Arterial Diseases
Question 1. Write in short on Burger’s disease.
Answer. It is also known as thromboangiitis obliterans or smoker disease.
A chronic recurring, inflammatory, vascular occlusive disease, chiefly of the peripheral arteries and veins of the extremities.
Burger’s Disease Classification
- Type I- Upper limb thromboangiitis obliterans.
- Type II- Involving leg and feet – crural/infrapopliteal
- Type III- Femoropopliteal
- Type IV- Aortoiliofemoral
- Type V- Generalized.
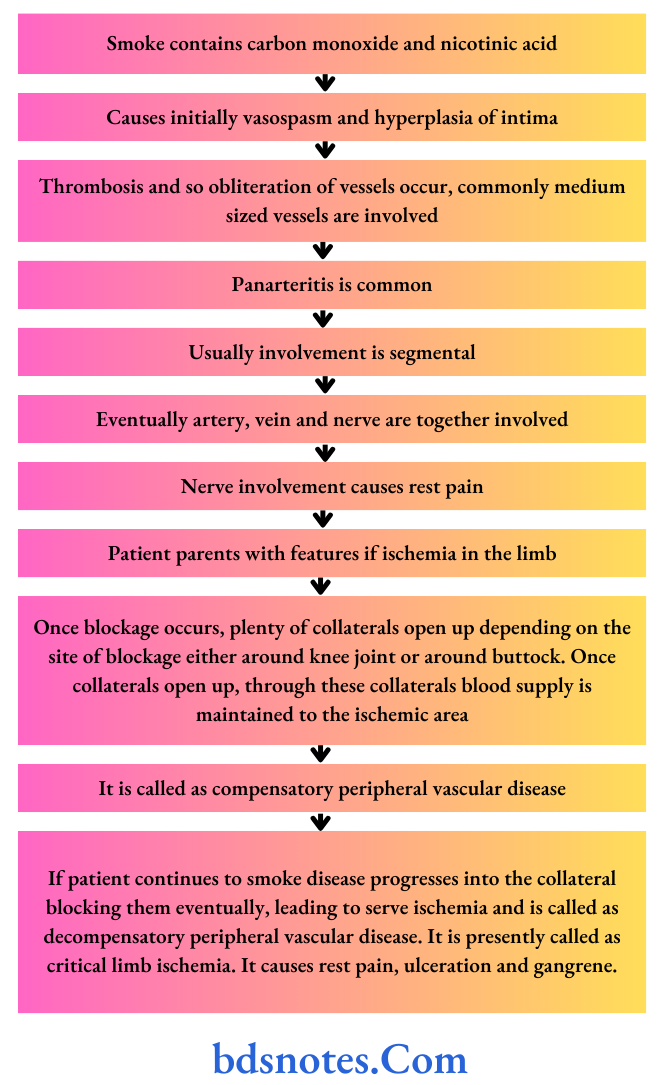
Burger’s Disease Pathogenesis
Read And Learn More: General Surgery Questions and Answers
Burger’s Disease Clinical Features
- It is common in male smokers between 20 to 40 years of age.
- Intermittent claudication in foot and calf progressing to rest pain, ulceration, and gangrene.
- It includes paresthesia of the foot or pain confined to one toe.
- Easy fatiguability and leg cramps. The leg fatigue quickly especially during walking.
- Ulceration or moist gangrene of hands and feet; amputation may be necessary.
- Recurrent migratory superficial thrombophlebitis
- Absence/Feeble pulses distal to proximal; dorsalis pedis, popliteal and femoral arteries.
Burger’s Disease Diagnosis
Burger’s Disease Criteria of Olin (2000)
- It occurs typically between 20 and 40 years of age in males, although females are also diagnosed.
- History of tobacco use.
- Presence of distal extremity ischemia indicated by claudication, pain at rest, ischemic ulcers, or gangrene. This is documented by noninvasive vascular testing, i.e. ultrasound.
- Exclusion of other autoimmune diseases such as hypercoagulable states and diabetes mellitus by laboratory tests.
- Exclusion of proximal source of emboli by echocardiography and arteriography.
- Consistent arteriographic findings in clinically involved and non-involved limbs.
No laboratory test should confirm the diagnosis of Burger’s disease.
The main goal of various investigations is to exclude other diseases in differential diagnoses.
Burger’s Disease Treatment
Smoking is strictly stopped.
Burger’s Disease Drugs
- Vasodilators, i.e. nifedipine should be given.
- Pentoxifylline should be given since it increases the flexibility of RBCs so they reach easily in microcirculation.
- Aspirin 75 mg OD is given.
- Analgesics, often sedatives, and antilipid drugs like atorvastatin may be needed.
Burger’s Disease Care of the Limbs
Buerger’s position and exercise: Regular graded exercises up to the point of claudication improve the collateral circulation.
In Buerger’s position, the head end of the bed is raised; the foot end of the bed is lowered to improve circulation. In Buerger’s exercise leg is elevated and lowered alternatively, each for 2 minutes several times at a time.
Care of feet: It is better to wear socks with footwear. Heel raise by raising the heels of shoes by 2 cm decreases the calf muscle work to improve claudication.
Burger’s Disease Chemical Sympathectomy
The sympathetic chain is blocked to achieve vasodilatation by injecting a local anesthetic agent (xylocaine 1%) paravertebrally beside the bodies of L 2, 3, and 4 vertebrae in front of lumbar fascia, to achieve temporary benefit.
Long-term efficacy can be achieved by using 5 mL phenol in water.
It is done under C-Arm guidance. The feet will become warm immediately after injection.
Burger’s Disease Surgery
- Omentoplasty to revascularize the affected limb.
- Profundaplasty is done for blockage in profunda femoris artery to open more collaterals across the knee joint.
- Lumbar sympathectomy to increase the cutaneous perfusion to promote ulcer healing. But it may divert blood from muscles towards the skin causing muscles more ischemic.
- Amputations are done at different levels depending on the site, severity, and extent of vessel occlusion. Usually either below—knee or above-knee amputations are done.
- Ilzarov’s method of bone lengthening helps in improving rest pain and claudication by creating neo-osteogenesis and improving the overall blood supply to the limb.
Question 2. Discuss briefly pressure sores.
Or
Discuss briefly bed (pressure) sores.
Answer. It is also known as decubitus ulcer pressure sores or Bedsores.
Pressure Sore Pathophysiology
Pressure sore occurs due to compression of issues by an external force.
Blood flow to the skin stops as external pressure becomes more than 30mm of Hg which causes ischemia. Ischemia causes inflammation and tissue anoxia.
Tissue anoxia leads to cell death, necrosis, and ulceration.
Pressure Sore Clinical Features
- It is a trophic ulcer with bone as a base.
- It is a non-mobile, deep, punched-out ulcer.
- It is commonly seen in old age bedridden patients, tetanus, orthopedic
- patients, diabetics, and patients with head injuries.
Pressure Sore Sites affected
- Over the ischial tuberosity
- Sacrum
- In the heel
- About the head of the metatarsal
- Buttocks
- Over the shoulder
- Occiput
Pressure Sore Factors Causing Pressure Sore
- Normal stimulus to relieve pressure is absent in anesthetized patients.
- Nutritional deficiencies worsen necrosis
- Inadequate padding over bony prominences in malnourished patients
- Urinary incontinence in paraplegia patients causes skin soiling—maceration—infection—necrosis.
Pressure Sore Staging of Pressure Sore
- Non-blanching erythema—Early superficial ulcer
- Partial thickness skin loss—Late superficial ulcer
- Full-thickness skin loss extending into subcutaneous tissue but not through fascia—Early deep ulcer
- Full-thickness skin loss with fascia and underlying structures like muscle, tendon, bone, etc—Late deep ulcer
Pressure Sore Treatment
- The cause for pressure sore should be treated.
- Adequate nutritional supplementation should be done.
- Proper rest, antibiotics, slough excision, and regular dressings should be given.
- Vacuum-assisted closure: It is the creation of intermittent negative pressure of minus 125 mm Hg to promote the formation of healthy granulation tissue.
- Negative pressure reduces tissue edema, clears the interstitial fluid improves the perfusion, increases the cell proliferation and so promotes the healing.
- A perforated drain is kept over the foam dressing covered over the pressure sore.
- It is sealed with a transparent adhesive sheet.
- The drain is connected to the required vacuum apparatus.
- Once the ulcer granulates well, flip cover or skin grafting is done.
- Excision of the ulcer and skin grafting can also be done.
- Flaps—local rotation or other flps (transposition flps).
- Cultured muscle interposition should be done.
- Proper care should be given to the patient, i.e.
- Change in position once in 2 hours; lifting the limb upwards for 10 seconds once in 10 minutes
- Use of water bed/air bed/air-flid floatation bed and pressure dispersion cushions to the affected area.
- Urinary and fecal care
- Hygiene should be maintained
- Psychological counseling should be done.
- Regular skin observation; keeping skin clean and dry (using regular use of talcum powder); oil massaging of the skin and soft tissues using clean, absorbent porous clothing; control and prevention of sepsis helps in the management.
Question 3. Write a short note on gangrene.
Answer. Gangrene is a form of necrosis of tissue with superadded putrefaction.
Gangrene Etiology
- Trauma: Direct or indirect
- Infection: Boil, carbuncle, gas gangrene, Fournier’s gangrene, cancrum oris
- Physical: Burns, scald, frostbite, chemicals, irradiation and electrical
- Venous gangrene
- Secondary to arterial occlusion like atherosclerosis, emboli, diabetes,
- Raynaud’s disease, ergot.
Gangrene Clinical Features
- In gangrene, the organ involved is pale, gray, purple, and brownish-black. This is due to the disintegration of hemoglobin to sulfide
- Pulse is absent.
- There is a loss of sensation and function
- There is the presence of a line of demarcation between vital and dead tissue
. A band of hyperemia and hyperesthesia is present along with a developmental layer of granulation tissue.
Types Of Gangrene
Gangrene is of three types, i.e. dry, wet, and gas gangrene.
- Dry gangrene: It is a condition that results when one or more arteries become obstructed.
In this type of gangrene, the tissue slowly dies because of inadequate or no blood supply.
It happens mostly in the extremities and it develops in people with diabetes or arteriosclerosis. - Wet gangrene: It is a gangrene that develops as a complication of an untreated infected wound, caused by various bacterial infections.
The tissue is infected by saprogenic microorganisms, i.e. (C. perfringens, fusiform, etc.) which cause tissue to swell and emit a fetid smell. - Gas gangrene: It is a bacterial infection that produces gas within tissues. It is caused by bacterial exotoxins produced by Clostridium perfringens which are mostly found in soil and other anaerobes.
The infection spreads rapidly as the gases produced by bacteria expand and infiltrate healthy tissue in the vicinity. - Other gangrenes:
- Noma or cancrum oris is a gangrene of the face.
- Necrotizing fasciitis affects the deeper layers of the skin.
- Fournier gangrene usually affects the male genitals and groin.
Gangrene Investigations
- CBC, hemoglobin, and blood sugar
- Arterial Doppler, angiogram
- Ultrasonography of the abdomen to find out the status of the aorta
Treatment of Gangrene
Gangrene limb-Saving Method
- Drugs such as antibiotics, vasodilators, small doses of aspirin, and paraxylene are started.
- Care of feet and toes: Part ofthe feet or toe should be kept dry.
- Any injury has to be avoided
- Proper footwear is advised for the patient
- Pressure areas should be protected.
- If pus is present, it has to be drained.
- The limb should not be warmed.
- Diabetes should be controlled.
- Surgeries such as omentoplasty, profunda plasty, and arterial bypass graft are done to improve limb perfusion.
Gangrene Lifesaving Procedures
Amputations can be done as a lifesaving procedure.
- Below-knee amputation is a better option as the fi of the prosthesis is better and movements of the knee joint are retained.
In above-knee amputation range of movement is less and third support is required to walk.
Question 4. Write a short note on dry and wet gangrene.
Or
Write briefl on wet gangrene.
Or
Write short note on dry wet and gas gangrene.
Or
Write short answers on dry, wet, and gas gangrene.
Answer.
Dry Gangrene
- It is a condition that results when one or more arteries become obstructed.
- In this gangrene, the tissue slowly dies because of inadequate or no blood supply.
- It happens mostly in the extremities and it occurs in people with diabetes or arteriosclerosis.
It can also develop after prolonged exposure to freezing temperatures. - In dry gangrene tissue fist becomes bluish and the patient feels cold to the touch, As time progresses, a line of demarcation appears between the healthy and devitalized tissue, which becomes dry and dark black.
- Eventually, there may be a separation of the dead tissue from the living tissue; with spontaneous amputation (autoamputation) of the involved extremity.
- Treatment of this type of gangrene is aimed at improving circulation, and revascularization (i.e. restoration of blood to flow) to the affected area. This may be accomplished with drugs or through the surgical removal of the obstruction.
Wet Gangrene
- Wet gangrene is gangrene that develops as a complication of an untreated infected wound, caused by a certain bacterial infection.
- The tissue is infected by saprogenic microorganisms (C.perfringens, fusiformis, etc.) which cause tissue to swell and produce a fetid smell.
- This gangrene develops rapidly due to blockage of venous and/or arterial blood flow.
- In this affected part is saturated with stagnant blood, which promotes the rapid growth of bacteria.
- Toxic products formed by bacteria are absorbed causing the systemic manifestation of septicemia and finally death.
- Wet gangrene occurs in naturally moist tissue and organs such as the mouth, bowel, lungs, cervix, and vulva.
- Bedsores occurring on body parts such as the sacrum, buttocks, and heels—although not necessarily moist areas are also categorized as wet gangrene infections.
- The affected part is edematous, soft, putrid, rotten, and dark. The darkness in wet gangrene occurs due to the same mechanism as in dry gangrene.
- Administration of antibiotics and sometimes the surgical removal of the dead tissue to keep the infection from spreading is the treatment.
Gas Gangrene
- Gas gangrene is a bacterial infection that produces gas within tissues.
It is caused by bacterial exotoxins produced by Clostridium perfringens which are mostly found in soil and other anaerobes (e.g. Bacteroides and anaerobic streptococci). - The infection spreads rapidly as the gases produced by bacteria expand and infiltrate healthy tissue in the vicinity.
- After an incubation period of one to four or five days, the affected tissue is swollen, painful, and cold.
A watery, brownish, foul-smelling fluid drains from the wound and little bubbles of gas develop in the tissues. - Gas gangrene can cause necrosis, gas production, and sepsis. Progression to toxemia and shock is often very rapid.
- Gas gangrene is often treated with the antitoxin for Clostridium. In several cases. amputation may have to be used to keep the infection under control.
- Severe cases have been treated by keeping the patient in an oxygen-rich atmosphere, as in a hyperbaric chamber.
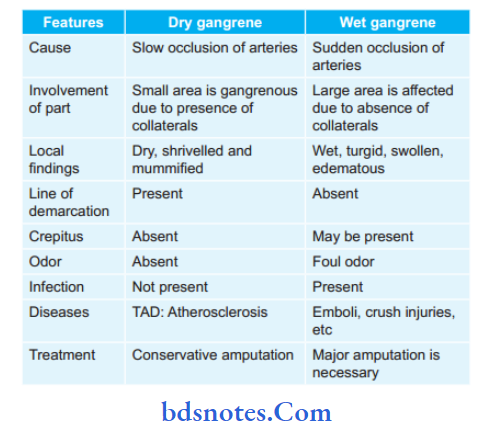
Question 5. Enumerate the differences between dry and wet gangrene.
Answer.
Question.6. Defie gangrene. Describe various causes of gangrene and management of diabetic gangrene foot.
Answer. Gangrene is the death of body tissue associated with loss of vascular supply and followed by bacterial invasion and putrefaction.
Gangrene Causes
- Secondary to arterial occlusion like atherosclerosis, emboli, diabetes, and Raynaud’s disease.
- Infective: Boil, carbuncle, gas gangrene, Fournier’s gangrene, cancrum oris
- Traumatic: Either direct trauma or indirect trauma
- Physical: Burns, scalds, frostbite, chemicals, irradiation, electrical
- Venous gangrene.
Management of diabetic Gangrene Foot
The foot can only be saved if a good blood supply is present.
- Antibiotics should be started based on culture and sensitivity tests.
- Regular dressings should be given to the patient
- Drugs such as vasodilators, pentoxifylline, dipyridamole, and low-dose aspirin are given.
- Diabetes is controlled by insulin
- The diet should be controlled
- Surgical debridement of the wound is carried out.
Gangrene lifesaving Procedures
Amputations of diabetic foot should be done occasionally.
- The level of amputation is decided based on skin changes, temperature, line of demarcation, and Doppler study.
- Below knee, amputation is done, in this BK prosthesis is fitted better and also the movements of the knee joint are retained.
- In the above-knee amputation range of movements is less, limb is present and requires third support to walk.
Gangrene Care of Feet and toes
- Part of the foot should be kept dry.
- Injury to the foot and toes is avoided
- Proper footwear is advised to the patient, i.e. microcellular rubber footwear
- Measures for pain relief are to be taken
- Nutritional supplementation is given
- Hyperkeratosis is avoided
- Localized pus should be drained
- The limb should not be warmed.
Question 7. Write a short note on diabetic foot.
Answer. Diabetic foot consists of callosities, ulceration, abscess, cellulitis of the foot, osteomyelitis of different bones, diabetic gangrene, and arthritis of joints.
Meggitt’s Classifiation of Diabetic Foot
- Grade 0: Foot symptoms like pain, only
- Grade l: Superficial ulcers
- Grade 2: Deep ulcers
- Grade 3: Ulcer with bone involvement
- Grade 4: Forefoot gangrene
- Grade 5: Full foot gangrene.
Pathogenesis of Diabetic Foot
- High glucose levels in tissues are a good culture medium for bacteria. So infection is common.
- Diabetic microangiopathy causes blockade of microcirculation leading to hypoxia.
- Diabetic neuropathy: Due to sensory neuropathy, minor injuries are not noticed and so infection occurs.
Due to motor neuropathy, dysfunction of muscles, arches of the foot, and joints occur.
And loss of reflexes of the foot occurs causing more prone to trauma and abscess.
Due to autonomic neuropathy, the skin will be dry causing a defective skin barrier and so more prone to infection. - Diabetic atherosclerosis: It reduces the blood supply and causes gangrene.
Thrombosis can be precipitated by infection-causing infective gangrene. Blockage occurs at plantar, tibial, and dorsalis pedis vessels. - Increased glycosylated hemoglobin in blood causes defective oxygen dissociation leading to more hypoxia.
At the tissue level, there will be increased glycosylated tissue proteins, which prevents proper oxygen utilization and so aggravates hypoxia.
Diabetic foot Clinical Features
- Pain in the foot
- Ulceration
- Absence of sensation
- Absence of pulsations in the foot (Posterior tibia and dorsalis pedis arteries).
- Loss of joint movements.
- Abscess formation
- Changes in temperature and color when gangrene sets in.
- Patients may succumb to ketoacidosis, septicemia, or myocardial infarction.
Diabetic foot Investigations
- Blood sugar, urine ketone bodies.
- Blood urea and serum creatinine.
- X-ray of a part to look for osteomyelitis.
- Pus for culture and sensitivity.
- Doppler study of the lower limb to assess arterial patency.
- Angiogram to look for proximal blockage.
- Ultrasound of the abdomen to see the status of the abdominal aorta.
- Glycosylated hemoglobin estimation.
Diabetic foot Treatment
- The foot can be saved if only there is a good blood supply:
- Antibiotics—decided by pus culture and sensitivity
- Regular dressing
- Drugs: Vasodilators, pentoxifylline, dipyridamole, low-dose aspirin.
- Diabetes is controlled by insulin only.
- Diet control, control of obesity.
- Surgical debridement of the wound.
- Amputations of the gangrenous area. The level of amputation has to be decided by skin changes and temperature changes or Doppler study.
- Care of feet in diabetic:
- Any injury has to be avoided.
- MCR footwear must be used (Microcellular rubber)
- Feet has to be kept clean and dry, especially toes and clefts
- Hyperkeratosis should be avoided.

Leave a Reply