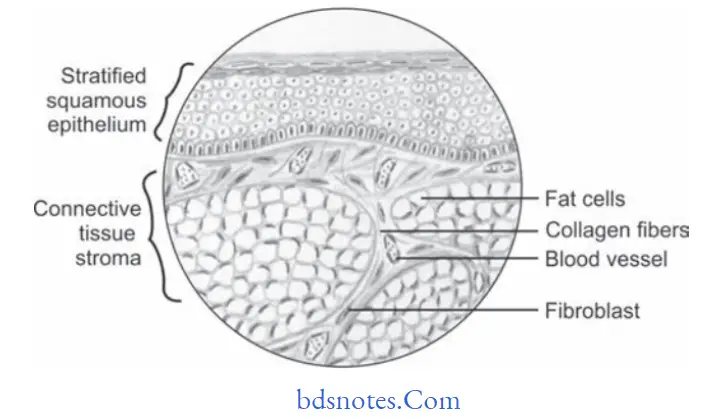
Histopathology
During leukoplakia variety of histologic changes are present which are related to:
- Keratinization pattern
- Changes in cellular layer
- Thickness of epithelium
- Alteration in underlying connective tissue stroma.
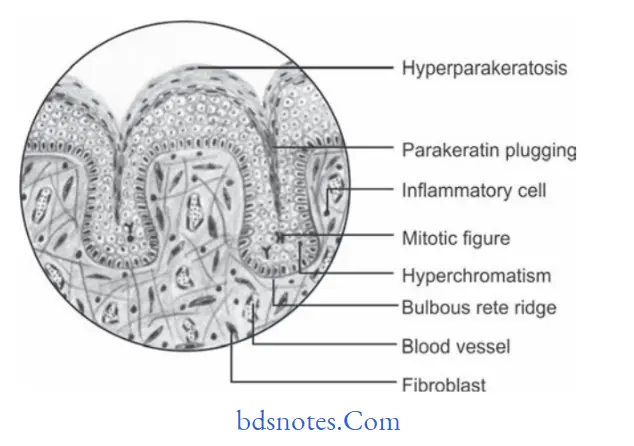
Keratinization pattern
- Leukoplakia generally presents hyperorthokeratinization or hyperparakeratinization or both with or without the presence of epithelial dysplasia.
- In case of leukoplakia an abnormal increase in the thickness of orthokeratin layer is seen in area of epithelium which is usually keratinized.
- An important histological criterion of leukoplakia is presence of hyperkeratinization of normally keratinized epithelium or some amount of parakeratin deposition in area of epithelium which are usually not keratinized.
- Epithelium dysplasia is more frequently associated with hyperkeratinized lesion.
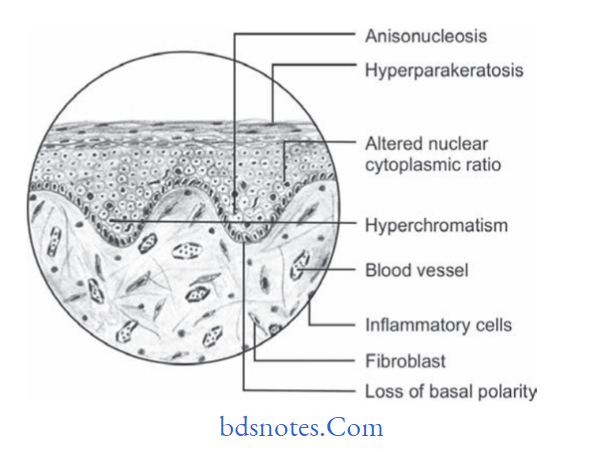
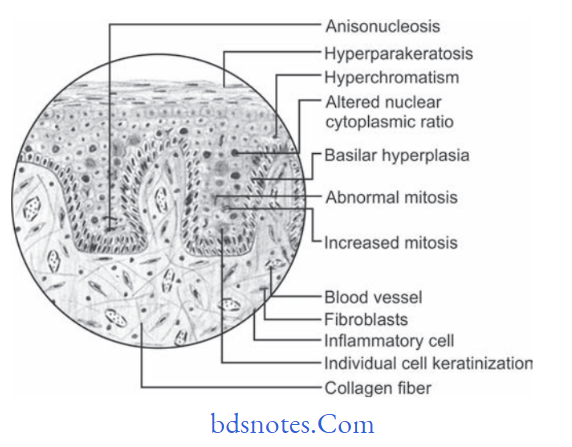
Changes in Cellular layer
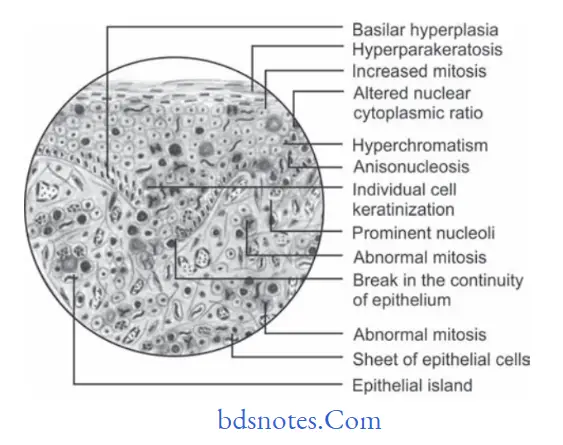
Epithelial dysplasia is the hallmark of histologic changes seen in epithelium in case of leukoplakia. The criteria for epithelial dysplasia are:
Architecture and Cytologic Criteria for Grading Epithelial Dysplasia Given by WHO (2005)
Architecture Criteria
- Irregular epithelial stratifiation
- Loss of polarity of basal cells
- Basal cell hyperplasia
- Drop shaped rete pegs
- Increased number of mitotic fiures
- Abnormally superfiial mitosis
- Dyskeratosis i.e. premature keratinization in the cell
- Keratin pearls within rete ridges
Cytologic Criteria
- Anisonucleosis: Abnormal variation in nuclear size
- Nuclear pleomorphism: Abnormal variation in nuclear shape
- Anisocytosis: Abnormal variation in cell size
- Cellular pleomorphism: Abnormal variation in cell shape
- Increased nuclear cytoplasmic ratio
- Increased nuclear size
- Atypical mitotic fiures
- Increase in the number and size of nucleoli
- Hyperchromatism
Histopathology
- Classification of epithelial dysplasia is done on basis of its severity which is:
- Mild epithelial dysplasia: It refers to the alteration which is limited to basal and parabasal cell layers.
- Moderate epithelial dysplasia: It shows involvement from basal layer to mid portion of spinous cell layer.
- Severe epithelial dysplasia: It shows alterations from basal layer to the level above mid portion of epithelium.
- When complete thickness of epithelium, term carcinoma in situ is used.
- Histopathological report of leukoplakia should include a statement on absence or presence of epithelial dysplasia.
Thickness Of The Epithelium
In leukoplakia, the thickness of epithelium is altered and it occurs in epithelial atrophy or acanthosis.
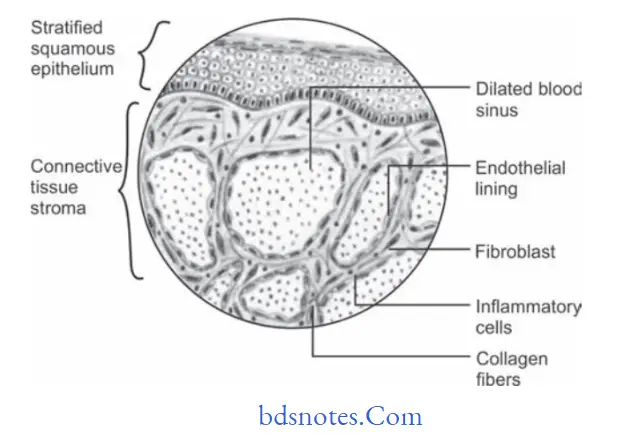
Alteration In Underlying Connective Tissue
In leukoplakia there is often variable degree of destruction of collagen fiers and moreover chronic inflammatory cell infitrate is also present in underlying connective tissue stroma.
Clinical Features
- Usually the lesion occurs in 4th, 5th, 6th and 7th decades of life.
- Buccal mucosa and commissural areas are most frequent affcted sites followed by alveolar ridge, tongue, hard and soft palate, etc.
- Oral leukoplakia often present solitary or multiple white patches.
- Size of lesion may vary from small well localized patch measuring few millimeters in diameter.
- The surface of lesion may be smooth or fiely wrinkled or even rough on palpation and lesion cannot be removed by scrapping.
- Lesion is whitish or greyish or in some cases it is brownish yellow in color due to heavy use of tobacco.
- In most of the cases these lesion are asymptomatic, however in some cases they may cause pain, feeling of thickness and burning sensation, etc.
Question.2.Define the premalignant lesions and conditions. Describe etiology, histopathology, and clinical features of leukoplakia.
Or
Define and enumerate precancerous lesions. Describe in detail leukoplakia.
Or
Define and enumerate precancerous lesions and conditions. Write in detail about histopathological features of leukoplakia.
Or
Define precancerous lesions and conditions of oral cavity with examples. Describe leukoplakia in detail.
Answer. Premalignant Lesions or Precancerous Lesions
Premalignant lesions are defied as ”A morphologically altered tissue in which cancer is more likely to occur then in its apparently normal counter part”.
The examples are:
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Actinic cheilitis, actinic keratosis and actinic elastosis
- Bowen’s disease
- Carcinoma in situ
Premalignant Condition or precancerous Condition
The premalignant condition is defied as “A generalized state of body, which is associated with signifiantly increased risk of cancer development”.
The examples are:
- Oral submucus firosis
- Syphilis
- Lichen planus
- Sideropenic dysphagia
- Lupus erythematosus
- Dyskeratosis congenita
- Xeroderma pigmentosum
- Epidermolysis bullosa.
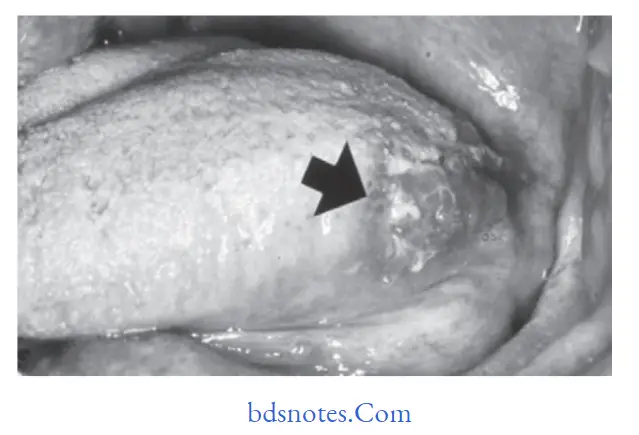
Question.3. Write notes on hairy leukoplakia.
Answer. Hairy leukoplakia is HIV associated mucosal disorder,which often involves lateral and ventral surfaces of tongue.
Homosexual man with HIV infection may develop white patchy lesion in oral cavity.
Clinical Features
- Clinically hairy leukoplakia occurs more frequently on the lateral border of the tongue however it can also occur on flor of the mouth, buccal mucosa, etc.
- The lesion often appears as white patch and is characterized by an irregular surface, exhibiting numerous linear vertical folds or projections, sometimes so marked to as resemble “Hairs”.
- The lesions are always colonized by Candida albicans.
Hairy leukoplakia probably occurs as an opportunistic infection caused by EpsteinBarr virus. - Hairy leukoplakias are asymptomatic lesions and whenever they occur they occur on buccal mucosa, the lesions are smooth and homogeneous with straitened margin.
Histopathology
- A very characteristic fiding in hairy leukoplakia is presence of subcorneal upper spinous layer zone made up of cytopathologically altered keratinocytes.
- Parakeratin layer is thick often colonized by candidal hyphae.
- The submucosa does not exhibit many inflammatory cell infitrate.
Differential Diagnosis
- Lichen planus
- Verrucous leukoplakia
- Chronic tongue biting habits.

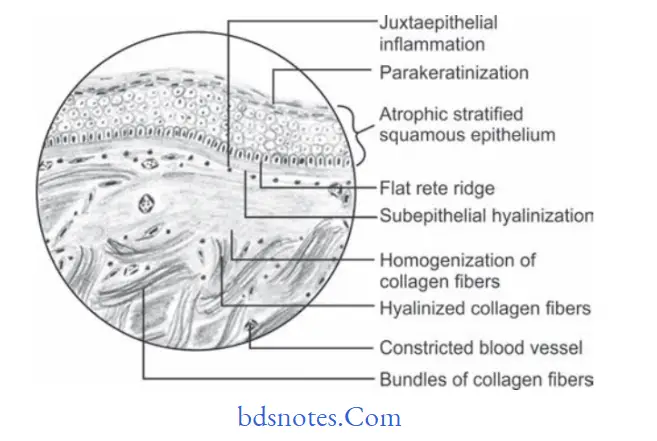
Question.4.Write notes on oral submucus firosis.
Answer. OSMF is defined as “An insidious chronic disease affcting any part of oral cavity and sometime pharynx.
Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxtaepithelial inflammatory reaction followed by firoelastic changes in lamina propria, with epithelial atrophy leading to stiffess of oral mucosa and causing trismus and inability to eat.” Pindborg (1966)
Etiology
- The OSMF is caused due to:
- Excessive consumption of red chillies.
- Excessive “areca nut” chewing.
- Nutritive deficiency
- Immunological factors
- Genetic factors
- Protracted tobacco use
- Patient with deficiency of micronutrients.
- Use of lime with areca nut
Clinical Features
- It is caused during 20 to 40 years of age.
- Females are affcted more than males.
- In OSMF firotic changes are frequently seen in buccal mucosa, retromolar area, uvula, tongue, etc.
- Initially patient complains of burning sensation in the mouth, particularly during taking hot and spicy foods.
- There can be excessive salivation, decreased salivation and defective gustatory sensation.
- In initial phase of disease palpation of mucosa elicits a “wet leathery” feeling.
- In advanced stage the oral mucosa loses its resilience and becomes blanched and stif and thereby causing trismus.
- Palpation of mucosa often reveals vertical firous bands.
Histopathology
Microscopically OSMF reveals following features:
- Overlying hyper keratinized, atrophic epithelium often shows flattening and shortening of rete pegs.
- There can be variable degrees of cellular atypia or epithelial dysplasia.
- In OSMF dysplastic changes are found in epithelium which include nuclear pleomorphism, sever intercellular edema, etc.
- Stromal blood vessels are dilated and congested and there can be areas of hemorrhage.
- Underlying connective tissue stroma in advanced stage of disease shows homogenization and hyalinization of collagen fiers.
- Decreased number of firoblastic cells and narrowing of blood vessels due to perivascular firosis are present.
- There can be presence of signet cells in some cases.
Treatment
- Stoppage of all causing habits.
- Definitive treatment of OSMF includes intralesional injection of collagenase, corticosteroids and firinolysin, etc.
- Systemic administration of steroids in severe cases.
Question.5. Describe in brief histopathology of intraepithelial carcinoma.
Answer. This is also called as carcinoma in situ
- Intraepithelial carcinoma is a condition which arises frequently on skin, but occurs also on mucus membrane including those of oral cavity.
- Metastasis is impossible in intra epithelial carcinoma.
- Bowen’s disease is a special form of intraepithelial carcinoma occurring with some frequency on skin, particularly in patients who have had arsenic
therapy and is often associated with development of internal or extra cutaneous cancer.
Histological Features
- Keratin may or may not be found on the surface of lesion but, if present, is more apt to be parakeratin rather than orthokeratin.
- In some instances, there appears to be hyperplasia of the altered epithelium while in others there is atrophy.
- An increased nuclear/cytoplasmic ratio and nuclear hyperchromatism is seen.
- Cellular pleomorphism is common
- There is loss of orientation of cells and loss of their normal polarity.
- Sometimes a sharp line of division between normal or altered epithelium extends from surface down to the connective tissue rather then a blending of epithelial changes.
Treatment
- Treatment is done by surgery, radiotherapy or electrocautery
Question.6. Describe etiology, histopathology and clinical features of carcinoma of tongue.
Or
Describe in detail the etiology, clinical features and histopathology of squamous cell carcinoma of tongue.
Answer.
Etiology
- Syphilis either an active case or past history of it coexistent with carcinoma of tongue. Syphilis is accepted as having strong association with development of dorsal tongue carcinoma. Arsenicals and heavy metals used to treat syphilis before advent of modern antibiotics have carcinogenic properties themselves and are responsible for some of earlier carcinoma development
in this disease. - Leukoplakia is the common lesion of tongue which leads to carcinoma of tongue.
- Carcinoma of tongue is due to poor oral hygiene, chronic trauma and use of alcohol and tobacco.
- Carcinoma of tongue is due to source of chronic irritation such as carious or broken tooth or an ill fitting denture.
Histopathology
- Cells are generally large and show distinct cell membrane.
- Nuclei of neoplastic cells are large.
- Carcinomas of tongue ranges from well diffrentiated keratinizing carcinoma to highly diffrentiated neoplasm.
- Changes of epithelial dysplasia are present.
- There is increased number of mitotic fiure per fild.
Clinical Features
- Most common presenting signs of carcinoma of tongue is painless mass or ulcer. The lesion becomes painful when it is secondarily affcted.
- Tumor begins as superfiially indurated ulcer with slightly raised borders and may proceed either to develop a fungating, exophytic mass or to infitrate deep layers of tongue,producing fiation and induration without much surface change.
- If carcinoma is present on the dorsum of tongue,then patient has past or present history of syphilitic glossitis.
- Paresthesia of tongue frequently occurs due to invasion of lingual nerve by tumor cells.
- The common site where the lesion develops is lateral border of tongue and ventral surface of tongue.
- Initial lesions often appear as erythematous macules or nodules or fisured areas over the tongue.
Question.7. Write short note on peripheral giant cell granuloma.
Or
Describe histologic features with diagram of peripheral giant cell granuloma.
Answer. Peripheral giant cell granuloma is the most common of giant cell lesions which arises from tooth bearing areas of jaw and appears as a purplish red nodule.
Clinical Features
- Lesion usually arises during mixed dentition or during third and fourth decade of life.
- It is most common in males.
- Its site in dentulous patient is interdental papilla. Mandible is more frequently affcted than maxilla.
- Peripheral giant cell granuloma appears as a small, exophytic,well circumscribed, pedunculated lesion on gingival surface.
- Color of lesion varies from purplish red to darkish red.
There can be bleeding from the surface either spontaneously or on provocation from instrument. - Sometimes the peripheral cell granuloma can be aggressive in nature and such lesion may attin very large size and involves some teeth.
In some cases the lesion may develop with an ‘hourglass shape.’
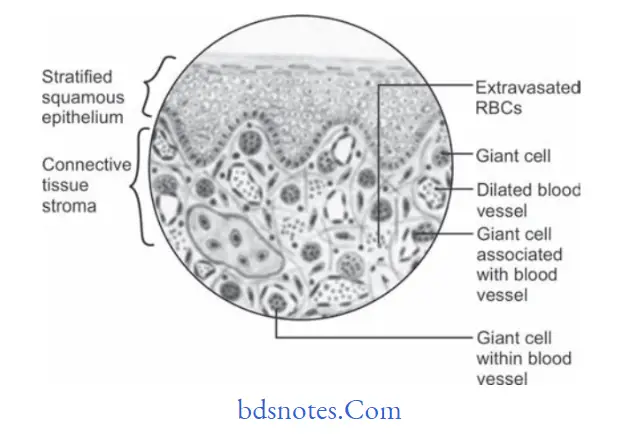
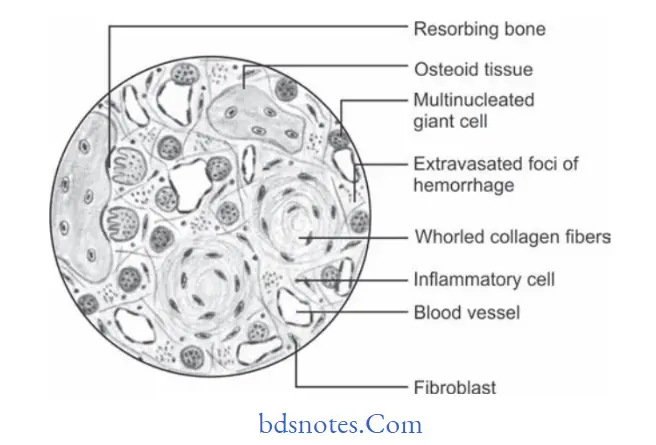
Histopathology
- Peripheral giant cell granuloma present following histological features.
- Overlying covering epithelium is ulcerated with areas of hemorrhage.
- Underlying connective tissue stroma reveals numerous proliferating firoblasts, blood capillaries and multinucleated giant cells, which are scattred throughout the lesion.
- Fibroblasts present in hypercellular stroma are spindle shaped and have oval shaped nuclei.
- Giant cells are large in size and contain more number of nuclei as compared to true giant cell tumor.
- Areas of hemorrhage and hemosiderin pigment are present within connective tissue stroma.
Treatment
Surgical excision with curettage.
Question.8. Write short note in hemangioma.
Answer. Hemangiomas are lesions which are not present at birth but they manifest within the fist month of life, exhibit a rapid proliferative phase and slowly involute to nonexistent.
Classification of Hemangiomas by Watson and McCarthy
- Capillary hemangioma
- Cavernous hemangioma
- Angioblastic hemangioma
- Racemose hemangioma
- Diffse systemic hemangioma
- Metastaizing hemangioma
- Port-Wine stain
- Hereditary hemorrhagic telangiectasia
Clinical Features
- Occur most commonly in infants and children.
- Peak incidence of central hemangiomas is during 2nd decade of life.
- More common in females
- Most commonly affected bones are facial bones, i.e. mandible, maxilla and nasal bones.
- Lesion appears as a flat or raised lesion of mucosa which is deep red or bluish red and is circumscribed.
- Lesion is compressible and filed slowly when released.
- Intra-orally commonly affected sites are lip, tongue, buccal mucosa and palate.
Histopathology
- There are several histopathologic types of hemangioma found in oral cavity, among them two very common types are:
- Capillary hemangioma
- Cavernous hemangioma.
Capillary hemangioma
- They are histologically characterized by numerous, small,endothelial lined capillaries in lesion which are densely packed by erythrocytes.
- Cells of endothelial lining are single layered.
- Endothelial cells are spindle shaped.
- Capillaries are well formed and are present throughout the lesion.
- Fibrous connective tissue stroma is not well formed and is loosely arranged.
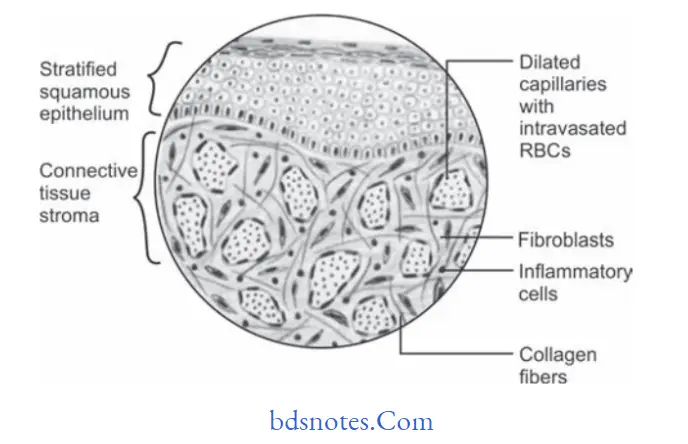
Histopathology Of Cavernous Hemangioma
- They are histologically characterized by large, irregularly shaped, dilated, endothelialized sinuses which contain large aggregates of erythrocytes.
- A single layer of flttd endothelial cell lines each sinus.
- Sinus lacks muscular coat on their walls.
- Large area of hemorrhage and hemosiderin pigments is often seen within cavernous hemangioma lesions.
Treatment
Surgical excision is treatment of choice.
Question.9. Write notes on verrucous carcinoma.
Or
Discuss about verrucous carcinoma.
Or
Describe in detail clinical features, histopathology and treatment of verrucous carcinoma.
Or
Write short note on verrucous carcinoma.
Or
Write short answer on verrucous carcinoma.
Answer. Verrucous carcinoma is a diffused papillary, nonmetastasizing well-differentiated malignant neoplasm of oral epithelium.
It is also known as Ackerman’s tumor.
Clinical Features
- Tumor occurs during 60 years of life and males are more commonly affcted.
- Common locations for verrucous carcinoma are gingiva,alveolar mucosa and buccal mucosa.
- Verrucous carcinoma presents as slow growing, exophytic,papillary growth having white pebbly surface.
- Carcinoma occurs either as single entity or there can be multiple lesions involving diffrent parts of oral cavity.
- Lesions on buccal mucosa are sometimes very extensive and often cause pain, tenderness and diffilty in taking the food.
- Regional lymph nodes are often enlarged and tender.
Histopathology
- Hyperplastic epithelium often exhibits a papillary surface being covered by the thick layer of parakeratin.
- Massively enlarged bulb like acanthotic rete ridges are seen which invaginated into underlying connective tissue stroma.
- Many deep cleft like spaces lined by thick layer of parakeratin, these extend from the surface of epithelium and project deep into the center of bulbous rete ridges. This is known as parakeratin plugging.
- All bulbous rete ridges of the epithelium projects into the connective tissue and is known as pushing margin.
- The basement membrane is intact and underlying connective tissue shows inflammatory cell infitration.
- Formation of epithelial pearls and microcytes are seen.
Treatment
- Surgical excision or laser therapy is done.
- Prognosis should be good.
Question.10. Discuss about central giant cell granuloma.
Answer. Central giant cell granuloma is relatively a common benign intraosseous destructive giant cell lesion which affcts anterior part of jaw bone.
Clinical Features
- Lesion occurs in young children and female predilection is present.
- Central giant cell granuloma affcts the mandible more often than maxilla and occurs anterior to fist molar.
- Central giant cell granuloma is a small, slow enlarging bony hard swelling of jaw which is painful on palpitation.
- Lesion causes expansion and distortion of cortical plates and there is presence of displacement or mobility of regional teeth.
- Central giant cell granuloma follow an aggressive course and in such cases they produce fast enlarging, large,painful swelling in the jaw.
Histopathology
- Central giant cell granuloma exhibits fibro vascular connective tissue stroma, consisting of numerous stromal cell which are plum and spindle shaped and undergo frequent mitosis.
- Several areas of hemorrhage and hemosiderin pigmentations are also evident.
- Multiple multinucleated giant cells of varying size are dispersed throughout firous tissue stroma. Giant cells are found around the blood capillaries or near the area of hemorrhage and giant cells consist of 5 to 20 nuclei.
- Small foci of osteoids are often found near periphery of lesion.
- Little amount of chronic inflmmatory cell infitration in connective tissue stroma.
Radiological Features
- Radiographically the lesion produces multicellular radiolucent area in jaw with soap bubble appearance.
- Margin of lesion is scalloped and well demarcated.
- Resorption of roots of nearby teeth or divergence of roots is common feature.
Treatment
- Surgical excision is done with curettge.
Question.11.Describe the histopathology of moderately diffrentiated squamous cell carcinoma.
Answer.Histopathology
- In it the tumor cells are usually more severely dysplastic than of well diffrentiated type.
- Malignant epithelial cells produce little or no keratin and they exhibit greater number of mitotic division.
- Formation of epithelial islands is diminished since tumor cells do not mature properly.
- Malignant tumor cells are recognized as stratifid squamous epithelial cells.
Question.12. Write notes on giant cell.
Answer. Giant cells are multinucleated cells that commonly occur at sites of chronic inflammation mostly complicated by granuloma formation.
Besides giant cells occurring in various lesions, there also exists physiological giant cells by virtue of the presence of multinucleated nature,present as a part of healthy tissues.
Multinucleated giant cells are highly stimulated cells of the monocytemacrophage lineage at a terminal stage of maturation and studies have demonstrated that their multinucleated appearance is produced by cell–cell fusion rather than by nuclear division without cytokinesis.
Classification of Giant Cells
Giant cell can be classified based according to their occurrence in the body:
- Physiological giant cells:
- Osteoclast
- Striated muscle cells
- Megakaryocytes
- Syncytiotrophoblast
- Pathological giant cells:
- Langhan’s giant cells
- Foreign body giant cells
- Touton giant cells
- Tumor giant cells
- Warthin–fikeldey giant cells
Osteoclast
Osteoclasts are highly specialized for resorption of bone mineral and matrix through the coordinated secretion of hydrogen ions and proteolytic enzymes.
Although most osteoclasts are large multinucleated cells, there are reports of mononuclear osteoclasts.
Situated on the bone surface, it occupies a concavity surface of small bone spicules.
An enlarged surface area created by plasma membrane infoldings, the ruffled border, characterizes the secretory or apical surface directed toward the bone.
In routine histologic sections, the ruffl border appears striated and lightly stained. The presence of a ruffl border is an indication that the osteoclast is actively engaged in bone resorption.
Each ruffl border is surrounded by a clear zone (or sealing zone), a cytoplasmic area rich in cytoplasmic actin fiaments and devoid of major cytoplasmic organelles.
Through close adaptation of the cell surface to the bone matrix, the clear zone establishes a seal between the bone resorption compartment and the interstitial flid.
Striated Muscle
They are the muscles in which the cells exhibit cross striations at the light microscopic level.
It is further sub-classifid based on its location:
- Skeletal muscle
- Visceral striated muscle
- Cardiac muscle
Skeletal Muscle Cell
A skeletal muscle cell is a multinucleated syncytium. In skeletal muscle, each muscle fier is a multinucleated syncytium.
A muscle fier is formed during development by the fusion of small, individual muscle cells called myoblasts.
When viewed in cross section, the mature multinucleated muscle fiers reveal a polygonal shape with a diameter of 10 to 100 µm.
Visceral Striated Muscle
It is morphologically identical to skeletal muscle but is restricted to the soft tissues, namely the tongue, pharynx, lumbar part of diaphragm and upper part of esophagus.
These play an essential role in speech, breathing and swallowing.
Cardiac Muscle
Cardiac muscle has the same type and arrangement of the contractile fiament as skeletal muscle.
In addition, cardiac muscle fiers exhibit densely staining cross bands called intercalated disks, that cross the fiers in a linear fashion or frequently in a way that resembles the rosters of a stairway.
The intercalated disks represent a highly specialized attchment sites between adjacent cells.
The linear cell—cell attchment of the cardiac muscle cells results in ‘fiers’ of variable length.
Megakaryocytes
Platelets are derived from large polypoid cells (cells whose nuclei contain multiple sets of chromosomes) in bone marrow are called megakaryocytes.
Syncytiotrophoblast
- The syncytiotrophoblast is a continuous, normally uninterrupted layer that extends over the surfaces of all villous trees as well as over pAns of the inner surfaces chorionic and basal plates.
- The syncytiotrophoblast is a multinucleated protoplasmic mass without intercellular boundaries.
- From this mass emerge figer like projections, which penetrate through the endometrial epithelium into the endometrial stroma.
Langhans giant Cell
They are characterized by location of the nuclei at the periphery of the cell in an acute confiuration.
They are seen in lesions such as tuberculosis, sarcoidosis, leprosy and vasculitis.
These are special, more highly organized forms than are ‘foreign body’ multinucleated giant cells.
These giant cells may attin diameters of 40 to 50 µm. They have a large mass of cytoplasm containing 20 or more small nuclei arranged peripherally.
Foreign body giant Cell
Formation of foreign body giant cell is hallmark of the foreign body reaction and is harmful to implanted biomaterials because it contributes to the degradation of the biomaterial and leads to stress cracking, tissue firosis and a chronic response.
Foreign body giant cells are thought to be a source of chemokines that mediate the neutrophils and lymphocytes.
Touton Giant Cell
Touton giant cells are characterized by a ring of nuclei surrounding central eosinophilic zone and surrounded by a zone of pallor extending to the periphery of cell.
These giant cells are seen in lesions with high lipid content such as xanthoma, xanthogranuloma, fat necrosis.
The characteristic appearance of ‘Xanthelasmatic giant cell’ of Touton is determined merely by the presence of demonstrable lipid in the cytoplasm.
Tumor Giant Cell
A feature of anaplasia is the formation of tumor giant cells,some possessing only a single huge polymorphic nucleus and others having two or more nuclei.
These giant cells are not to be confused with inflammatory LanghAns or foreign body giant cells, which are derived from macrophages and contain many small normalappearing nuclei.
In the cancer giant cell, the nuclei are hyperchromatic and large in relation to the cell.
Warthin-Finkeldey Giant Cell
The Warthin Finkeldey cells have up to 100 nuclei and contain spherical eosinophilic intracytoplasmic and intranuclear inclusions.
They are present in viral infections like measles.
Tompkins and Macaulay reported Warthin-Finkeldey giant cells in nasal secretions before the appearance of other clinical signs of measles such as Koplik’spots and skin rash.
These cells are found throughout the reticuloendothelial system and contain
up to 100 nuclei.

Question.13. Write notes on special stains.
Answer. The special stains are:
Van Gieson’S Stain
- It is a special stain which is used for connective tissue elements. It is used for differentiating between connective tissue fiers and muscle fiers.
- Epithelium (cell and cytoplasm): It takes greenish-yellow stain.
- Collagen fiers are red
- Muscle fiers are yellow
- Nuclei of cells are blue black.
Mallory stain
- It is a special stain for keratin that stains deep orange. It is used in hyperkeratotic lesions.
- The epithelium is royal blue.
- Collagen fiers are royal blue.
- Muscle fiers are royal blue.
- Keratin layers are orange.
- Nucleus is blue black.
Periodic Acid Schiff’S Stain Or Pas Stain
It is a special stain for mucopolysaccharide granules.
These are prominently seen in basement membrane, intercellular spaces and keratin layer.
It is used to detect continuity of basement membrane in intra epithelial carcinoma and squamous cell carcinoma.
- Epithelium and connective tissue is pink.
- Collagen fiers are pink.
- Muscle fiers are pink.
- Nucleus is blue black.
- Granules are of magenta color.
Masson’s trichrome stain
It is a special stain used to diffrentiate between collagen fiers and muscle fiers. It demonstrates connective tissue disorders like leiomyosarcoma and rhabdomyosarcoma.
- Epithelium is red.
- Muscle fiers are bluish violet.
- Collagen fiers and blood vessels are blue.
Question.14.Defie premalignant lesion and condition. Describe etiology, clinical features, and histopathology of oral submucous firosis.
Or
Define precancerous condition and precancerous lesion. Discuss about etiology and histopathology of OSMF.
Answer. The premalignant lesions are defied as morphologically altered tissue in which cancer is more likely to occur then in its apparently normal counter part, e.g. leukoplakia, erythroplakia, nicotiana palati, stomatitis, dyskeratosis congenita, etc.
- The premalignant condition is defied as generalized state of body, which is associated with significantly increased risk of cancer, e.g. oral sub- mucus firosis, syphilis, lichen planus, etc.
Question.15. Enumerate giant cell lesions. Describe in detail central giant cell granuloma.
Answer. Enumeration of giant cell lesions
Giant cell lesions of oral cavity
According To The Nature Of Different Pathologic
Conditions
- Infections
- Bacterial
- Viral
- Fungal
- Protozoal
- Parasitic
- Fibroosseous lesions and osteodystrophies
- Immunologic
- Idiopathic
- Orofacial granulomatosis
- Reaction to materials
- Benign and malignant tumors
In this Classification Giant Cells are Categorized into three Categories
1. Giant cells are the main cause for the pathology
2. Giant cells characterize these lesions
3. Lesions that may be associated with giant cells
Main Cause for the pathology
- Giant cell granuloma
- Peripheral
- Central
- Giant cell tumors
- Giant cell firoma
- Hyperparathyroidism
Giant Cells That Characterize Lesions
- Infections
- Tuberculosis
- Hansen’s disease
- Syphilis
- Measles
- Granulomatous lesions
- Wegener’s granulomatosis
- Orofacial granulomatosis
- Pulse granuloma
- Sarcoidosis
- Lesions in bone
- Aneurysmal bone cyst
- Cherubism
- Paget’s disease
- Foreign body lesions
- Silicosis
- Berylliosis
- Malignancies
- Lymphoma- hodgkin’s disease
- Bronchogenic carcinoma
- Carcinoma of thyroid
- Miscellaneous
- Xanthoma
- Giant cell arteritis
Lesions that may be associated with giant Cell
- Malignancies
- Multiple myeloma
- Ewing’s sarcoma
- Fibrosarcoma
- Chondrosarcoma
- Fibroosseous lesions
- Osteoblastoma
- Fibrous dysplasia
- Cemento-ossifying firoma
- Radicular cyst
Based on their origin
- Epithelially derived, i.e. Warthin-fikeldey giant cells,tumor giant cells
- Stromally derived, i.e. Reedsternberg giant cells.
Question.16. Enumerate and classify non-odontogenic tumors of oral cavity. Write briefl about malignant melanoma.
Answer.
Non-Odontogenic Tumors Of Oral Cavity
Epithelial Tissue
Benign tumors
- Papilloma
- Keratoacanthoma
- Squamous acanthoma
- Nevus
Malignant tumors
- Squamous cell carcinoma
- Mucoepidermoid carcinoma
- Adenocarcinoma
- Basal cell carcinoma
- Transitional cell carcinoma
- Melanoma
- Verrucous carcinoma
- Intraepidermoid carcinoma
Fibrous Connective Tissue
Benign tumors
- Fibroma
- Fibrous hyperplasia
- Fibrous epulis
- Giant cell firoma
- Myxoma
- Myxofiroma.
Malignant tumors
- Fibrosarcoma
Cartilage Tissue
Benign tumors
- Chondroma
- Chondroblastoma
- Chondromyxoid firoma.
Malignant tumors
- Chondrosarcoma
Adipose Tissue
Benign tumors
- Lipoma
- Angiolipoma.
Malignant tumors
- Liposarcoma
Bone
Benign tumors
- Osteoma
- Osteoid osteoma
- Osteoblastoma
Malignant tumors
- Osteosarcoma
- Osteochondrosarcoma
Vascular Tissue
Benign tumors
- Hemangioma
- Hereditary hemorrhagic telangiectasia
- Lymphangioma
Malignant tumors
- Hemangioendothelioma
Neural Tissue
Benign tumors
- Neurofibroma
- Neurilemmoma
- Schwannoma
Malignant tumors
- Neurosarcoma
- Neurofirosarcoma
Muscles
Benign tumors
- Leiomyoma
- Rhabdomyoma
Malignant tumors
- Leiomyosarcoma
- Rhabdomyosarcoma
Giant Cell Tumor
- Central and peripheral giant cell tumor
- Giant cell granuloma
- Giant cell tumor of hyperthyroidism.
Teratoma
Salivary Gland Tumor
Benign tumors
- Adenoma
- Warthin’s tumor
- Pleomorphic adenoma.
Malignant tumors
- Mucoepidermoid carcinoma
- Adenocystic carcinoma
- Adenocarcinoma
- Acinic cell carcinoma
- Malignant change in pleomorphic adenoma
Lymphoid Tissue
Malignant tumors
- Hodgkin’s and non-hodgkin’s lymphoma
- Lymphosarcoma
- Reticular cell sarcoma
- Ewing’s sarcoma
- Burkitts lymphoma
- Multiple myeloma
- Leukemia.
Malignant melanoma
Malignant melanoma is a neoplasm of epidermal melanocytes.
It is the third most common cancer of the skin.
Etiology
- Sun exposure: Persons who are exposed to the excess of sunlight develops malignant melanoma.
- Artifial UV source: PUVA thearpy has been reportedly associated with risk of melanoma.
- Socioeconomic status: It is seen in high socioeconomic status since people of high socioeconomic status go for holidays.
- Fare skin, freckles, red hair: These characteristics increased the risk of melanoma.
- Melanotic nevi are the strong risk factors.
- Genetic factors: Familial melanoma and xeroderma pigmentosum are considered to be strong genetic factors for development of malignant melanoma.
Clinical types of malignant melanoma
- Superficial spreading melanoma: Exists in a radial growth phase. Lesion present as tan, brown or black admixed lesion on sun exposed skin. Radial growth phase may last for several months to years.
- Nodular melanoma: It exists in a vertical growth phase. It present sharply delineated nodule with varying degrees of pigmentation. They may be pink or black.
- Lentigo maligna melanoma: Exists in a radialgrowth phase. The lesion occur as macular lesion on malar skin of Caucasians.
Acral lentiginous melanoma: Melanoma developing on the palms and soles as well as toe and figers. It is characterized by macular lentiginous pigmented area around nodule. - Mucosal lentiginous melanoma: Develops from mucosal epithelium that lines respiratory, gastrointestinal and genitourinary systems. It is more aggressive.
- Amelanotic melanoma: It is an erythematous or pink sometimes eroded nodule.
Clinical Features
- Oral melanomas initiate as macular pigmented focal lesions.
- Most of the lesions are pigmented excepting few nonpigmented lesions which referred to as “amelanotic melanomas”, which appear as “slightly” inflamed looking areas.
- Pigmented lesions are often darkbrown, bluishblack or simply black in appearance.
- Initial macular lesions grow very rapidly and often result in a large, painful, diffse mass.
- Surface ulceration is very common and beside; this, hemorrhage, paresthesia and superficial fungal infections are often present.
- As the tumor continues to grow, small satellite lesions can develop at the margin of the primary tumor.
- Like other epithelial malignant tumors, melanomas exhibit litte or no induration at the periphery.
- Oral melanomas often cause rapid invasion and extensive destruction of bone. This often results in loosening and exfoliation of the regional teeth in the jaw.
- Widespread dissemination of the tumor cells occurs frequently in the lymph nodes as well as in the distant sites,e.g. the lung, liver, bone and brain, etc.
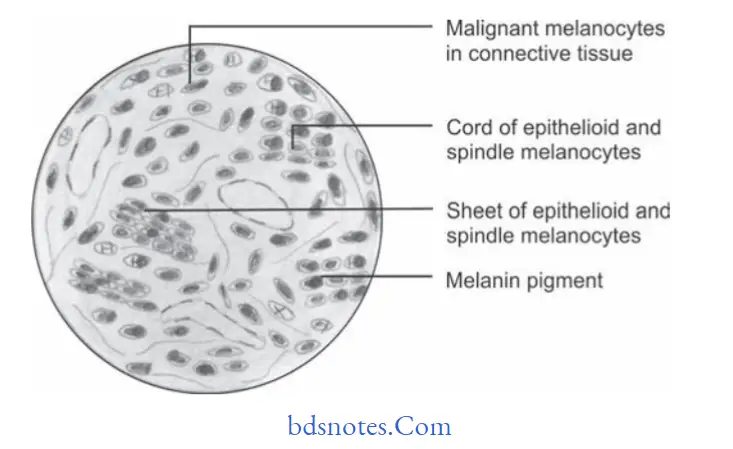
Histopathology
- Microscopically the malignant cells lie in nest or cluster of groups in an organoid fashion.
- Melanoma cells have large nuclei, often with prominent nucleoli and show nuclear pseudoinclusion.
- Cytoplasm of the cell is abundantly eosinophilic or optically clear.
There is presence of large, epithelioid melanocytes distributed in pagetoid manner. - When melanocytes penetrate the basement membrane a flrid host cell response of lymphocytes develop.
- Macrophages or melanophages may be present.
- Vertical growth phase is characterized by the proliferation of malignant epithelioid melanocytes in the underlying connective tissues.
- These malignant melanocytes often exhibit extensive cellular pleomorphism and nuclear hyperchromatism.
- However, in some lesions melanin production by the tumor cells can be very little and on few occasions there can be virtually no melanin production.
Treatment
- Radical surgery with prophylactic neck dissection is often advised.
Question.17. Describe in brief teratoma.
Answer. A true teratoma is a developmental tumor composed of tissues from all three germ layers, i.e. ectoderm, mesoderm and endoderm:
- Such tumors are believed to derive from germ cells or entrapped totipotent blastomeres which can produce derivatives of all three germ layers.
- Teratomas are more common in ovaries and or testis and can be benign or malignant.
Clinical Features
- It is most commonly seen in infants.
- Orally it involves soft palate and hard palate. Systemically it involves testis, ovary, abdominal viscera and pineal region.
- It consist of teeth, sebaceous material and some hairs.
Histopathology
- H and E-stained section show stratifid squamous epithelium with epithelial appendages consisting of sebaceous glands, sweat glands, hairs, salivary glands, teeth.
- At times thyroid gland tissue and pancreatic tissue can be seen.
Treatment
Surgical excision of tumor should be done.
Question.18.Write in detail about Hodgkin’s lymphoma.
Answer. It is also known as hodgkin’s disease.
- Epstein-Barr virus is considered to be the major cause.
- Patients with HIV infection have higher incidence of Hodgkin’s disease.
Clinical Features
- It is most commonly seen in young adults and older individuals.
- More common in males as compared to females.
- Clinical signs and symptoms of the disease are protean
- There is painless enlargement of one or more cervical lymph nodes.
- Palpable painless cervical lymphadenopathy occurs in cervical area, axilla and less commonly in inguinal area and Waldeyers ring and occipital nodes.
- Lymph nodes are fim and rubbery in consistency and overlying skin is normal.
- Symptoms are of unexplained weight loss, fever and night sweats.
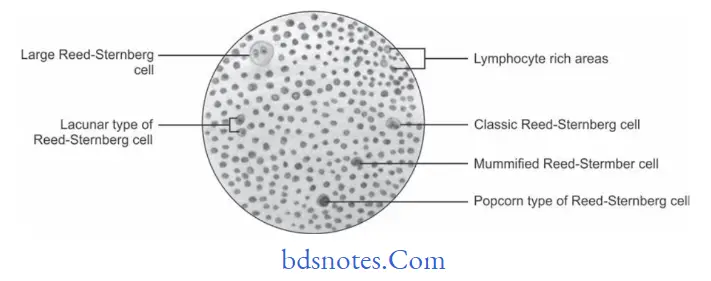
Histopathology
- Nodular sclerosis hodgkin’s disease
- Morphology show nodular pattrn.
- Broad bands of fiers divide node into nodules
- Characteristic cell is lacunar type ReedSternberg Cell which has monolobated, multilobated nucleus and a small nucleolus with abundant and pale cytoplasm.
- Mixed cellularity hodgkin’s disease
- Infiltrate is usually diffuse
- ReedSternberg cells are of classic type i.e. large with bilobate, double or multiple nuclei and a large eosinophilic inclusion like nucleolus.
- Lymphocyte-depleted hodgkin’s disease
- Infiltrate is diffuse and often appears hypocellular.
- Large number of ReedSternberg cells and bizarre sarcomatous variants are present.
- It is associated with older age and HIV positivity
- Lymphocyte-rich classic hodgkin’s disease
- ReedSternberg cells of the classic or lacunar type are observed with background infitrate of lymphocytes.
- Nodular lymphocyte-predominant hodgkin’s disease
- In this typical ReedSternberg Cell is not seen, instead a variant of Reed
- Sternberg Cell the lymphocytic and histiocytic cells or popcorn cells are seen within the background of inflammatory cells which are predominantly benign lymphocytes.
Treatment
Combination of radiotherapy and chemotherapy help in curing the disease.
Question.19. Write in detail on squamous cell carcinoma.
Enumerate all malignant epithelial neoplasms. Describe in detail histopathology of oral squamous cell carcinoma.
Or
Enumerate malignant tumors of epithelial origin. Describe in detail about squamous cell carcinoma.
Answer. Enumerationofmalignantepithelialneoplasms/Tumors:
- Basal cell carcinoma
- Squamous cell carcinoma
- Verrucous carcinoma
- Adenoid squamous cell carcinoma
- Malignant melanoma
- Spindle cell carcinoma
- Primary intra-alveolar carcinoma
- Multicentric oral carcinoma.
Squamous Cell Carcinoma
- Squamous cell carcinoma is defined as a malignant epithelial neoplasm exhibit squamous differentiation as characterized by formation of keratin and/or presence of intercellular bridges. (Pindborg et al, 1997)
- Squamous cell carcinoma is the commonest malignant epithelial tissue neoplasm of oral cavity. It is mostly derived from stratifid squamous epithelium.
Etiology
Following are the etiological factors which lead to squamous cell carcinoma:
- Tobacco smoking: Cigaretts, bidis, pipes, cigars and reverse smoking.
- Use of smokeless tobacco: Snuf dipping, gutkha, tobacco chewing, tobacco as a toothpaste.
- Alcohol: Drinking spirits, Drinking wines, drinking beers
- Diet anal nutrition: Vitamin A, B-complex and C defiiency,
- Nutritional defiiency with alcoholism.
- Dental factors: Chronic irritation from broken teeth, Illfitng or broken prosthesis.
- Radiations: Actinic radiation, Xray radiation
- Viral infections: Herpes simplex virus (HSV), Human papilloma virus (HPV),
- Human immunodeficiency virus (HIV),
- EpsteinBarr virus (EBV).
- Chronic infections: Candidiasis, syphilis
- Genetic factors: Oncogenes, Tumor suppressor genes
- Pre-existing oral diseases: Lichen planus, PlummerVinson Syndrome, discoid lupus erythematosus, OSMF.
Clinical Features
- Carcinomas mostly occur in the 4th to 7th decades of life.
- Males are more commonly affcted
- Lower lip is the most common site, the second most common site is the lateral border of the tongue.
Among all intraoral sites, dorsum of the tongue and hard palate are the least common sites for oral squamous cell carcinoma. - Initial lesion may be asymptomatic or can be presented as white or red nodule or fisure over the oral mucosa.
- Initially the lesion is usually painless.
- More advanced lesions present either as a fast enlarging,exophytic or invasive ulcer or sometimes as a large tumor mass or a verrucous growth.
- Ulcerated lesion often shows persistent induration around the periphery with an elevated and everted margin.
- Lesion can be painful either due to secondary infection or due to involvement of the peripheral nerves by the tumor cells. Lesion can also bleed easily.
- Lesions of flor of mouth often cause fiation of the tongue to the underlying structures with diffilty in speech and inability to open the mouth.
- When malignant tumor cells invade into the alveolar bone of either maxilla or mandible, they usually cause mobility or exfoliation of regional teeth.
- Involvement of inferior alveolar nerve often causes paresthesia of the lower teeth and the lower lip.
- Regional lymph nodes are often enlarged, tendered and fied; some of these nodes can be stony hard in consistency.
- Untreated lesions may sometimes destroy the oral tissues and extend into the skin on the outer surface of the face to produce a nodular or lobulated growth on the facial skin,which appears as an extraoral discharging sinus.
- Pathological fracture of the jaw bone may sometimes occur in untreated cases due to extensive destruction of the bone by the tumor.
Histological Features
Histological fiding as given by Broder’s grading for squamous cell carcinoma.
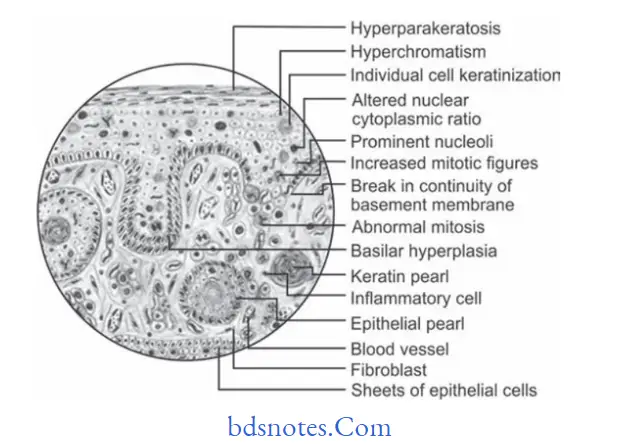
Well-differentiated Squamous Cell Carcinoma
- Most of the squamous cell carcinomas histologically belong to the well-diffrentiated category.
- In this lesion, the tumor epithelial cells to a large extent resemble the cells of the squamous epithelium both structurally and functionally.
- Tumor cells produce large amount of keratin in the form of “keratin pearls”.
- Tumor cells invade into the underlying connective tissue, where the cells proliferate further and give rise to the formation of many epithelial islands within the connective tissue stroma.
- Tumor cells often exhibit dysplastic features like cellular pleomorphism, nuclear hyperchromatism, individual cell keratinization, and altered nuclearcytoplasmic ratio, loss of cohesion, etc.
- Prognosis is better.
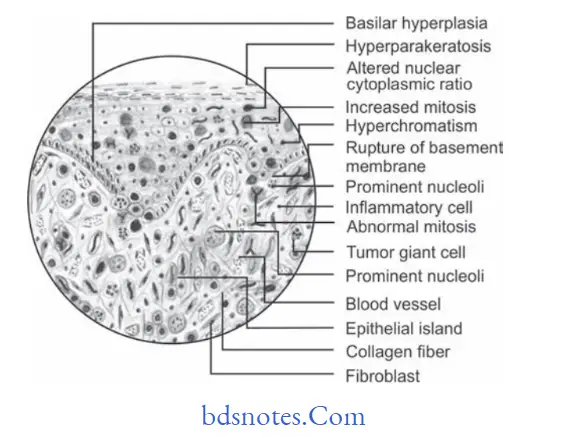
Moderately-differentiated squamous Cell Carcinoma
- Tumor cells are usually more severely dysplastic than that of the well-differentiated type.
- Growth rate of individual cells is more rapid and this is reflcted in greater number of mitotic fiures.
- There is formation of epithelial islands or cell nests, etc. are diminished since these tumor cells do not differentiate or
mature as much as the well differentiated type of cells do. - This tumor also carries a reasonably good prognosis.
Poorly-differentiated squamous Cell Carcinoma
- In poorly differentiated squamous cell carcinoma, the malignant tumor cells produce no keratin .
- The tumor exhibits extensive cellular abnormalities with lack of normal architectural pattern and loss of intercellular bridges between the tumor cells.
- Mitotic cell division is extremely high and because of this,the neoplastic cells are often very immature and primitive looking and it is often very difficult even to recognize them as squamous epithelial cells.
- Prognosis is poor.
Investigations
- Biopsy of the involved area should be done for confimation of diagnosis.
- Toluidine blue test should be done.
- Tumor markers like cytokeratins, epithlial membrane
antigen, carcinoembryonic antigen (CEA) and alphafetoprotein should be used for detection of cancer.
Treatment
Surgical excision of the involved site is the treatment of choice.
Question.20.Defie neoplasm. Describe in brief clinical features,X-ray details and histopathology of osteogenic sarcoma.
Answer. “A neoplasm is an abnormal mass of tissue, the growth of which exceeds and is uncoordinated with that of the normal tissues and persists in the same excessive manner after cessation of the stimuli which evoked the change.” Willis
Osteogenic Sarcoma
It is a common malignant neoplasm arising from the bone and beside plasma and myeloma.
Clinical Features
- It occurs during 10–25 years of age in the jaw and males are more commonly affected.
- The tumor involves maxilla more often than mandible.
- A very fast enlarging, painful swelling of jaw, causes expansion and distortion of cortical plates.
- Severe facial deformity and diffilty in taking the food due to restricted jaw movement.
- Displacement and loosening of regional teeth.
- Ulceration, hemorrhage and pathological fracture of bone are commonly associated.
X-ray Details
The Xray details of osteosarcoma are divided into following stages, i.e.
Osteolytic Stage
- It reveals moth eaten appearance.
- Border of the lesion at this stage are ill-defied.
- There is perforation and expansion of cortical plates.
- Lamina dura is absent, i.e. it get destroyed.
- Pathological fracture may be present.
- Root resorption is present.
Mixed Stage
- It is called as mixed because this stage show formation and destruction of bone.
- It reveals honeycomb appearance.
- Margins of lesion are ill defied.
Osteoblastic Stage
- It reveals sun ray appearance.
- At times subperiosteal bone laid down in layers which results in onion peel appearance.
- In osteosarcoma periosteum is elevated over the expanding tumor mass in a tent like fashion. At point on the bone where the periosteum begin to merge an acute angle between periosteum and bone is created which is known as
- Codman’s Triangle.
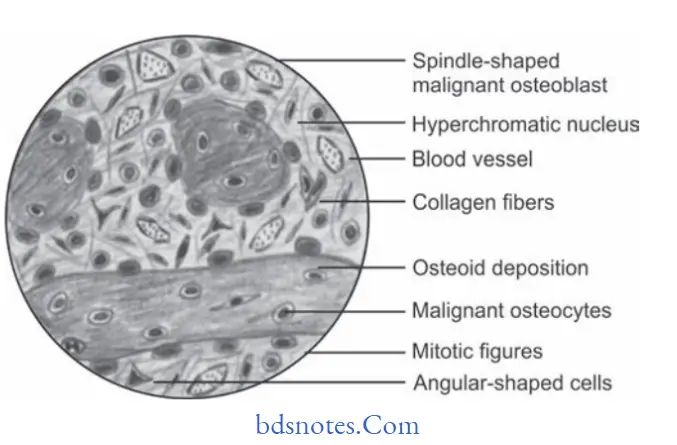
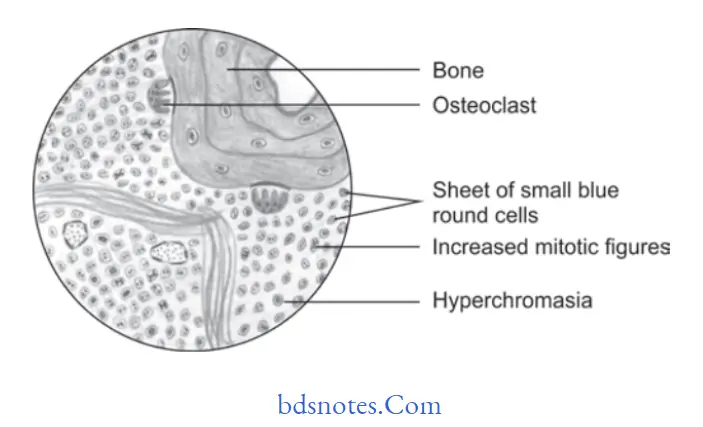
Histopathology
- There will be presence of numerous, actively proliferating,spindle shaped, oval or angular, malignant osteoblast cells within cellular stroma.
- The malignant osteoblast cells exhibit cellular pleomorphism, abnormal increased mitosis and nuclear hyperchromatism
- Multiple areas of newly formed bone or osteoid tissue are often present within firous stroma.
- In chondroblastic variations the malignant tumor cells produce large amount of cartilagenous tissue within tumor.
Question.21.Define oral submucous firosis. Describe in detail etiopathogenesis and histopathology of same.
Answer. OSMF is defined as “An insidious chronic disease affcting any part of oral cavity and sometime pharynx.
Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxtaepithelial inflammatory reaction followed by firoelastic changes in lamina propria, with epithelial atrophy leading to stiffess of oral mucosa and causing trismus and inability to eat.” — Pindborg (1966)
Etiopathogenesis
- Betel nut: Tannic acid and arecoline present in betel nut affct the vascular supply of oral mucosa leading to a neurotropic disorder. Nitrosation of arecoline causes formation of nitrosoguvacine and nitrosoguvacoline as well as 3 methyl nitrosamino propionitrile which leads to alkylation of DNA. Metabolism of nitrosoguvacine and nitrosoguvacoline as well as 3 methyl nitrosamino propionitrile causes formation of cyanoethyl. Cyanoethyl interacts with O’ methyl guanine in DNA. Constant ir
ritation by this leads to OSMF and exposure for long time leads to malignant transformation.
Recent concept: Arecoline in betel nut stimulates fibroblasts. Fibroblasts proliferates and produce collagen. Flavonoids, i.e. catechin and tannin in betel nut stabilizes collagen fiers which make them resistant to degradation by collagenase enzyme. Trismus is caused due to juxtaepithelial hyalinization as well as involvement of the secondary muscles. Increased muscle activity leads to glycogen depletion and reduced blood supply due to connective tissue changes leads to degeneration of muscle and also cause firosis. - Tobacco and lime: Tobacco act as a local irritant which leads to OSMF. Lime causes local irritation as well as vesicle and ulcer formation in the oral mucosa.
- Chilies: Capsaicin is an active ingredient present in red chillies. It is the irritant in chillies which leads to oral submucous firosis.
- Hereditary: Presence of genetic susceptibility is present.
Familial occurrence of OSMF is seen. - Immunological Studies: It was found that human leukocyte antigen (HLA) A10, B7 and DR3 occur signifiantly more frequently in oral submucous firosis.
Question.22.Classify the nonodontogenic tumors of oral cavity and describe firoma.
Or
Write short answer on firoma.
Answer.
Fibroma
It is a benign tumor of connective tissue origin.
Clinical Features
- It is a slow growing lesion and can be seen during 3rd, 4th and 5th decades of life.
- Female predilection is seen.
- It can occur anywhere in the oral cavity but most commonly it is seen on buccal mucosa along plane of occlusion. It also affcts gingiva, tongue, buccal mucosa,lips and palate.
- Lesion appears as elevated nodule of normal color with smooth surface and a sessile or at times pedunculated base.
- Its size can ranges from several millimeters to centimeters.
- Lesion if traumatized it become painful.
- Color of the lesion is pink and texture is smooth.
- Consistency of lesion can be soft or fim or can be elastic.
- At times lesion is traumatized and become inflmed and show ulceration or hyperkeratosis.
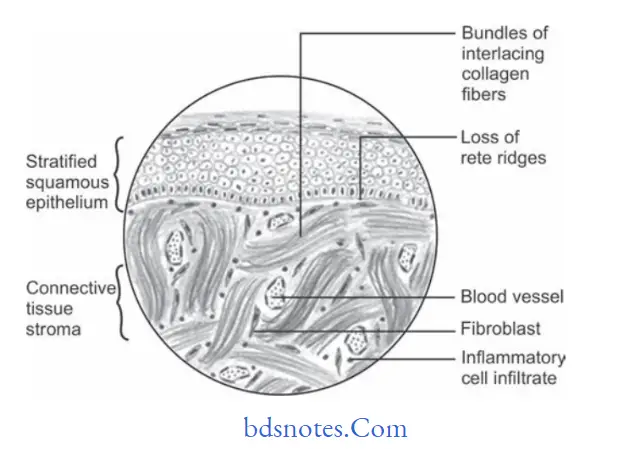
Histopathology
- Lesion consists of stratifid squamous epithelium which show shortening and fitting of rete pegs.
- Underlying connective tissue stroma show bundles of interlacing collagen fiers which are interspersed with numerous firoblasts.
- There is presence of chronic inflammatory cell infitrate
consisting of lymphocytes and plasma cells. - Areas of calcification and ossifiation can also be seen.
Treatment
Excision of the lesion should be done.
Question.23. Enumerate non-odontogenic connective tissue malignant tumors. Discuss in detail about clinical features, etiology and histopathology of firosarcoma.
Answer. Enumeration of non-odontogenic connective tissue malignant tumors
- Fibrous connective tissue: Fibrosarcoma
- Adipose Tissue: Liposarcoma
- Cartilage: Chondrosarcoma
- Bone
- Osteosarcoma
- Osteochondrosarcoma
- Vascular:
- Hemangioendothelioma
- Angiosarcoma
- Kaposi sarcoma
- Neural tissue: Neurosarcoma or Neurofirosarcoma
- Muscle
- Leiomyosarcoma
- Rhabdomyosarcoma
- Lymphoid tissue
- Hodgkin and NonHodgkin lymphoma
- Lymphosarcoma
- Reticular cell sarcoma
- Ewing’s sarcoma
- Burkitts lymphoma
- Multiple myeloma
- Leukemia.
Fibrosarcoma
- It is the malignant firous connective tissue tumor and is the malignant tumor of firoblasts.
Clinical Features
- It arises at any age but mean age is 40 years.
- Male predilection is seen.
- It is most commonly seen in lower extremities i.e. femur and tibia.
- In oral cavity tumor involves mandible, maxilla, maxillary sinus, lip and palate.
- Tumor is generally a large painless mass which lies deep to fascia and has ill-defied margin.
- Associated teeth become mobile.
- Tumors in starting show benign growth and later on they spread rapidly producing large tumor with ulceration and hemorrhage.
- They can also cause pathological fracture.
Etiology
- Most of the firosarcomas arise from preexisting lesions such as Paget’s disease, firous dysplasia chronic osteomyelitis, bone infarcts and in previously irradiated areas of bone.
- Congenital firosarcomas are thought to arise from genetic mutations.
Histopathology
- Various histological grading of firosarcoma are:
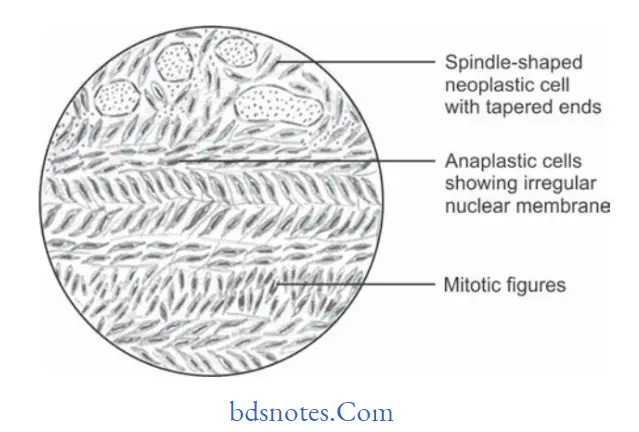
Well-differentiated
- In this multiple plump-shaped firoblasts with pale eosinophilic cytoplasm, hyperchromatic spindleshaped nuclei with tapered ends is seen.
- Malignant firoblasts are dispersed in rich collagen area.
- Few mitotic fiures are evident.
Intermediate Grade
- In this tumor show Herring bone pattrn, i.e. parallel sheets of cells arranged in intertwining whorls.
- Cellularity is high.
- Cellular pleomorphism is evident.
- Areas of hyalinization can be appreciated.
High Grade
- Marked cellular atypia and mitotic activity is evident.
- This grade is highly anaplastic and pleomorphic with bizarre nuclei.
Question.24. Write short note on keratoacanthoma.
Answer. It is also known as molluscum sebaceum, selfhealing carcinoma or pseudocarcinoma.
It clinically and histologically resembles epidermoid carcinoma so it is mistaken as oral carcinoma.
Etiology
- Hereditary predisposition is present.
- Human papilloma virus (HPV) 26 or 37 can lead to keratoacanthoma.
- Sun exposure
- Chemical agents such as coal tar and minerals
Clinical Features
- Its occurrence is at the age of 50 to 70 years. Male predilection is present.
- Intraorally, it is most commonly found on lips.
- Lesion is painful and regional lymphadenopathy is present.
- Lesion is elevated, umblicated with depressed central core with presence of plug of keratin. Lesion appears as dome shaped.
- Margins of lesions are sharply delineated.
- Lesion begins as small nodule which increases in size from 4 to 6 weeks. Later on it undergoes spontaneous regression from 6 to 8 weeks with scar formation.
Histopathological Features
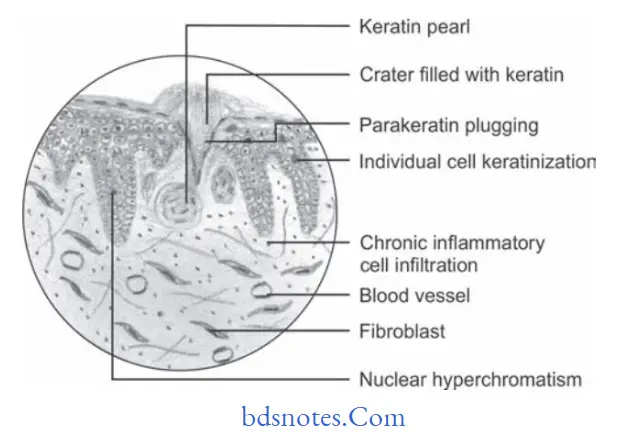
- Hyperplastic squamous epithelium growing into underlying connective tissue.
- Epithelial surface is covered by parakeratin or orthokeratin with parakeratin plugging.
- Pseudocarcinomatous infiltration typically present smooth, regular, well demarcated front which does not extend beyond the level of sweat gland.
- Connective tissue show chronic inflmmatory cell infitration.
- Most characteristic feature of lesion is seen at the margins where normal adjacent epithelium is elevated towards central portion of crater, later on an abrupt change in normal epithelium occurs as hyperplastic acanthotic epithelium is reached.
Treatment
Surgical excision.
Question.25. Write short note on Kaposi’s sarcoma.
Answer. It is also known as multiple idiopathic hemorrhagic sarcoma of Kaposi.
- Kaposi’s sarcoma is the multicentric proliferation of vascular or spindle cell components.
- Kaposi’s sarcoma is currently associated with HIV/AIDS.
Clinical Features
- Clinically, Kaposi’s sarcoma is of four types, i.e.
- Classic (Chronic)
- Endemic (Lymphadenopathic; African)
- Immunosuppression associated (Transplant)
- AIDS related.
Classic type
- Development of cutaneous multifocal blue red nodules on the lower extremities.
- Lesion slowly increases in size and number with some of the lesions extinguishing and new ones forming on adjacent or distinct skin.
- Orally, soft bluish nodules occur on palatal mucosa or gingiva.
Lymphadenopathic
- Present in young African children.
- There is generalized or localized enlargement of lymph node chain which includes cervical lymph nodes.
- Disease follow fulminant course with visceral involvement and minimum skin or mucous membrane involvement.
Immunosuppression Associated
- It is usually seen in renal transplant patients.
- It occurs 1 to 2 years after transplantation
- Progression of disease is directly proportional to loss of cellular immunity of host.
AiDs Related
- Homosexual AIDS patients have maximum chances of developing Kaposi’s sarcoma.
- Lesions occur on cutaneous lesions i.e. along lines of cleavage and tip of nose.
- Oral lesions can occur anywhere in oral cavity, but predilection is for palatal mucosa and gingiva.
- Early oral mucosal lesions are flt and slight blue, red or purple plaques, either focal or diffse and may be completely asymptomatic.
- Later on these lesions may be more deeply discolored and there is development of surface papules and nodules which may become exophytic and ulcerated. These lesions can also bleed.
- Cervical lymphadenopathy and salivary gland enlargement is seen.
Histopathology
Early Lesion Or Patch Stage
- There is proliferation of small veins and capillaries around one or more preexisting dilated vessels.
- Slit like vessels are seen near periphery of preexisting blood vessel, skin adnexa and in between collagen fiers.
- Slit like vessels are lined by plump, mild atypical endothelial cells.
- There is presence of mononuclear inflmmatory cell infitrate consisting of mast cells, scattred erythrocytes and hemosiderin deposit.
Advance Lesion Or Plaque Stage
- There is presence of increased numbers of increased capillaries and dilated vascular channels which are interspersed with proliferating sheets of sarcomatous cells with large number of extravasated erythrocytes.
- Slit like vessels without visible endothelial lining are interspersed with spindle cells.
- Lesional cells show enlarged, hyperchromatic nuclei with mildtomoderate pleomorphism.
Nodular Stage
In all features are more prominent than plaque stage.
Question.26. Write short note on tori.
Answer. Tori are of two types, i.e. torus palatinus and torus mandibularis
Torus Palatinus
It is a slow growing, flt based boney protuberance which occurs in midline of hard palate.
Clinical Features
- Women are affcted more commonly.
- Torus palatinus can occur at any age. It reaches at its peak incidence at age of 30 years.
- It is an outgrowth in the midline of palate.
- It is spindle shaped, nodular or lobular.
- Mucosa overlying torus is intact and occasionally it appears blanched.
- It may become ulcerated if traumatized.
- Torus itself may be composed of dense compact bone or dense compact bone with center of cancellous bone.
Torus Mandibularis
It is an exostosis or outgrowth of mandible found on the lingual surface.
Clinical Features
- Growth on lingual surface of mandible occurs at mylohyoid line which is usually opposite to cuspid teeth.
- Mandibular tori are bilateral.
- Bilateral overgrowths are globular or they are multiple.
Treatment
For both tori treatment is surgical excision.
Question.27. Write short note on congenital epulis.
Answer. It is also known as congenital epulis of newborn or
Neumann’s tumor.
It is benign in nature and mostly occurs as single tumor.
Clinical Features
- Tumor is present at birth.
- It is located over maxillary or mandibular gingiva. But more common on maxillary.
- Lesion is pedunculated and is found on incisor region arising from crest of alveolar ridge or alveolar process.
- Lesion varies from few centimeters to millimeters.
Histology
- Presence of sheets of large closely packed cells showing fie, granular, eosinophilic cytoplasm which comprises the tumor mass.
- Numerous capillaries are present.
Treatment
- Surgical Excision.
Question.28. Enumerate malignant epithelial tumors of oral cavity.
Discuss about etiology, clinical features and histopathology of verrucous carcinoma.
Answer. Enumeration of malignant epithelial tumors of oral cavity
- Squamous cell carcinoma
- Intraepidermoid carcinoma
- Adenocarcinoma
- Metastatic carcinoma
- Basal cell carcinoma
- Transitional cell carcinoma
- Malignant melanoma
- Verrucous carcinoma
- Intraepidermoid carcinoma
- Spindle cell carcinoma
- Primary intra-alveolar carcinoma
- Adenoid squamous cell carcinoma.
Etiology
Tobacco: Verrucous carcinoma develops in tobacco chewers. It usually occurs in the buccal sulcus area where the person holds the tobacco most.
Question.29. Write in brief lipoma.
Answer. Lipoma is a rare intraoral tumor.
It is a benign, slow growing tumor of mature fat cells.
Classification
On the basis of morphology
Superficial: It is a single, yellow, lobulated, painless lesion with sessile or pedunculated base.
Diffse: It occurs in deeper tissues and produces a slight surface elevation.
Encapsulated: It is surrounded by a capsule.
Pathogenesis
- HMGIC gene which is mapped to 12q15 is a member of high mobility group protein gene family, play a role in development of lipoma.
- Cells of lipoma are different metabolically as compared to normal fat cells. Precursors of fatt acid should be incorporated at faster rate in fat of lipoma as compared to normal fat and there is reduction in lipoprotein lipase activity.
Clinical Features
- Lipomas commonly occur in adults, usually around 3rd and 4th decades of life or in older individuals too.
- Lipomas are soft, smooth surface and nodular masses which can be sessile or pedunculated.
- It is asymptomatic for months or years.
- Buccal mucosa and buccal vestibule are the most common sites which are affected. Other sites involved are tongue,flor of mouth and lips.
- The lesion is 3 cm in size but with time, its size increases up to 5 to 6 cm.
Histopathology
- Lesion consists of mature fat cells and can demonstrate a thin firous capsule.
- Lesion shows the lobular arrangement of fat cells.
- Various microscopic variants of lipoma are appreciated histologically, i.e.
- Fibrolipoma: Fibrous component intermixed with lobules of fat cells.
- Angiolipoma: Admixture of mature adipocytes and multiple small blood vessels.
- Spindle cell lipoma: Variable amount of spindle cell in conjunction with lipomatous component.
- Pleomorphic lipoma: Presence of spindle cells along with bizarre,hyperchromatic giant cells.
- Myolipoma: When spindle cells are of smooth muscle origin
- Intramuscular lipomas: Infitrative growth of mature adipocytes which extend between skeletal muscle bundles.
- Myxoid lipoma: If stromal background is myxoid.
Treatment
Conservative local excision is the treatment of choice.
Question.30. Write short note on Ewing’s sarcoma—histopathology.
Answer. Following is the histopathology of Ewing’s sarcoma:
- The lesion consists of solid sheets of small round cells with very minimal stroma but at a few places connective tissue septae are present.
- Cells are round and small in shape along with scanty cytoplasm, nuclei of the cell is large round to oval in shape along with dispersed chromatin and hyperchromasia.
- Borders of cell are ill defied.
- Cells also show mitotic fiures.
- Cells of the sarcoma are arranged in fiigree pattrn.
- Small vascular channels are also evident.
- Hemorrhage along with vascular lakes or sinuses are appreciated.
- Perivascular sparing and geographical necrosis is very common in Ewing’s sarcoma.
Question.31. Write short note on epithelial dysplasia.
Answer. Epithelial dysplasia comprises a loss in the uniformity of individual cells or cytological atypia as well as a loss in their architectural orientation.
Dysplasia is a histopathological diagnosis which is made on the basis of presence of certain histological and cytological features in premalignant lesions and conditions.
Architecture and Cytologic Criteria for grading epithelial
Dysplasia Given by WHO (2005)
Architecture Criteria
- Irregular epithelial stratifiation
- Loss of polarity of basal cells
- Basal cell hyperplasia
- Dropshaped rete pegs
- Increased number of mitotic fiures
- Abnormally superfiial mitosis
- Dyskeratosis, i.e. premature keratinization in the cell
- Keratin pearls within rete ridges.
Cytologic Criteria
- Anisonucleosis: Abnormal variation in nuclear size
- Nuclear pleomorphism: Abnormal variation in nuclear shape
- Anisocytosis: Abnormal variation in cell size
- Cellular pleomorphism: Abnormal variation in cell shape
- Increased nuclear cytoplasmic ratio
- Increased nuclear size
- Atypical mitotic fiures
- Increase in the number and size of nucleoli
- Hyperchromatism.
Grading Of Epithelial Dysplasia
- Histopathological interpretation of potentially malignant disorders shows presence of epithelial dysplasia.
- There are numerous prognostic molecular markers but the epithelial dysplasia is considered to be the strongest predictor of future malignant transformation in potentially malignant disorders.
- Grading of epithelial dysplasia is divided into three categories:
Mild: Cellular atypia and architectural disturbances limited to basal and parabasal layers.
Moderate: Cellular atypia and architectural disturbances limited from basal to midportion of spinous cell layer.
Severe: Cellular atypia and architectural disturbances from basal layer to a level above midpoint of epithelium.
Carcinoma in situ: Theoretical concept of carcinoma in situ is that malignant transformation has occurred but invasion is absent.
This is the most severe form of epithelial dysplasia and involves entire thickness of epithelium.
This is cytologically similar to squamous cell carcinoma but architecturally the epithelial basement membrane remains intact and no invasion in connective tissue has occurred.
Question.32. Write short note on neurilemmoma.
Answer. It is also known as schwannoma.
It is a benign neural neoplasm of Schwann cell origin.
Clinical Features
- The lesion occurs most commonly in young and middle age adults.
- Neurilemmoma is a slow growing encapsulated tumor which arises in association with nerve trunk.
- Usually the tumor mass is asymptomatic, but tenderness or pain is present if tumor is causing pressure in associate nerves.
- Tumor may range from few millimeters to several centimeters in size.
Oral Manifestations
- It occurs commonly in oral cavity and the most common site of occurrence is tongue.
- The lesion is a single, circumscribed nodule of varying size which presents no pathognomonic features.
- Neurilemmoma also occur as central lesion in the mandible and arises from mandibular nerve.
- Centrally occurring lesion may lead to destruction of bone with expansion of cortical plates.
- Pain and paresthesia is common in centrally occurring lesions.
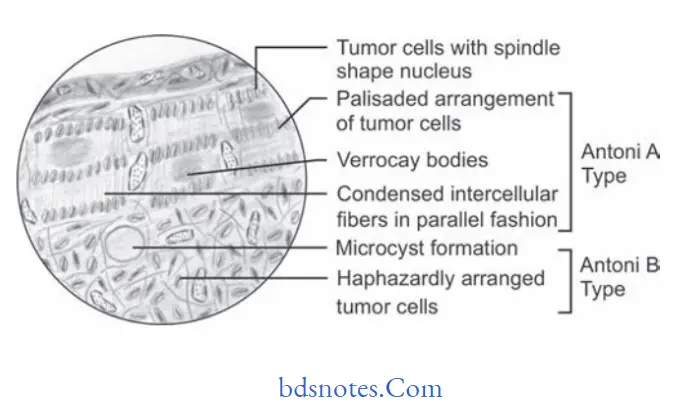
Histopathology
- Usually, the lesion presents two types of histologic patterns, i.e. Antoni A and Antoni B pattern.
- Antoni A: This pattern is made up of the cells which have spindle shape or elongated nuclei which are aligned to form a characteristic palisaded pattrn and the intercellular fiers are arranged in parallel fashion between rows of nuclei. In some areas, these fiers show arrangement in shape of whorls or swirls. In the palisaded arrangement of cells around central acellular area eosinophilic areas are seen known as Verocay bodies.
- Antoni B: In this pattrn, there is disordered arrangement of spindle cells and fiers in loose myxomatous stroma with areas of edema flid and formation of microcysts.
Treatment
Surgical excision is the treatment of choice.
Question.33. Enumerate the carcinomas of oral cavity. Describe staging and grading of squamous cell carcinoma.
Answer. Enumeration of carcinomas of oral cavity
- Squamous cell carcinoma
- Verrucous carcinoma
- Basaloid squamous cell carcinoma
- Adenoid squamous cell carcinoma
- Spindle cell carcinoma
- Adenosquamous carcinoma
- Undifferentiated carcinoma.
Staging of squamous Cell Carcinoma
Staging is defined as extent of spread of tumor within the body.
Staging of squamous cell carcinoma is done by TNM
classification which was given by American Joint Committee
on Cancer (AJCC)
T is suggestive of primary tumor
N is suggestive of regional lymph nodes
M is suggestive of distant metastasis
T primary tumor
TX Primary tumor cannot be assessed.
T0 No evidence of primary tumor
Tis carcinoma in situ
T1 Tumor 2 cm of less in greatest dimension
T2 Tumor more than 2 cm but not more than 4 cm in greatest dimension
T3 Tumor more than 4 cm in greatest dimension
T4a (Lip) Tumor invades through cortical bone, inferior alveolar nerve, flor of mouth or skin (chin or nose).
T4a (Oral Cavity) Tumor invades through cortical bone, intodeep/extrinsic muscle of tongue (genioglossus, hyoglossus,palatoglossus and styloglossus), maxillary sinus or skin of face.
T4b (lip and oral cavity) Tumor invades masticatory space,pterygoid plates or skull base or encases internal carotid artery
N Regional lymph nodes
NX Regional lymph nodes cannot be assessed
N0 No regional lymph node metastasis
N1 Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension.
N2a Metastasis in a single ipsilateral lymph node, more than3 cm but not more than 6 cm in greatest dimension.
N2b Metastasis in multiple ipsilateral lymph nodes, not more than 6 cm in greatest dimension.
N2c Metastasis in bilateral or contralateral lymph nodes, not more than 6 cm in greatest dimension.
N3 Metastasis in a lymph node more than 6 cm in greatest dimension.
M Distant Metastasis
MX Distant metastasis cannot be assessed
M0 No distant metastasis
M1 Distant metastasis.
Stage Grouping Of Oral Cancer

Grading Of Squamous Cell Carcinoma
- Grading is defined as macroscopic and microscopic degree of differentiation of a tumor.
- Squamous cell carcinoma is divided in following categories by Broder also known as Broder’s classification:
Broader’s Classification
- Grade I Well differentiated, – <25% undiffrentiated cells
- Grade II Moderately differentiated – <50% undifferentiated cells
- Grade III Poorly differentiated – <75% undifferentiated cells
- Grade IV Anaplastic/Pleomorphic – >75% undifferentiated cells
Question.34. Write short note on radiological features of osteosarcoma.
Answer. The radiographic features of osteosarcoma are divided into following stages, i.e.
- Osteolytic Stage
- It reveals moth eaten appearance.
- Border of the lesion at this stage are ill defied.
- There is perforation and expansion of cortical plates.
- Lamina dura is absent, i.e. it get destroyed.
- Pathological fracture may be present.
- Root resorption is present.
- Mixed Stage
- It is called as mixed because this stage shows formation and destruction of bone.
- It reveals honeycomb appearance.
- Margins of lesion are ill defied.
- Osteoblastic Stage
- It reveals sun ray appearance.
- At times subperiosteal bone laid down in layers which results in onion peel appearance.
- In osteosarcoma periosteum is elevated over the expanding tumor mass in a tent like fashion.
At point on the bone where the periosteum begin to merge an acute angle between periosteum and bone is created which is known as Codman’s Triangle.
Question.35. Write short note on papilloma.
Answer. Papilloma is the benign proliferation of stratified squamous epithelium which result in papillary and verruciform mass.
Etiology
Papilloma is caused by human papilloma virus. Viral subtypes 6 and 11 are identified in 50% of oral papillomas.
Mode Of Transmission
Exact mode of transmission is unknown but transmission is by sexual and nonsexual person to person contact, contaminated objects, saliva or breast milk.
Clinical Features
- Papilloma can be diagnosed at any stage but more commonly it is seen in persons of 30 to 50 years of age.
- Papilloma occurs more commonly on tongue, lip and soft palate but it can involve any of the surface.
- Papilloma is a soft, painless usually pedunculated, exophytic nodule with numerous figer like projections which impart cauliflwer or wartlike appearance.
- Lesion can be white, slightly red or normal in color depend on surface keratinization.
- Papilloma remains solitary and enlarges to the maximum size of 0.5 cm but lesions of 3 cm are also reported.
Histopathology
- Papilloma is characterized by proliferation of keratinized stratifid squamous epithelium which is arranged in figer like projections along with the fibrovascular cores.
- Its hallmark feature is proliferation of spinous cells in papillary pattrn.
- Connective tissue core can show inflammatory changes.
Presence of chronic inflammatory cells can be variably noted in connective tissue. - Koilocytes, i.e. virus altered epithelial clear cells with small dark or pyknotic nuclei with perinuclear clear spaces are sometimes seen in prickle cell layer.
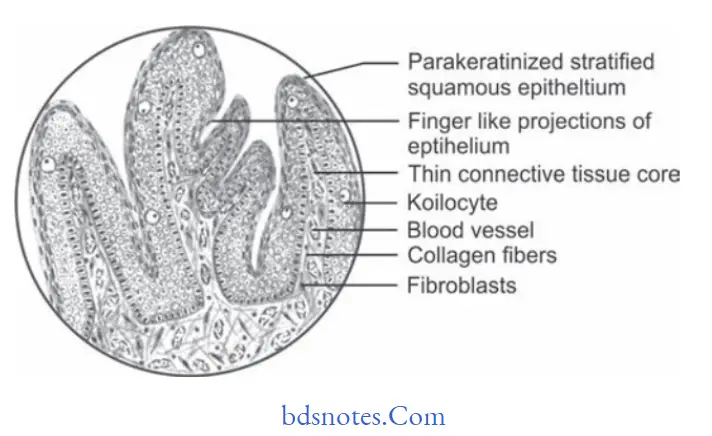
Treatment
Surgical excision should be done including the base of lesion.
Question.36. Write short note on Ewing’s sarcoma.
Answer. Ewing’s sarcoma is a small round cell tumor. It arises inside the bone.
Clinical Features
- It occurs predominantly in children and young adults between 5 to 25 years with median age of 13 years.
- It is more common in males as compared to females.
- Whites develop this tumor more commonly but in blacks not even single case is reported.
- Pain in Ewing’s sarcoma is intermittnt in nature.
- Swelling of the bone is earliest clinical sign.
- Long bones of extremities are more commonly affcted besides these skull, clavicle, ribs, shoulder are also affcted.
- Ewing’s sarcoma in occur more commonly in mandible as compared to maxilla
- Paresthesia and loosening of teeth are common fidings in Ewing’s sarcoma of jaw.
- Appearance of jaw swelling is rapid and intraoral mass become ulcerated.
- Tumor commonly penetrates the cortex resulting in soft tissue mass which overlie affected area of bone.
Radiographic Features
- Most common fiding is formation of layers of new subperiosteal bone which produces onion skin appearance of fim.
- There is presence of irregular lytic bone destruction with ill-defied margins.
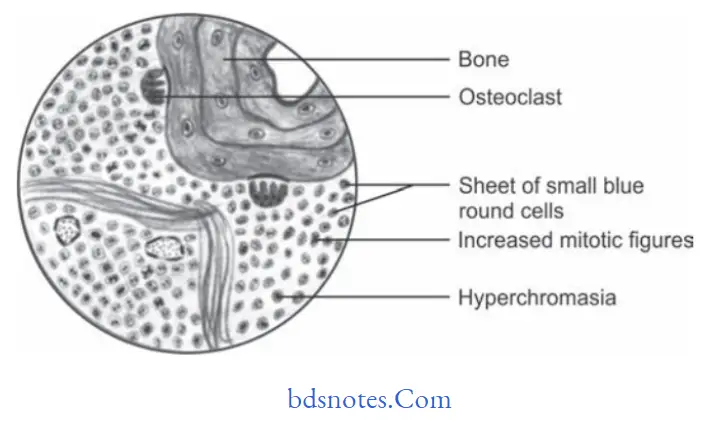
Histopathology
- Ewing’s sarcoma is highly cellular which consists of solid sheets or mass of small round cells with litte stroma, few connective tissue septa can also be seen.
- Cells are small and round in shape having scanty cytoplasm. Nuclei of cell is large round to oval in shape with dispersed chromatin and hyperchromasia.
- Borders of cell are indistinct.
- Cells are arranged in filigree pattern.
- Mitotic figures are commonly seen.
- Multiple small vascular channels are also present.
- Hemorrhage with vascular lakes or sinuses can be seen.
- There is also presence of geographic necrosis with perivascular sparing.
- Necrosis can be seen on the opposite side of fragment of bone.
Histological Differential Diagnosis
- Small cell osteosarcoma
- Peripheral neuroectodermal tumor of infancy
- Metastatic neuroblastoma
- Mesenchymal chondrosarcoma
- Malignant lymphoma
- Embryonal rhabdomyosarcoma.
Treatment
- Radical surgical excision should be done alone or coupled with Xray radiation.
- Current treatment consists of combined surgery, radiotherapy and multidrug chemotherapy which led to 40 to 80% of survival rates.
Question.37. Write short note on features of epithelial dysplasia.
Answer. Following are the features of epithelial dysplasia:
Architecture And Cytologic Criteria For Grading Epithelial
Dysplasia Given by WHO (2005)
Architecture Criteria
- Irregular epithelial stratification
- Loss of polarity of basal cells
- Basal cell hyperplasia
- Dropshaped rete pegs
- Increased number of mitotic fiures
- Abnormally superfiial mitosis
- Dyskeratosis, i.e. premature keratinization in the cell
- Keratin pearls within rete ridges.
Cytologic Criteria
- Anisonucleosis: Abnormal variation in nuclear size
- Nuclear pleomorphism: Abnormal variation in nuclear shape
- Anisocytosis: Abnormal variation in cell size
- Cellular pleomorphism: Abnormal variation in cell shape
- Increased nuclear cytoplasmic ratio
- Increased nuclear size
- Atypical mitotic fiures
- Increase in the number and size of nucleoli
- Hyperchromatism.
Question.38. Write short note on multiple myeloma.
Answer. Multiple myeloma is a relatively uncommon malignancy of plasma cell origin which often has multicentric origin within the bone.
Pathogenesis
Mutation of terminally differentiated B cells or early committd B cells lead to more differentiated plasma cells.
Abnormal plasma cells probably arising from single malignant precursor which had undergone uncontrolled mitotic division and spreads throughout the body.
Since the neoplasm develops from the single cell, all daughter cells which comprises of the lesional tissue have same genetic makeup and produce same proteins.
Clinical Features
- It occurs between 40 to 70 years of age.
- Male to female ratio is 4:1.
- Bone pain is present particularly in the lumbar spine.
- Pathological fractures are also present.
- Petechial hemorrhages of skin can be seen.
- Swelling over the areas of bony involvement can be seen.
- Metastatic calcifiation may involve the soft tissue and is due to hypercalcemia secondary to tumor related osteolysis.
- Amyloid deposits occur at periorbital region appearing waxy, fim, plaque like lesions.
- Death occurs due to renal failure as there is accumulation of abnormal proteins in renal tissue.
Oral Manifestations
- Mandible is commonly involved as compared to maxilla.
Angle of mandible is commonly involved. - Patient complaints of pain, numbness and swelling of jaw.
- Intraoral swelling is present which tends to be ulcerated,rounded and bluish red.
- Tongue may show diffuse enlargement and firmness or may have nodular appearance. Sometimes nodules are ulcerated.
Radiographic Features
Presence of multiple well defied, punched out radiolucency or ragged radiolucent lesions. This is evident on skull radiograph.
Laboratory Investigations
- Urinary examination: Light chain products found in urine of 30 to 50% of multiple myeloma patients are known as Bence Jones proteins.
- On serum protein electrophoresis most patients suffering from multiple myeloma have decreased quantity of normal immunoglobulin and an abnormal monoclonal immunoglobulin protein peak, known as M spike. The immunoglobulin is usually of IgG or IgA class with monoclonal light chain component.
- Alkaline phosphatase levels are raised.
Histopathology
- There is presence of sheets of closely packed cells resembling plasma cells. Cells are round to oval in shape with eccentrically placed nucleus exhibiting chromatin clumping in cartwheel or checkerboard pattrn.
- Perinuclear halo can also be seen.
- Russell bodies are seen in chronic inflmmatory lesions with numerous typical plasma cells.
- Mitotic activity can be seen along with some frequency.
- If amyloid is present, it appears as homogenous, eosinophilic and relatively acellular.
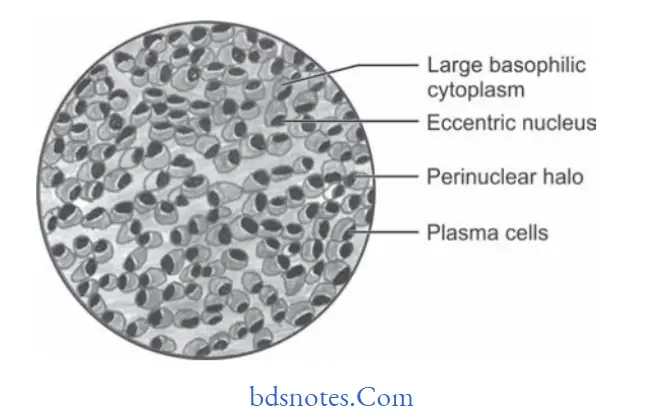
Treatment
- Multiple myeloma is treated by chemotherapeutic agents such as melphalan and cyclophosphamide along with prednisolone.
- Oral bicarbonates, high flid intake and corticosteroid decreases calcium levels.
- Local radiation therapy decreases painful bony lesions.
Question.39. Write short note on pathogenesis of oral submucous firosis.
Answer. Basically, pathogenesis of OSMF consists of disturbance in collagen metabolism via TGF β. The whole procedure is described as:
Initial Event Of Disease Process
According to P.Rajalitha, S.Vali (2005) initial event of the disease process is, oral mucosa which is in direct contact with betel quid (tobacco + areca nut + slaked lime + catechu and condominents) because of the habit which is the meAns of constant irritation.
Major areca nut alkaloids are arecoline,arecaidine, arecolidine, guacoline and guacine. Out of all these arecoline is most abundant.
These alkaloids undergo nitrosation and give rise to N nitrosamines which have cytotoxic effects on cells.
Important flvonoid components of areca nut are tannins and catechins.
So all these alkaloids,flvonoids and microtrauma produced by friction of coarse fiers of areca nut leads to chronic inflammatory process which is characterized by presence of inflammatory cells, i.e.
T cells and macrophages, these cells release and/or stimulate synthesis of various cytokines and growth factors.
Increased susceptibility among individuals who are anemic due to iron or vitamin B12 deficiencies.
It is because of increased fragility of mucosa by which there is more betel quid absorption.
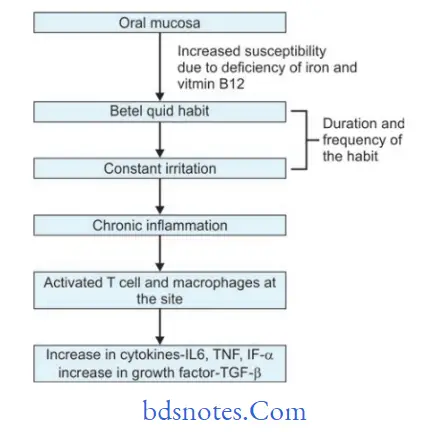
Collagen production pathway as regulated by tgF β
Transforming growth factor-β (TGF–β) is a growth factor which regulate the collagen production pathway, it has autocrine activity.
TGF–β activate procollagen genes which lead to production of more procollagen.
TGF–β also increases secretion of procollagen C proteinase (PCP) and procollagen N proteinase (PNP) both of these are needed for conversion of procollagen to collagen fibrils.
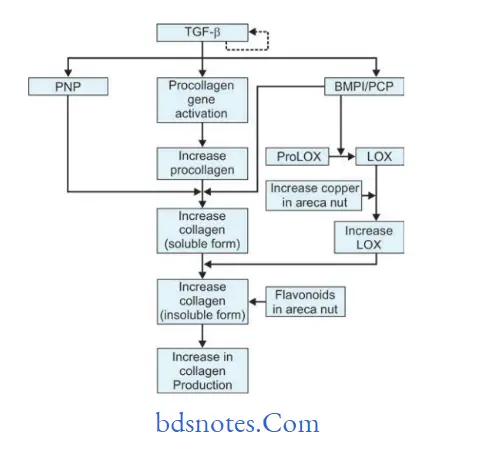
In oral submucous fibrosis, there is increase in cross linking of collagen which results to increase in insoluble form.
This is facilitated by increased activity and production of key enzyme Lysyl oxidase (LOX).
PCP and bone morphogenetic protein 1 and increased copper in betel quid stimulate the activity of LOX which produces increase collagen which is insoluble.
Flavonoids increases the cross linking of collagen fiers. These all steps lead to increase in collagen production.
TGF β strongly promote the expression of LOX both at mRNA and protein levels in various cell lines.
LOX activity is important in formation of insoluble collagen due to cross-linking.
Process of cross linking provides tensile strength and mechanical properties to fiers as well as makes collagen fiers resistant to proteolysis.
Collagen Degradation pathway as regulated by tgF–β
There are also two main events modulated by TGF–β which also decreases collagen degradation, i.e. activation of tissue inhibitor of matrix metalloproteinase gene (TIMPs) and activation of plasminogen activator inhibitor (PAI) gene.
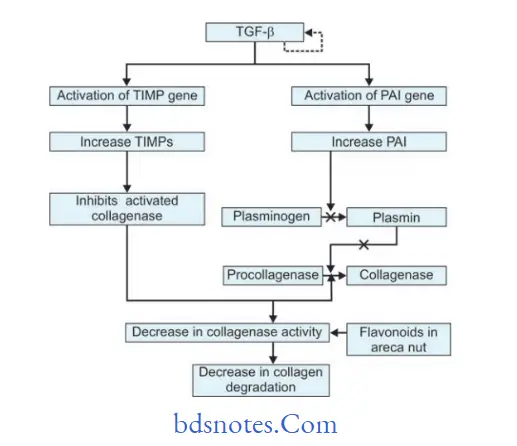
Collagen degradation pathway as regulated by TGF-β activates genes for TIMPs and so more TIMP is formed.
Now this inhibit activated collagenase enzyme which is necessary for degradation of collagen.
It also activate genefor PAI which is the inhibitor of plasminogen activator,so there is no plasmin formation.
Plasmin is needed for the conversion of procollagenase to active form of collagenase and absence of plasmin lead to absence of active collagenase.
Flavonoids inhibit collagenase activity.
Reduction in activity and levels of collagenase result in decrease in collagen degradation.
Overall Effect Of TgF–Β Pathway
So, overall effect of activated TGF–β pathway is that there is an increase in collagen production and crosslinking (insoluble form) along with decrease in collagen degradation.
This produces an increased collagen deposition in subepithelial connective tissue layer of oral mucosa causing oral submucous fibrosis.
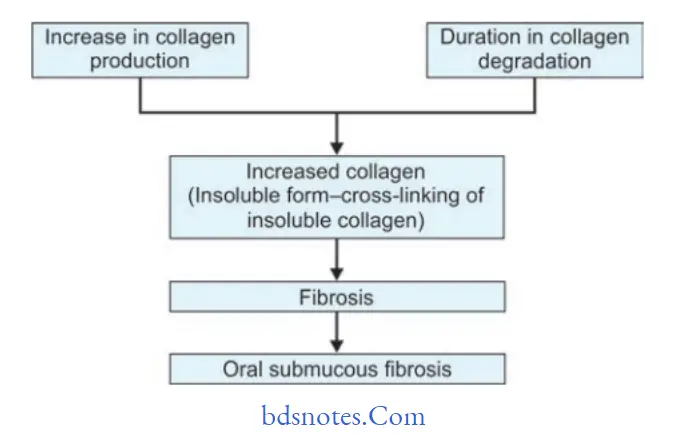
Question.40. Write short note on histopathology of oral submucous firosis.
Answer. Following is the common histopathological features of oral submucous fibrosis:
- Overlying hyper keratinized or atrophic epithelium often shows flttning and shortening of rete pegs.
- There can be variable degrees of cellular atypia or epithelial dysplasia.
- In OSMF dysplastic changes are found in epithelium which include nuclear pleomorphism, sever intercellular edema, etc.
- Stromal blood vessels are dilated and congested and there
can be areas of hemorrhage. - Underlying connective tissue stroma in advanced stage of disease shows homogenization and hyalinization of collagen fiers.
- Decreased number of firoblastic cells and narrowing of blood vessels due to perivascular firosis are present.
- There can be presence of signet cells in some cases.
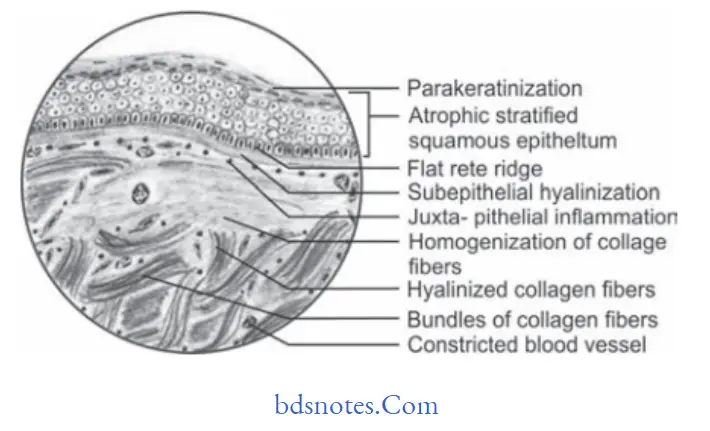
Histopathology Based On Various Types Of OSMF
Khanna JN and Andrade NN in 1995 given the group classification system for OSMF which consists of various groups of OSMF and their clinical and histological aspect. So following are the histological aspects as per the OSMF group:
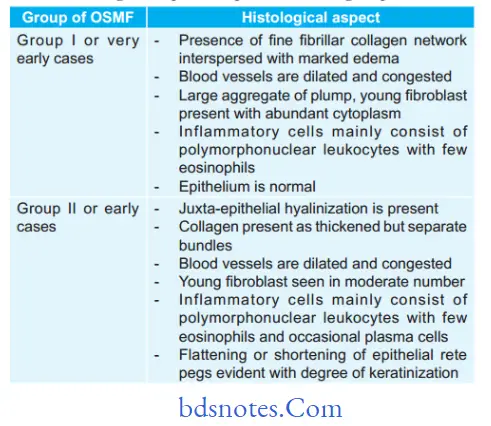
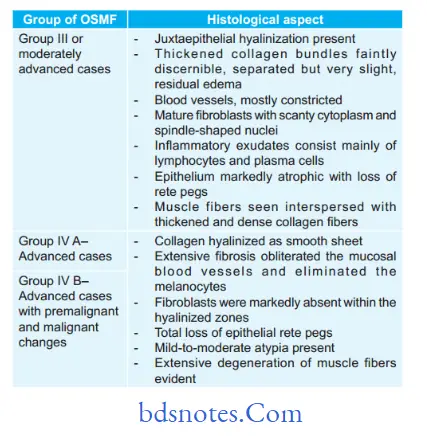
Question.41. Write short note on lymphangioma.
Answer. Lymphangioma is a benign hamartomatous tumor of lymphatic vessels.
Lymphangioma is thought to be developmental malformation of vessels which have poor communication with normal lymphatic system.
Types
Following are the types of lymphangiomas:
- Lymphangioma simplex or capillary lymphangioma: It consists of small thin walled capillaries.
- Cavernous lymphangioma: It consists of dilated lymphatic vessels with surrounding adventitia.
- Cystic lymphangioma or cystic hygroma: It consists of large,macroscopic cystic spaces with surrounding firovascular tissue and smooth muscle.
- Benign lymphangioendothelioma: In this lymphatic channels appear dissecting through dense collagen bundles.
Clinical Features
- Lymphangioma occur more commonly on head and neck.
- Cervical lymphangiomas are common in posterior triangle and are soft as well as flctuant masses.
Oral Manifestations
- Most commonly lesion occurs on tongue and also seen on palate, buccal mucosa, gingiva and lips.
- Superficial lesions occur as papillary lesions which are ofsame color to surrounding mucosa or can be of red hue.
- Deep lesions appear as diffse nodules or masses.
Secondary hemorrhage in lymphatic spaces can cause some of vesicles to appear purple. - Tongue involvement results in increase in size of tongue,i.e. macroglossia. Anterior dorsal part of tongue is commonly affcted.
- Lip involvement can lead to macrocheilia.
- Small lymphangiomas are less than 1 cm in size and occur on alveolar ridge of black neonates.
Histopathology
- Lesion shows multiple, intertwining lymph vessels in loose firovascular stroma.
- Cavernous type show many dilated lymphatics with singlelayer of endothelial cells with flt nuclei and having lymph.
- Vessels which lie beneath surface epithelium replace connective tissue papillae and produce papillary surface change. This appears as translucent vesicle like clinical appearance.
- At times channels can be filed with blood which is known as hemangiolymphangioma.
- At times channels demonstrate proliferation of lymphatic channels with smooth muscle cells known as lymphangiomyoma.
- Cystic hygroma shows cyst like structures.
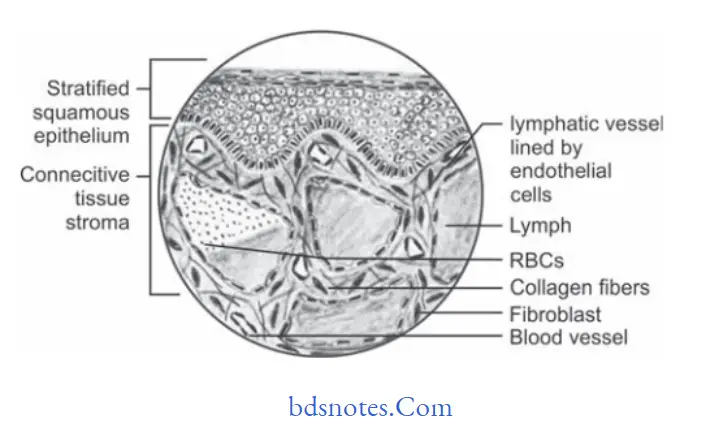
Treatment
- Surgical removal should be done.
- Complete removal is impossible.
- Surgical debulking is the typical treatment provided.

Leave a Reply