Antiamoebic Drugs
Question 1. Why It Will Be Troublesome For A Patient To Take Metronidazole If He Is In a Habit Of Taking Alcohol?
Answer:
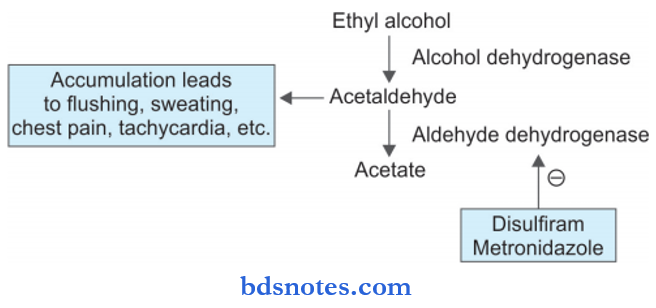
Metronidazole alters the metabolism of alcohol by inhibiting the aldehyde dehydrogenase enzyme. This leads to increased blood levels of the toxic metabolite acetaldehyde.
When the blood levels of acetaldehyde increase, the patient experiences unpleasant symptoms like increased heart rate, chest pain, palpitations, dizziness, flushing, sweating, weakness, vomiting, headache, etc.
Since these effects are also observed with an irreversible inhibitor of aldehyde dehydrogenase called disulfiram, this reaction is termed as a disulfiram-like reaction.
That’s why alcohol is avoided when metronidazole is induced.
Read And Learn More: Pharmacology Question And Answers
Question 2. Write In Brief About Antiamoebic Drugs And Their Significance In Dental Pharmacology.
Answer:
Antiamoebic drugs are those which are used to treat amoebiasis caused by the protozoan known as entamoeba histolytica.
Classification Of Antiamoebic Drugs
1. Tissue amoebicides
- For both intestinal and extraintestinal amoebiasis:
- Nitroimidazoles, i.e. metronidazole, tinidazole, Secnidazole
- Alkaloids: Emetine, dehydroemetine.
- For extraintestinal amoebiasis, i.e. chloroquine.
2. Luminal amoebicides
- Amide: Diloxamide furoate, nitazoxanide
- 8-hydroxyquinolines, i.e. quiniodochlor, diiodohydroxyquin
- Antibiotics: Tetracyclines.
Antiamoebic Drugs In Brief

Significance Of Antiamoebic Drugs In Dental Pharmacology
- Metronidazole is used in the treatment of alveolar abscesses, pericoronitis, periodontitis, etc.
- Metronidazole is used in acute ulcerative gingivitis. It is given as 200 to 400 mg for a week.
- Tinidazole is used in oriental anaerobic infections. It is given as 600 mg BD for 5 days.
- Tetracyclines are mainly used in chronic periodontitis. They are also used in the treatment of acute necrotizing ulcerative gingivitis.
Question 3. Mention The Basic Use Of Metronidazole In Orodental Infections.
Answer:
Metronidazole is of very high value in anaerobic or dental infections caused due to Bacteroides spp, Borrelia vincenti, Fusobacterium, Peptostreptococcus, and various other anaerobic microorganisms.
- Metronidazole is used in the treatment of alveolar abscesses, pericoronitis, periodontitis, etc.
- Metronidazole is used in acute ulcerative gingivitis or Vincent’s angina. It is given as 200 to 400 mg for a week. The drug is highly effective in Vincent’s angina as it is secreted in the saliva.
Question 4. Write In Short On Metronidazole.
Or
Write A Short Note On Metronidazole.
Or
Write Short Note On The Therapeutic Uses Of Metronidazole.
Answer:
- It is a highly active amoebicide.
- It has broad-spectrum tidal activity against protozoa, including Giardia lamblia in addition to the above two.
- Many anaerobic bacteria, such as Bacteroides fragilis, Clostridium perfringens, Helicobacter pyroli, spirochetes, and anaerobic Streptococci are sensitive.
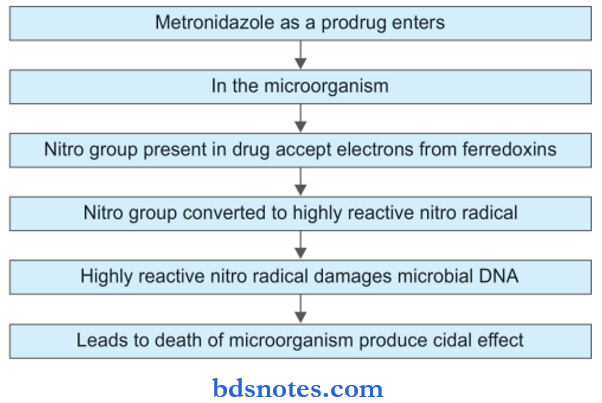
Metronidazole Mechanism Of Action
Metronidazole Pharmacokinetics
Metronidazole can be given orally, IV, and topically. The drug is well absorbed after oral administration and is poorly bound to plasma proteins.
Metronidazole diffuses well into the tissues including the brain. Its therapeutic levels are achieved in saliva, semen, vaginal secretion, bile, breast milk, and cerebrospinal fluid.
The drug is metabolized in the liver and metabolites are secreted in urine.
Metronidazole Adverse Effects
- Gastrointestinal: Nausea, anorexia, metallic taste, xerostomia, abdominal cramps. Occasionally there can be vomiting and looseness of stools.
- Allergic reactions: Skin rashes, urticaria, itching, and flushing.
- CNS effects: Irritability, dizziness, vertigo, confusion. At times convulsions and ataxia may occur. If chronic therapy is given polyneuropathy may occur.
- Disulfiram–like reaction: This can occur if metronidazole is taken with alcohol. The patient has nausea, vomiting, abdominal cramps, headache, and flushing.
Metronidazole Contraindications
It is contraindicated in:
- Neurological diseases
- Blood dyscrasias
- The first trimester of pregnancy
- Chronic alcoholism.
Metronidazole Uses
- Amoebiasis: Metronidazole is the first-line drug in the treatment of amoebiasis. For invasive dentistry and liver abscess 800 mg TDS is given for 7–10 days. For mild intestinal disease, 400 mg TDS is given for 5–7 days.
- Giardiasis: It is highly effective at a dose of 400 mg TDS for 7 days.
- Trichomonas vaginitis: It is the drug of choice and is given 400 mg TDS for 7 days.
- Anaerobic bacterial infections: These occur after colorectal or pelvic surgery or appendicectomy. Brain abscess and endocarditis may be caused by anaerobic organisms.
Metronidazole in combination with gentamycin or cephalosporins is equally effective. - Pseudomembranous enterocolitis: Oral metronidazole 800 mg TDS is effctive.
- H. pylori gastritis/Peptic ulcer: Metronidazole 400 mg TDS is frequently used along with amoxicillin/clarithromycin.
Use Of Metronidazole In Dentistry
- Metronidazole in a dose of 200–400 mg TDS is extensively used to treat dental infections because anaerobic bacteria are frequently involved. Certain oral anaerobes not inhibited by penicillin/amoxicillin are susceptible to metronidazole.
- It is the drug of choice for ANUG which is often combined with either penicillin V, amoxicillin, erythromycin, or tetracycline. The response is rapid with the disappearance of the causative spirochete fusobacterium complex from the lesions and resolution of pain, bleeding, ulceration, and bad breath within 2 to 3 days. A 5-day course is often sufficient.
- Periodontitis, pericoronitis, acute apical infections, and some endodontic infections also respond well to metronidazole given for 5–7 days. Because it is not active against aerobic and facultative bacteria, metronidazole is mostly combined with a penicillin, cephalosporin, or macrolide antibiotic.
Question 5. Describe Antiamoebic Drugs.
Answer:
Antiamoebic Drugs Chloroquine
Chloroquine kills trophozoites of E. histolytica and is highly concentrated in the liver. Therefore, it is used in hepatic amoebiasis only.
Because it is completely absorbed from the upper intestine and not so highly concentrated in the intestinal wall it is neither effective in invasive dysentery nor in controlling the luminal cycle (cyst passers).
For amoebic liver abscess, chloroquine is sometimes given along with or immediately after a course of metronidazole to ensure complete eradication of the trophozoites in the liver.
A luminal amoebicide must always be given with or after chloroquine to abolish the luminal cycle.
Antiamoebic Drugs Diloxanide Fuorate
It is a highly effective luminal amoebicide that directly kills tropho- zones responsible for the production of cysts. The furoate ester is hydrolyzed in the intestine and the released diloxanide is largely absorbed.
Diloxanide is a weaker amoebicide than its furoate ester, no systemic antiamoebic activity is evident despite its absorption. Diloxanide furoate exerts no antibacterial action.
lt is less effective in invasive amoebic dysentery, because of poor tissue amoebicidal action. However, it has produced high cure rates in mild intestinal amoebiasis and in asymptomatic cyst passers.
Diloxanide furoate is very well tolerated; the only side effects are flatulence, occasional nausea, itching, and rarely urticaria.
Antiamoebic Drugs Nitazoxanide
This congener of the anti-tapeworm drug niclosamide has been introduced for the treatment of giardiasis but is useful in amoebic dysentery and cryptosporidiosis also. Its active metabolite acts by inhibiting the enzyme pyruvate: ferredoxin oxidoreductase (PFOR) in the parasite.
Antiamoebic Drugs 8-Hydroxyquinolines
8-hydroxyquinolines were widely employed in the past. All have similar properties; are active against Entamoeba, Giardia, Trichomonas, some fungi, and some bacteria fungi (dermatophytes, Candida) and some bacteria.
They kill cyst-forming trophozoites in the intestine but do not have tissue amoebicidal action. They afford relief in chronic intestinal amoebiasis.
Their efficacy in eradicating- ing cysts from asymptomatic carriers is rated lower than that of diloxanide furoate and they are totally valueless in extraintestinal amoebiasis.
Antiamoebic Drugs Tetracyclines
They directly inhibit amoebae only at high concentrations. The older tetracyclines are incompletely absorbed in the small intestine, reach the colon in large amounts and inhibit the bacterial flora with which Entamoeba live symbiotically.
Thus, they indirectly reduce the proliferation of entamoeba in the colon and are especially valuable in chronic, difficult-to-treat cases with only the luminal cycle and little mucosal invasion.
Antiamoebic Drugs Emetine
- Emetine is a potent amoebicide and kills trophozoites but has no effect on cysts. It acts by inhibiting protein synthesis in amoebae by arresting intraribosomal translocation of the tRNA amino acid complex. In acute dysentery the stool is rapidly cleared of the trophozoites and symptomatic relief occurs in 1–3 days. It is highly efficacious in amoebic liver abscesses also.
- Emetine cannot be given orally because it will be vomited out. It is administered by SC or IM injection.
Question 6. Describe Metronidazole With Special References To Uses In Dentistry.
Answer:
Use Of Metronidazole In Dentistry
- Metronidazole in a dose of 200–400 mg TDS is extensively used to treat dental infections because anaerobic bacteria are frequently involved. Certain oral anaerobes not inhibited by penicillin/amoxicillin are susceptible to metronidazole.
- It is the drug of choice for ANUG which is often combined with either penicillin V, amoxicillin, erythromycin, or tetracycline. The response is rapid with the disappearance of the causative spirochete fusobacterium complex from the lesions and resolution of pain, bleeding, ulceration, and bad breath within 2 to 3 days. A 5-day course is often sufficient.
- Periodontitis, pericoronitis, acute apical infections, and some endodontic infections also respond well to metronidazole given for 5–7 days. Because it is not active against aerobic and facultative bacteria, metronidazole is mostly combined with a penicillin, cephalosporin, or macrolide antibiotic.
Question 7. Describe Important Adverse Effects And Uses Of Metronidazole.
Answer:
Adverse Effects Of Metronidazole
- Gastrointestinal: Nausea, anorexia, metallic taste, xerostomia, abdominal cramps. Occasionally there can be vomiting and looseness of stools.
- Allergic reactions: Skin rashes, urticaria, itching, and flushing.
- CNS effects: Irritability, dizziness, vertigo, confusion. At times convulsions and ataxia may occur. If chronic therapy is given polyneuropathy may occur.
- Disulfiam-like reaction: This can occur if metronidazole is taken with alcohol. The patient has nausea, vomiting, abdominal cramps, headache, and flushing.
Uses Of Metronidazole
- Amoebiasis: Metronidazole is the first-line drug in the treatment of amoebiasis. For invasive dentistry and liver abscess 800 mg TDS is given for 7–10 days. For mild intestinal disease, 400 mg TDS is given for 5–7 days.
- Giardiasis: It is highly effective at a dose of 400 mg TDS for 7 days.
- Trichomonas vaginitis: It is the drug of choice and is given 400 mg TDS for 7 days.
- Anaerobic bacterial infections: These occur after colorectal or pelvic surgery or appendicectomy. Brain abscess and endocarditis may be caused by anaerobic organisms. Metronidazole in combination with gentamycin or cephalosporins is equally effective.
- Pseudomembranous enterocolitis: Oral metronidazole 800 mg TDS is effctive.
- H. pylori gastritis/Peptic ulcer: Metronidazole 400 mg TDS is frequently used along with amoxicillin/clarithromycin.

Leave a Reply