Antihypertensive Drugs
Question 1. Write Classification And Uses Of Antihypertensive Drugs.
Answer:
Classification Of Antihypertensive Drugs
- ACE inhibitors: Captopril, enalapril, lisinopril, perindopril, ramipril, lisinopril, benazepril and fosinopril
- Angiotensin antagonist: Losartan, candesartan, irbesartan, valsartan, telmisartan
- Calcium channel blockers: Verapamil, diltiazam, nifedipine, felodipine, amlodipine
- Diuretics
- Thiazides: Hydrochlorthiazide, chlorthalidone, indapamide
- High ceiling: Furosemide, bumetanide, torsemide
- K+ sparing: Spironolactone, Amiloride, triamterene
- Beta adrenergic blockers: Propranolol, atenolol, temolol, nadolol
- Beta + Alpha-adrenergic blockers: Labetalol, carvedilol
- Alpha adrenergic Blockers: Prazosin, terazosin, doxazosin, phentolamine, phenoxybenxamine
- Central sympatholytics: Clonidine and methyldopa
- Vasodilators
- Arteriolar: Hydralazine, minoxidil and diazoxide
- Arteriolar + Venous: Sodium nitroprusside.
Read And Learn More: Pharmacology Question And Answers
Antihypertensive Drugs Uses
- Antihypertensive drugs such as ACE inhibitors preload and afterload in CHF.
- An antihypertensive drug such as calcium channel blockers is useful in the treatment of angina pectoris.
- The calcium channel blockers are also useful in the treatment of arrhythmias, Raynaud’s disease, and in the prevention of neurological damage.
- Antihypertensive drugs such as hydralazine act as vasodilators and causes fall in BP.
- Antihypertensive drugs mainly ACE inhibitors improve renal functions in diabetes.
Question 2. Discuss Calcium Channel Blockers.
Or
Write Short Note On Calcium Channel Blockers.
Answer:
There are three subclasses of calcium channel blockers:
- Phenylalkylamines: Verapamil
- Benzothiazepines: Diltiazam
- Dihydropyridines: Nifedipine, amlodipine nicardipine, pelodipine, isradipine, nisoldipine.
Calcium Channel Blockers Mechanism Of Action
- Smooth muscle relaxants: The movement of calcium inside cardiac muscle cells released more calcium from the sarcoplasmic reticulum causing excitation-contraction coupling.
- Calcium channel blockers block all types of calcium channels and decrease the availability of calcium ions thus causing the relaxation of smooth muscle cells or cardiac cells. The effect is more on arterioles and less on veins.
Negative, Chronotropic, Ionotropic And Dromotropic Action
- Calcium channel blockers inhibit calcium movement inside the cell in the depolarization phase thus inhibiting the contraction of cardiac muscle. Cardiac work and oxygen consumption are decreased.
- Calcium channel blockers inhibit the refractory period of the AV node, decrease SA nodal discharge suppresses ectopic foci producing Antiarrhythmic action.
Uses Of Calcium Channel Blockers
- Angina pectoris: It is useful in both types of angina, i.e. classical and variant angina.
- Hypertension: They are fist line drugs in hypertension. Calcium channel blockers decrease total peripheral resistance and hence decrease BP.
- Arrhythmias: Calcium channel blockers are preferred in supraventricular tachycardia.
- Calcium channel blockers are also used in hypertensive emergencies.
- Hypertrophic cardiomyopathy: Verapamil improves diastolic function.
- Migraine: Flunarizine reduces the frequency of migraine attacks. Verapamil is used as a prophylactic drug.
Question 3. Write On Nifedipine As Antihypertensive.
Answer:
Nifedipine is a calcium channel blocker.
- It comes under the subclass of calcium channel blockers, i.e. Dihydropyridines.
- Nifedipine is a prototype drug.
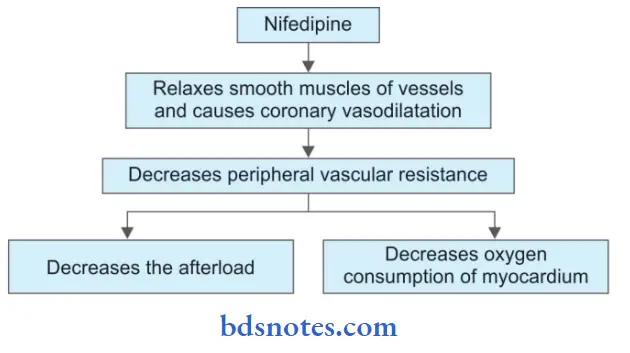
Nifedipine Mechanism of Action
Nifedipine Adverse Effects
Palpitation, flushing, ankle edema, hypotension, headache, drowsiness, nausea, reflux tachycardia, fatigue, dizziness, and sedation.
Nifedipine Uses
- Nifedipine is used in the treatment of Raynaud’s disease.
- It is an alternate drug for premature labor.
- It is used as a first-line drug for hypertension.
- It is used as an antianginal drug.
Question 4. Discuss Basis Of Verapamil In Paroxysmal Supraventricular Tachycardia.
Answer:
Paroxysmal supraventricular tachycardia is a sudden atrial tachycardia.
- It is a type of arrhythmia.
- In paroxysmal supraventricular tachycardia, the atrial rate is 150–200 minutes.
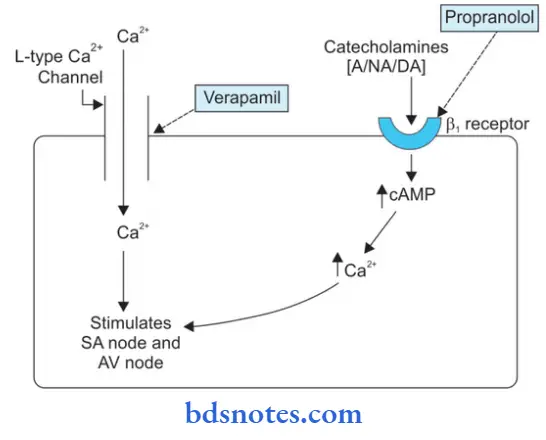
- Verapamil is a calcium channel blocker and lies in class IV of antiarrhythmic drugs.
Verapamil Mechanism of Action
Verapamil increases the repolarization of the AV node and decreases SA node discharge and suppresses ectopic foci due to this it undergoes antiarrhythmic action. So that’s why Verapamil is used in paroxysmal supraventricular tachycardia.
Question 5. Discuss Blood Vasodilator Drugs.
Answer:
Blood vasodilator drugs are of two types:
- Arteriolar: Hydralazine, Minoxidil, and Diazoxide
- Arteriolar + Venous: Sodium nitroprusside.
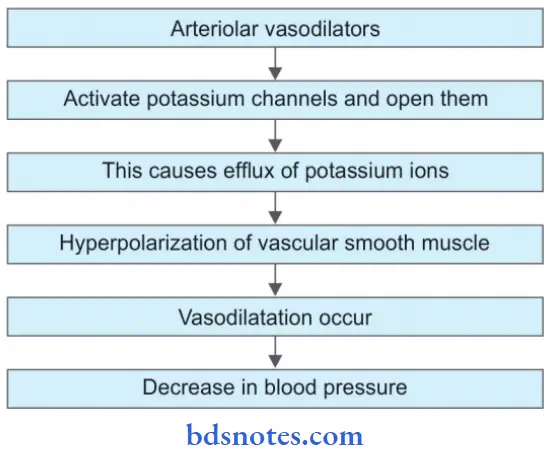
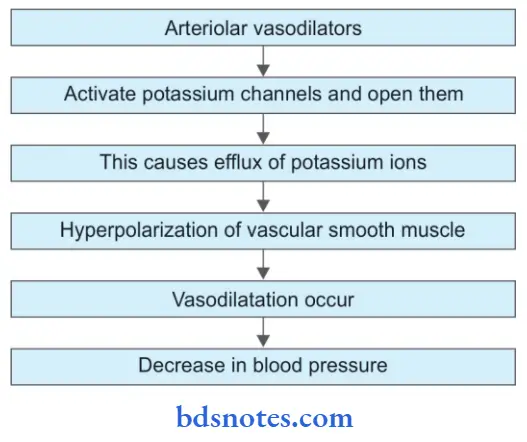
Mechanism Of Action Of Arteriolar Vasodilator
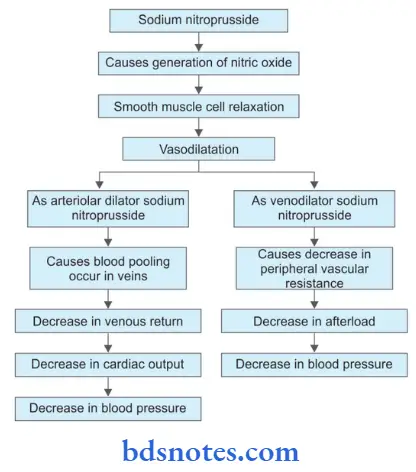
Mechanism Of Action Of Arteriolar + Venous Vasodilators
Blood Vasodilator Drugs Uses
- Vasodilator drugs are preferred antihypertensive drugs during pregnancy.
- They are used in moderate to severe hypertension when not controlled by first-line drugs.
- They are used in hypertensive emergencies.
Question 6. Discuss Diuretics In Hypertension.
Answer:
Diuretics as antihypertensive drugs are classified as:
- Thiazides: Hydrochlorthiazide
- High ceiling: Furosemide
- K+ sparing: Spirinolactone.
Diuretics Mechanism of Action
- Diuretics are weak antihypertensives
- Diuretics cause loss of sodium and water in urine due to which there is a decrease in cardiac output and hence a fall in BP.
- Due to direct loss of sodium, arterioles respond less to noradrenaline and hence less vasoconstriction and fall in BP.
Drawbacks Of Diuretics As Antihypertensives
- Hypokalemia: Muscle pain, impotence, and fatigue
- Proinsulin in the presence of potassium ions is converted to insulin so due to hypokalemia it precipitates diabetes.
- It increases cholesterol and triglycerides.
- It increases the chances of sudden cardiac death.
Diuretics Uses
- They are used for hypertension
- They are used in hypertensive emergencies.
Question 7. Write Briefl On β Receptor Blocker.
Or
Describe Briefly β (Beta)Blockers And Their Indications.
Or
Enumerate Important Indications, Contraindications, And Adverse Reactions Of β Blockers.
Or
Write A Short Answer On Contraindications To Use Of β Blockers.
Answer:
These drugs inhibit responses mediated by the adrenergic β blockers.
β Receptor Blocker Classifiation
- Cardioselective (β1): Metoprolol, atenolol, acebutolol.
- β2 selective: Butoxamine.
- Nonselective (β1+β2): Propranolol, nadolol, sotalol, timolol.
β Receptor Blocker Actions
- Heart: These drugs decrease the force of contraction, decrease AV conduction, decreases heart rate, and decrease automaticity of myocardial fibers thus cardiac output is decreased.
- Blood vessels: On prolonged administration BP falls in hypertensives.
- Respiratory system: It causes an increase in bronchoconstriction in asthmatics.
- Eye: β-blockers decrease aqueous humor secretion.
Adverse Effects And Contraindications
Adverse Reactions
- CVS: Bradycardia, heart block, and can precipitate heart failure.
- Respiratory system: These drugs can precipitate bronchial asthma.
- CNS: Disturbed sleep, fatigue, hallucination, and mental depression.
- Muscular weakness and tiredness.
- Abrupt withdrawal can cause angina or frank myocardial infarction.
Contraindications
- They are contraindicated in asthmatics and COPD.
- They are contraindicated in patients of print metal angina.
- They are contraindicated in peripheral vascular disease.
- They are contraindicated in patients with low cardiac reserve.
- They are contraindicated in diabetics who are taking oral antidiabetic drugs as they delay recovery from hypoglycemia.
Uses Or Indications Of β Blockers
- Hypertension: β blockers are used to treat all grades of hypertension. They are also indicated in angina, myocardial infarction, and cardiac arrhythmias.
- In the prophylaxis of angina and myocardial infarction: β blockers decrease the oxygen demand of the myocardium and decrease the heart rate. These drugs reduce the frequency of angina attacks. They are indicated in the acute phase of myocardial infarction so that they limit the size of the infarct.
- In cardiac arrhythmias: They are indicated in atrial arrhythmias, i.e. atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia.
- Congestive cardiac failure: Chronic usage of β blockers reduces the rate of mortality during chronic heart failure.
- Pheochromocytoma: These drugs control cardiac manifestations produced by pheochromocytoma.
- Glaucoma: They decrease intraocular pressure by decreasing the secretion of aqueous humor. Timolol is the choice of drug.
- In the prophylaxis of migraine: They decrease the frequency of migraine headaches.
- Hyperthyroidism: Signs and symptoms of hyperthyroidism decrease due to the blockade of β receptors.
- Essential tremors: Propranolol provides relief in tremors.
- Anxiety: It acts as an anti-anxiety drug.
- Alcohol withdrawal: Propranolol provides benefits for alcohol withdrawal.
- Dissecting aortic aneurysm: β blockers reduce cardiac contractility as well as the development of pressure during systole.
Question 8. Describe The Therapeutic Uses Of Propranolol.
Answer:
The therapeutic uses of propranolol are:
- Essential hypertension: Propranolol is used alone or can be combined with either a diuretic or α-adrenergic blocking drug. The fall in blood pressure, when used alone, is gradual and without postural hypotension.
- Ischemic heart disease: It decreases the workload on the heart, diminishes myocardial oxygen demand, and increases exercise tolerance; hence β-blockers benefit patients having angina of effort. The drug should be given continuously and not merely when an attack occurs.
- Myocardial infarction: β-blockers significantly decrease the incidence, recurrence, and mortality in cases of myocardial infarction after long-term use.
- Cardiac arrhythmias: Propranolol is effective in all supraventricular tachycardias associated with high levels of circulating catecholamines as occurs with the use of certain general anesthetics like halothane, in digitalis toxicity, pheochromocytoma, and thyrotoxicosis. The beneficial effect is mainly due to an increase in the refractory period of the AV node and direct membrane stabilizing action.
- Congestive cardiac failure: Propranolol should be introduced gradually and should be maintained for a long time. The drug has the tendency to retard the progression of congestive cardiac failure.
- Dissecting aortic aneurysm: It reduces the cardiac contractile force and aortic pulsation. It also reduces the rate of development of pressure at the time of systole.
- Pheochromocytoma: The drug in pheochromocytoma control cardiac manifestations such as tachycardia and arrhythmia.
- Hyperthyroidism: The drug controls the sign and symptoms produced due to hyperthyroidism without affecting the thyroid status.
- Anxiety: Propranolol has antianxiety effects and controls palpitation, tachycardia, tremor, sweating, etc.
- Essential tremors: Propranolol provides relief in cases with essential tremors.
- Glaucoma: It reduces intraocular pressure by decreasing the production of aqueous humor.
Question 9. Discuss The Management Of Hypertension.
Answer:
- Nonpharmacological methods which control hypertension are weight reduction, decrease in sodium intake, restriction of alcohol, physical
exercise, mental relaxation, smoking cessation, and taking a potassium-rich diet. - In pharmacological treatment, various factors, i.e. age, sex, cost of the drug, complications, etc. are helpful in the selection of an appropriate antihypertensive drug.
- Drugs used in the treatment of initial hypertension are ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, and thiazides.
- Treatment should be started with a single agent. Combination therapy should be applied to patients who do not respond to single-drug therapy.
- Below mentioned is the regimen for the treatment of hypertension.
It is administered in two types of people, i.e.
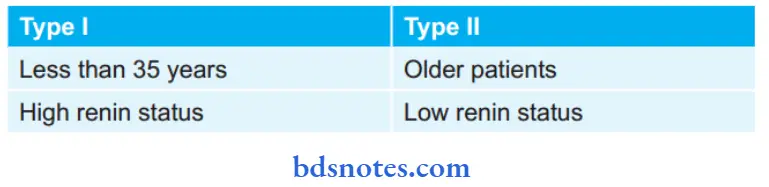
A (ACE inhibitor) C (Calcium channel Blocker)
Or Or
B (β blocker) D (Diuretics)
- If BP is not controlled then use a single drug from another group, i.e. A is replaced by C or B is replaced by D, or vice versa.
- If BP is still not controlled then two drug regime is started, i.e. one drug from the first group and another drug from the second group, i.e. A + C or A + D
- Finally, A + B or C + D can be tried but it has less additive effect on BP.
- B + C is contraindicated: Produces cardiac depressant action.
- If BP is still not controlled then use a triple-drug regime.
- A + C + D is ideal regimen.
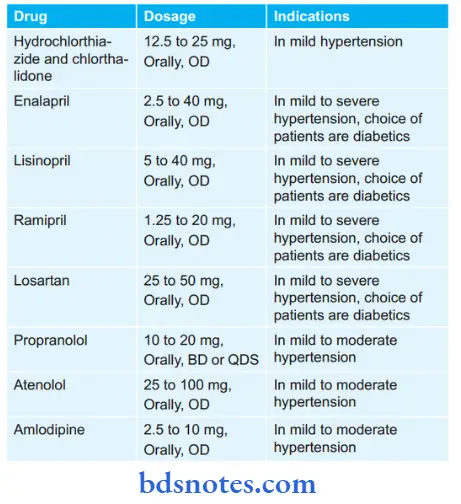
Various Dosages Along With The Indications Of Antihypertensive Drugs
Question 10. Discuss Drugs In Hypertensive Crisis.
Answer:
Hypertensive crisis is of two types, i.e. hypertensive urgency and hypertensive emergency.
Hypertensive Urgencies
This is due to:
- Severely elevated BP, i.e. (200/120)
- Absence of organ damage.
Hypertensive Crisis Treatment
There is a slow reduction of blood pressure over 12 hours with oral antihypertensive, e.g. labetalol, nifedipine, etc.
Hypertensive Emergencies
The hypertensive emergencies are due to:
- Severely elevated BP
- Ongoing organ damage.
Hypertensive Crisis. Treatment
Quick reduction of BP is by parenteral agents, i.e. IV sodium nitroprusside, labetalol, etc.
Question 11. Describe The Drugs Used In Hypertensive Emergencies.
Or
Describe The Drugs Used In The Treatment Of Hypertensive Emergencies.
Answer:
The following are the drugs that are used in the treatment of hypertensive emergencies:
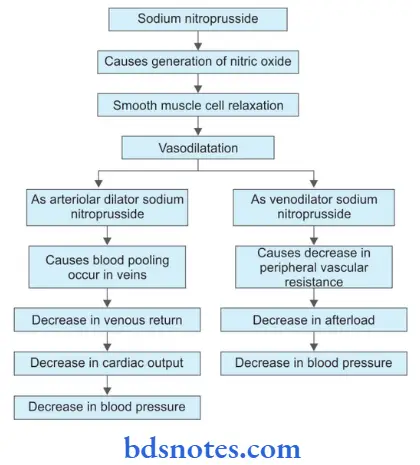
- Sodium nitroprusside: It is the drug of choice for most hypertensive emergencies. It has instantaneous, titrable, and balanced arteriovenous vasodilatory action. It needs an infusion pump and constant monitoring.
- Glyceryl trinitrate: It is given through IV infusion and it acts under 2 to 5 minutes. It has vasodilator action which makes it suitable for lowering blood pressure after cardiac surgery in acute left ventricular failure, myocardial infarction, and unstable angina.
- Esmolol: It is provided as a bolus which is followed by a slow IV injection which produces its action in 1 to 2 minutes. Its action last for 10 to 20 min. It is useful in cardiac contractility and when cardiac work is to be reduced.
- Phentolamine: It is an α1 + α2 blocker. It is mostly used in hypertensive episodes in pheochromocytoma, cheese reaction, and clonidine withdrawal.
Question 12. Discuss The Mode Of Action And Advantages Of A Combination Of Atenolol With Hydrochlorothiazide As An Antihypertensive Agent.
Answer:
Atenolol Mode Of Action
Since atenolol is a β-blocker it decreases the force of contraction, decreases AV node conduction, decreases heart rate, and decreases automaticity of myocardial fibers, thus cardiac work is decreased.
Hydrochlorothiazide is a diuretic so it decreases sodium water retention, decreases body fluid, decreases venous return, and decreases cardiac work but it is a weak antihypertensive drug.
Advantages Of Combination Of Atenolol And Hydrochlorothiazide
Hydrochlorothiazide is a weak antihypertensive and it potentiates the activity of atenolol in hypertension.
Hydrochlorothiazide has a compensatory effect on plasma renin activity because atenolol which is a β-blocker lowers the plasma renin activity and diuretic, i.e. hydrochlorothiazide increases plasma renin activity.
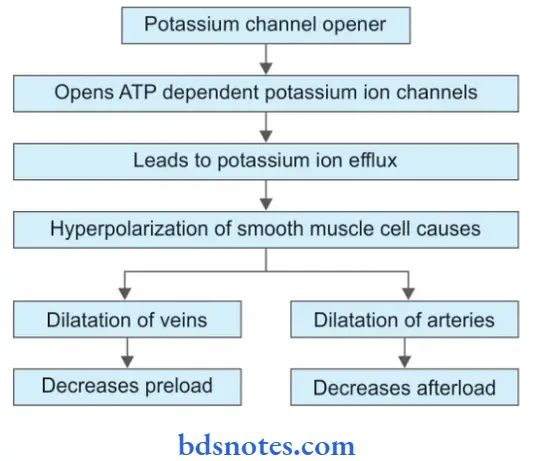
Question 13. Write The Basic Use Of Potassium Channel Opener In Hypertensive Emergency.
Answer:
The potassium channel opener used in hypertensive emergencies is nicorandil.
Question 14. Mention uses and drug action of antihypertensive drugs.
Answer:
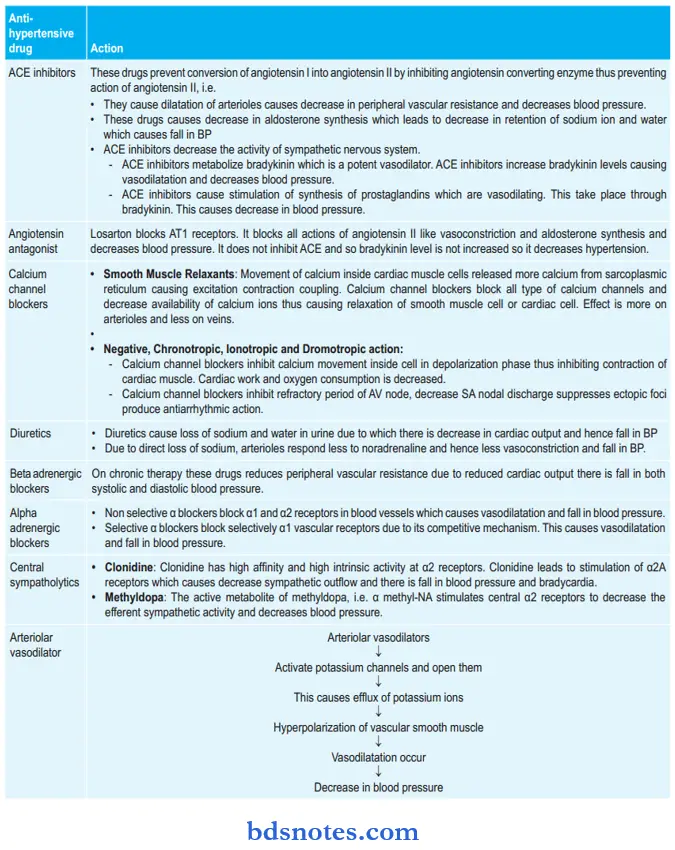
Drug Action Of Various Antihypertensive Drugs
Question 15. Discuss Hypertension Mode Of Action And Therapeutic Indications Of Atenolol.
Answer:
Atenolol is a selective beta blocker.
Hypertension Mode Of Action
Therapeutic Indications Of Atenolol
- In young hypertensive patients who have high renin levels.
- In patients with angina pectoris.
- In patients with postmyocardial infarction.
- In patients with migraine.
- In patients with psychosomatic disorders.
- It is indicated in patients who receive vasodilators to counteract reflex tachycardia.
- It is indicated to subside symptoms of alcohol withdrawal.
- It is also indicated to treat the symptoms of grave disease till anti-thyroid medication produces its effect.
Question 16. Explain The Pharmacological Basis For Beta Blockers In Hypertension And Angina Pectoris.
Answer:
Pharmacological Basis For Beta Blockers In Hypertension
When a beta blocker is administered total peripheral resistance is increased initially and cardiac output is reduced, so there is little decrease in blood pressure.
With continued treatment resistance vessels gradually adapt to chronically reduced cardiac output so that total peripheral resistance decreases and both systolic and diastolic blood pressure falls.
Pharmacological Basis For Beta Blockers In Angina Pectoris
Beta-blockers reduce cardiac work and oxygen consumption. Total coronary flow is reduced but this is largely restricted affected.
The main overall effect of beta blockers in angina pectoris is that these drugs improve oxygen supply/demand status and exercise tolerance is increased.
Question 17. Enumerate Therapeutic Uses Of Beta Blockers.
Answer:
Therapeutic Uses Of Beta Blockers
- Hypertension
- Angina Pectoris
- Cardiac arrhythmia
- Myocardial infarction
- Congestive heart failure
- Dissecting aortic aneurysm
- Pheochromocytoma
- Thyrotoxicosis
- Migraine
- Anxiety.
Question 18. Explain Why Selective Α1 Agonists Are Preferred Over NonSelective Α Blockers For Hypertension.
Answer:
Selective α1 blockers block selectively α1 vascular receptors by a competitive mechanism. They have no effect on α2 receptors so there is not any increase in the levels of noradrenaline due to which there is very less tachycardia while the non-selective α blockers block both α1 and α2 receptors.
So due to their blocking effect of α2 receptors, there is an increase in the release of noradrenaline due to which tachycardia is more. That’s why selective α1 agonists are preferred over non-selective α blockers in hypertension.
Question 19. Write Short Note On Sodium Nitroprusside In Hypertensive Emergencies.
Answer:
Sodium nitroprusside is a powerful parenterally administered vasodilator that dilates both venous and arterial blood vessels resulting in a decrease in peripheral vascular resistance and in venous return.
The onset of its hypotensive effect is rapid. It is administered by continuous IV infusion for the treatment of hypertensive emergencies.
Question 20. Discuss Propranolol In Detail. Add A Note On Dental Consideration In Hypertensive Patient.
Answer:
Hypertensive Propranolol Actions
- Cardiovascular System
- Heart: Propranolol decreases heart rate, force of contraction, and cardiac output. It prolongs systole by retarding conduction so that the synergy of contraction of ventricular fibers is disturbed. The effects on a normal resting subject are mild but become prominent under sympathetic overactivity. Cardiac work and oxygen consumption are reduced as the product of heart rate and aortic pressure decreases.
- Blood vessels: Propranolol blocks vasodilatation and falls in BP evoked by isoprenaline and enhances the rise in BP caused by adrenaline. On prolonged administration BP gradually falls in hypertensive subjects but not in normotensive. Total peripheral resistance is increased initially and cardiac output is reduced-little change in BP with continued treatment, resistance vessels gradually adapt to chronically reduced cardiac output so that total peripheral resistance decreases—both systolic and diastolic BP fall.
- Respiratory Tract: Propranolol increases bronchial resistance by blocking β2 receptors.
- Local Anesthetic: Propranolol is as potent a local anesthetic as lidocaine, but is not clinically used for this purpose because of its irritant property.
- Metabolic: Propranolol blocks adrenergic ally-induced lipolysis and consequent increase in plasma-free fatty acid levels. Plasma triglyceride level and LDL/HDL ratio is increased during propranolol therapy.
- Skeletal Muscle: Propranolol inhibits adrenergic ally-provoked tremors. This is a peripheral action exerted directly on the muscle fibers. It tends to reduce exercise capacity by attenuating the increase in blood flow to the exercising muscles as well as by limiting glycogenolysis and lipolysis which provide fuel to working muscles.
Indications Or Therapeutic Uses
- Essential Hypertension: Propranolol is used alone or can be combined with either a diuretic or α-adrenergic blocking drug. The fall in blood pressure, when used alone, is gradual and without postural hypotension.
- Ischemic Heart Disease: It decreases the workload on the heart, diminishes myocardial oxygen demand, and increases exercise tolerance; hence β-blockers benefit patients having angina of effort. The drug should be given continuously and not merely when an attack occurs.
- Myocardial Infarction: β-blockers significantly decrease the incidence, recurrence, and mortality in cases of myocardial infarction after long-term use.
- Cardiac Arrhythmias: Propranolol is effective in all supraventricular tachycardias associated with high levels of circulating catecholamines as occurs with the use of certain general anesthetics like halothane, in digitalis toxicity, pheochromocytoma, and thyrotoxicosis. The beneficial effect is mainly due to an increase in the refractory period of the AV node and direct membrane stabilizing action.
- Congestive cardiac failure: Propranolol should be introduced gradually and should be maintained for a long time. The drug has the tendency to retard the progression of congestive cardiac failure.
- Dissecting aortic aneurysm: It reduces the cardiac contractile force and aortic pulsation. It also reduces the rate of development of pressure at the time of systole.
- Pheochromocytoma: The drug in pheochromocytoma control cardiac manifestations such as tachycardia and arrhythmia.
- Hyperthyroidism: The drug controls the sign and symptoms produced due to hyperthyroidism without affecting the thyroid status.
- Anxiety: Propranolol has anti-anxiety effects and controls palpitation, tachycardia, tremor, sweating, etc.
- Essential tremors: Propranolol provides relief in cases with essential tremors.
- Glaucoma: It reduces intraocular pressure by decreasing the production of aqueous humor.
Adverse Effects And Contraindications
- Bronchoconstriction: This is of little significance in normal persons but in asthmatics, or in patients with bronchitis or emphysema this effect could be life-threatening.
- Cardiac Failure: Cardiac patients always need a degree of sympathetic drive to support the heart to maintain proper cardiac output. β-blockers block this support and may aggravate heart failure.
- Hypoglycemia: The sympathetic response to hypoglycemia is a safety device that warns patients of diabetes to eat sugar, by producing symptoms like tachycardia, cold sweating, and tremors. β-blockers mask these symptoms and delay recovery from hypoglycemia.
- Bradycardia: Lowering of heart rate to 55 beats/min, as it occurs with β-blockers at times, can lead to life-threatening bradyarrhythmias and heart block.
- Cold Extremities: This results from a loss of receptor-mediated cutaneous vasodilatation in the extremities.
Drug Interactions
- Hypertensive patients receiving propranolol are very sensitive to the pressor responses of epinephrine because simultaneous blockade of vasodilatory β2 receptors provides an unopposed vasoconstricting action of epinephrine on α receptor.
- Enzyme inducers decrease the plasma concentration of propranolol.
- β-blockers impair the clearance of lignocaine and thus may increase its bioavailability.
Dental Consideration In Hypertensive Patient
- Detail case history of the patient is taken.
- Before the dental procedure, it should be confirmed that the patient is on antihypertensive therapy. If a patient is hypertensive and is not on therapy he/she should be immediately sent to consult a physician.
- Just before following the dental procedure blood pressure of the patient is checked. It should be 120/80 mm of Hg, i.e. within its normal limits.
- While giving anesthesia, the anesthetic agent should be used which is without epinephrine, as epinephrine constricts blood vessels and lead to an increase in blood pressure.
- After a surgical dental procedure, the surgical area should be properly cleaned and is sutured.
- Patients who are on alpha-blockers and vasodilators may undergo postural hypotension. So they are advised to take care during getting up from the dental chair.
Question 21. Explain The Drug Interaction Between Propranolol And Verapamil.
Answer:
Propranolol along with verapamil cause additive depression of the SA node and AV conduction and can lead to cardiac arrest.
Verapamil is a phenylethylamine calcium channel blocker that has maximal cardiac depressant activity among all calcium channel blockers. It reduces the calcium influx in SA Node and AV node thereby reducing their automaticity. Propranolol also has a depressant effect in the SA Node and AV node.
So, if both drugs are administered concomitantly, they exhibit additive depression of sinus rhythm and cardiac conduction. This may result in severe bradycardia to the extent of even asystole. This may prove fatal for the individual receiving this combination of drugs.
Question 22. Write A Short Note On Therapeutic Uses Of βBlockers.
Answer:
- Hypertension: β blockers are used to treat all grades of hypertension. They are also indicated in angina, myocardial infarction, and cardiac arrhythmias.
- In the prophylaxis of angina and myocardial infarction: β blockers decrease the oxygen demand of the myocardium and decrease the heart rate. These drugs reduce the frequency of angina attacks. They are indicated in the acute phase of myocardial infarction so that they limit the size of the infarct.
- In cardiac arrhythmias: They are indicated in atrial arrhythmias i.e. atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia.
- Congestive cardiac failure: Chronic usage of β blockers reduced the rate of mortality during chronic heart failure.
- Pheochromocytoma: These drugs control cardiac manifestations produced by pheochromocytoma.
- Glaucoma: They decrease intraocular pressure by decreasing the secretion of aqueous humor. Timolol is the choice of drug.
- In the prophylaxis of migraine: They decrease the frequency of migraine headaches.
- Hyperthyroidism: Signs and symptoms of hyperthyroidism decrease due to the blockade of β receptors.
- Essential tremors: Propranolol provides relief in tremors.
- Anxiety: It acts as an antianxiety drug.
- Alcohol withdrawal: Propranolol provides benefits for alcohol withdrawal.
- Dissecting aortic aneurysm: β blockers reduce cardiac contractility as well as the development of pressure during systole.
Question 23. Write Short Note On The Therapeutic Uses Of Clonidine.
Answer:
Clonidine is an antihypertensive drug.
Clonidine Uses
- It is used in hypertensives along with the diuretics.
- Opioid withdrawal: Clonidine suppresses sympathetic overactivity of opioid withdrawal syndrome and reduces craving to some extent.
- Clonidine has also facilitated alcohol withdrawal and smoking cessation.
- Clonidine has analgesic activity: It has been used to substitute morphine for intrathecal/epidural surgical and postoperative analgesia.
- Administered preoperatively, it diminishes anesthetic requirements.
- Clonidine attenuates vasomotor symptoms of menopausal syndrome.
- Clonidine has been used to control loose motions due to diabetic neuropathy.
Question 24. Explain Why Prazosin Is Used In Hypertension.
Answer:
Prazosin is a highly selective α1 blocker having α1:α2 selectivity ratio of 1000:1. All subtypes of α1 receptors, i.e. α1A, α1B, α1D are blocked equally. It blocks sympathetically mediated vasoconstriction and produces a fall in BP.
Question 25. Explain Why Ace Inhibitors Are Fist Line Drugs In The Treatment Of Hypertension.
Answer:
ACE inhibitors are first-line drugs in the treatment of hypertension because 50% of patients respond to monotherapy with ACE inhibitors and the majority of them rest to their combination with diuretics or β blockers or both.
Question 26. Explain The Mechanism Of Action And Adverse Effects Of Centrally Acting Sympatholytics.
Answer:
Centrally Acting Sympatholytics
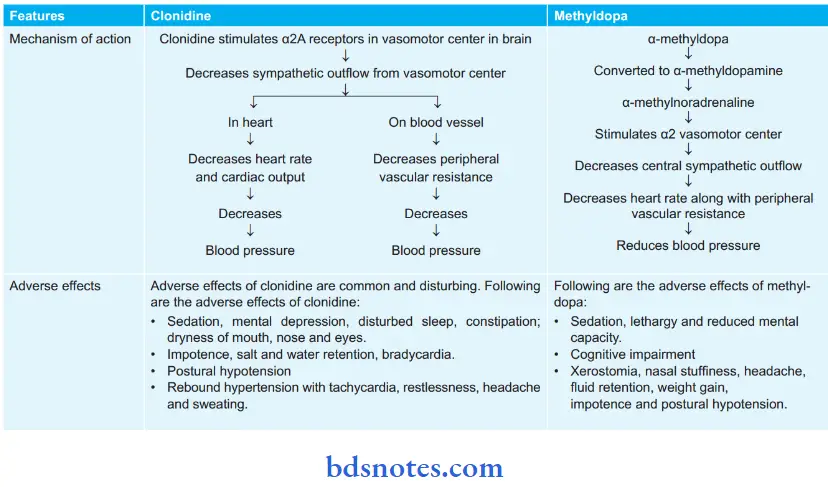
Centrally acting sympatholytics are clonidine and methyldopa.
Question 27. Classify Beta-Adrenergic Receptor Blockers. Describe Important Uses, Contraindications, And Adverse Effects Of Atenolol.
Answer:
Classification Of Beta-Adrenergic Receptor Blockers
- Nonselective (β1 and β2)
- Without intrinsic sympathomimetic activity: Propranolol, sotalol, timolol
- With intrinsic sympathomimetic activity: Pindolol
- With additional α blocking properties: Labetalol, carvedilol
- Cardioselective β1: Metoprolol, atenolol, acebutolol, bisoprolol, esmolol, celiprolol, nebivolol.
Atenolol Uses
- In young hypertensive patients who have high renin levels.
- In patients with angina pectoris.
- In patients with post-myocardial infarction.
- In patients with migraine.
- In patients with psychosomatic disorders.
- It is indicated in patients who receive vasodilators to counteract reflex tachycardia.
- It is indicated to subside symptoms of alcohol withdrawal.
- It is also indicated to treat the symptoms of grave’s disease till antithyroid medication produces its effect.
Atenolol Contraindications
- Bradycardia
- Cardiogenic shock
- Asthma (may cause bronchoconstriction).
- Symptomatic hypotension (blood pressure of less than 90/60 mm Hg with dizziness, vertigo, etc.)
- Angina of the Prinzmetal type (vasospastic angina)
- Metabolic acidosis (a severe condition with more acidic blood than normal)
- Severe disorders in the peripheral arterial circulation
- Atrioventricular blockage of second and third-degree (a particular form of arrhythmia)
- Acutely decompensated congestive heart failure [symptoms may be fluid retention with peripheral edema and/or abdominal fluid retention (ascites), and/or lung edema]
- Sick sinus syndrome (a particular form of arrhythmia)
- Hypersensitivity and/or allergy to atenolol
- Pheochromocytoma (a rare type of tumor of the adrenal glands)
- Atenolol should not be taken by patients with preexisting bronchial asthma.
- Atenolol may retard fetal growth and possibly cause other abnormalities, and is classified by FDA in pregnancy category D. It should be used during pregnancy only if absolutely necessary.
Atenolol Adverse Effects
Side effects have been known to include the following:
- Indigestion, constipation
- Dry mouth
- Dizziness or faintness (especially cases of orthostatic hypotension)
- Cold extremities
- Impotence
- Rhinitis
- Depression
- Confusion
- Insomnia, nightmares
- Fatigue, weakness, or lack of energy
- Edema.
The following more-serious side effects have also been observed and/or reported
- Hallucinations
- Low blood pressure (hypotension)
- Skin reactions, for Example. rash, hives, flaking of the skin, worsening of psoriasis
- The sensation of ‘pins and needles in hands or feet
- Irritated eyes, visual disturbances
- Difficulty in hearing
- Difficulty in speaking
- Unsteadiness when walking.
Question 28. Write uses of propranolol.
Answer:
Uses Of Propranolol
- Essential Hypertension: Propranolol is used alone or can be combined with either a diuretic or α-adrenergic blocking drug. The fall in blood pressure, when used alone, is gradual and without postural hypotension.
- Ischemic Heart Disease: It decreases the workload on the heart, diminishes myocardial oxygen demand, and increases exercise tolerance; hence β-blockers benefit patients having angina of effort. The drug should be given continuously and not merely when an attack occurs.
- Myocardial Infarction: β-blockers significantly decrease the incidence, recurrence, and mortality in cases of myocardial infarction after long-term use.
- Cardiac Arrhythmias: Propranolol is effective in all supraventricular tachycardias associated with high levels of circulating catecholamines as occurs with the use of certain general anesthetics like halothane, in digitalis toxicity, pheochromocytoma, and thyrotoxicosis. The beneficial effect is mainly due to an increase in the refractory period of the AV node and direct membrane stabilizing action.
- Congestive cardiac failure: Propranolol should be introduced gradually and should be maintained for a long time. The drug has the tendency to retard the progression of congestive cardiac failure.
- Dissecting aortic aneurysm: It reduces the cardiac contractile force and aortic pulsation. It also reduces the rate of development of pressure at the time of systole.
- Pheochromocytoma: The drug in pheochromocytoma control cardiac manifestations such as tachycardia and arrhythmia.
- Hyperthyroidism: The drug controls the sign and symptoms produced due to hyperthyroidism without affecting the thyroid status.
- Anxiety: Propranolol has antianxiety effects and controls palpitation, tachycardia, tremor, sweating, etc.
- Essential tremors: Propranolol provides relief in cases with essential tremors.
- Glaucoma: It reduces intraocular pressure by decreasing the production of aqueous humor.
Question 29. Describe The Other Uses Of Clonidine.
Answer:
Other Uses Of Clonidine
- It is used to treat withdrawal symptoms in opioid and alcohol addicts and smoking cessation.
- It is used as a pre-anesthetic agent.
- It is used as an antidiarrheal in diabetic neuropathy
- It reduces postmenopausal hot flashes
- It is used in the prophylaxis of migraine
- It has analgesic activity. It has been used to substitute morphine for intrathecal/epidural surgical and postoperative analgesia.
Question 30. Write A Short Note On The Adverse Effects Of Atenolol.
Answer:
The following are the adverse effects of atenolol:
Side effects have been known to include the following:
- Indigestion, constipation
- Dry mouth
- Dizziness or faintness (especially cases of orthostatic hypotension)
- Cold extremities
- Impotence
- Rhinitis
- Depression
- Confusion
- Insomnia, nightmares
- Fatigue, weakness, or lack of energy
- Edema.
The following more-serious side effects have also been observed and/or reported
- Hallucinations
- Low blood pressure (hypotension)
- Skin reactions, for Example. rash, hives, flaking of the skin, worsening of psoriasis
- A sensation of ‘pins and needles in hands or feet
- Irritated eyes, visual disturbances
- Difficulty in hearing
- Difficulty in speaking
- Unsteadiness when walking.
Question 31. Describe Briefly The Role Of Thiazides And Calcium Channel Blockers In the Management Of Hypertension.
Answer:
Role Of Thiazides In The Management Of Hypertension
Thiazides are used in the management of uncomplicated mild to moderate hypertension.
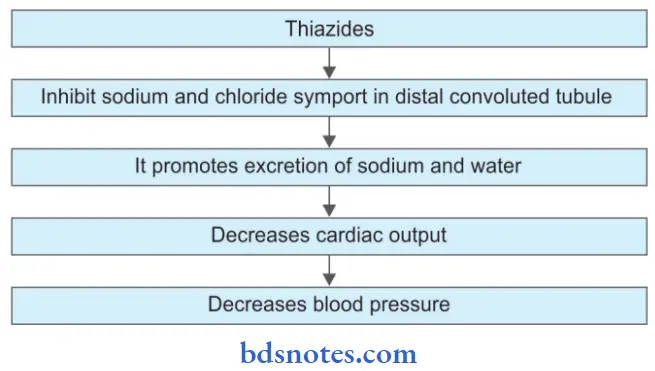
If chronic therapy of thiazide is given to the patient there is a decrease in sodium concentration in vascular smooth muscle which causes a decrease in pulmonary venous return and this leads to a decrease in blood pressure.
Along with thiazides, potassium-sparing diuretics should be given to counteract potassium loss and increase antihypertensive efficacy.
Role Of Calcium Channel Blockers In The Management Of Hypertension
- Calcium channel blockers lead to the dilatation of the arterioles which causes a decrease in peripheral vascular resistance. Examples are verapamil, diltiazem, and dihydropyridines.
- In calcium channel blockers dihydropyridines are the preferred drugs due to their selective action over blood vessels. Examples of dihydropyridines are nifedipine, amlodipine, felodipine, etc. These drugs reduce total peripheral resistance.
- Nifedipine causes reflex tachycardia. For counteracting reflex tachycardia β blockers are given with nifedipine. Nifedipine is given sublingually and is used in cases of hypertensive emergency.
- Verapamil decreases the force of contraction and decreases heart rate which reduces the oxygen requirement of the myocardium. This leads to a decrease in blood pressure.
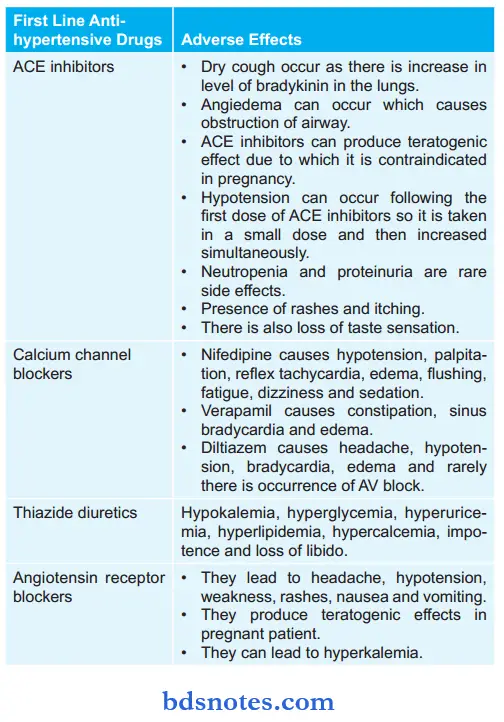
Question 32. Enumerate Fist Line Antihypertensive Drugs With Their Adverse Effects.
Answer:
Question 33. Classify Advantages Of Calcium Channel Blockers.
Answer:
Advantages Of Calcium Channel Blockers
- All calcium channel blockers are effective antihypertensive agents because of peripheral vasodilator activity. Blood pressure reduction appears to be more marked in those with low renin hypertension.
- Calcium channel blockers combine well with drugs that block the renin-angiotensin system (ACE inhibitors and angiotensin receptor blockers) to produce overall antihypertensive effects.
- Dihydropyridine calcium channel blockers are particularly useful in elderly patients with isolated systolic hypertension.
- Calcium channel blockers are efficacious, especially for isolated systolic hypertension.
- Calcium channel blockers have a lower incidence of side effects when compared to many older antihypertensive drugs.
- They are alternative agents in the treatment of chronic stable angina in patients without contraindications, who do not respond adequately to or tolerate, nitrates and α-blockers.
- Angina is secondary to coronary artery spasm and may respond particularly well to verapamil, diltiazem, or nifedipine.
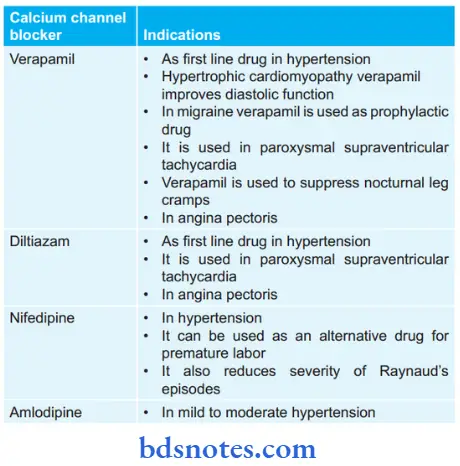
Question 34. Mention Four Calcium Channel Blockers And Their Indications.
Answer:
Following are the four calcium channel blockers and their indications:
Question 35. Write In Brief Antihypertensives Of Choice For Treatment Of High Blood Pressure, Detected Just Before Dental Procedure.
Answer:
Following are the antihypertensives of choice for the treatment of high blood pressure detected just before a dental procedure:
- Enalapril 2.5 to 40 mg OD orally.
Or - Lisinopril 5 to 40 mg OD orally.
Or - Ramipril 1.25 to 20 mg OD orally.
Or - Losartan 25 to 50 mg OD or BD orally.
Or - Propranolol 10 to 120 mg 2 to 4 times a day orally.
Or - Atenolol 25 to 100 mg OD orally.
Or - Amlodipine 2.5 to 10 mg OD orally.
Question 36. Enumerate Adverse Effects Of Propranolol.
Answer:
The following are the adverse effects of propranolol:
- Propranolol can accentuate myocardial insufficiency and worsen congestive heart failure.
- Bradycardia
- Propranolol worsens chronic obstructive lung disease and can precipitate bronchial asthma.
- Propranolol exacerbates variant angina due to unopposed mediated coronary constriction.
- Carbohydrate tolerance may be impaired in prediabetics.
- Plasma lipid profile is altered on long-term usage.
- If the gradual withdrawal of propranolol is not done after long-term use, it leads to rebound hypertension, worsening of angina, and sudden death.
- Tiredness and reduced exercise capacity.
- Cold hands and feet.
- GIT upset, lack of sexual drive, nightmares, forgetfulness, male patients have sexual distress.
Question 37. Classify And Enumerate Fist Line Antihypertensive Drugs.
Ans.
Following are the fist line antihypertensive drugs:
- Thiazide diuretics: Hydrochlorothiazide, chlorthalidone, indapamide
- Angiotensin II receptor blockers (ARBs): Losartan, candesartan, irbesartan, valsartan, telmisartan
- ACE inhibitors: Captopril, enalapril, lisinopril, perindopril, ramipril, fosinopril
- Calcium channel blockers: Verapamil, diltiazem, nifedipine, felodipine, amlodipine, nitrendipine, lacidipine
- Beta adrenergic blockers: Propranolol, metoprolol, atenolol.

Leave a Reply