Aminoglycoside And Macrolide Antibiotics
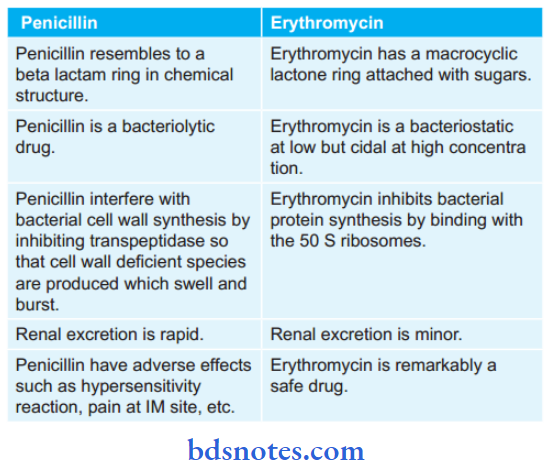
Question 1. Compare and contrast penicillin and erythromycin.
Answer:
Question 2. Describe Antimicrobials In Tooth Infection.
Answer:
During tooth infection the antibiotic cover is given to the patients undergoing:
- Scaling
- Root canal therapy
- Extraction of tooth
- Surgery involving gingival tissues.
Read And Learn More: Pharmacology Question And Answers
Antimicrobials Treatment Includes
- Treatment by using general anesthetics:
- Patients allergic to penicillin: IV vancomycin and IV gentamicin are preferred drugs.
- Patients not allergic to penicillin: Amoxicillin is the preferred drug.
- Treatment by using local anesthetics:
- Patients allergic to penicillin: Erythromycin is given
- Patients not allergic to penicillin: Amoxicillin is preferred.
Question 3. Enumerate Important Indication And Contraindication Of Streptomycin.
Answer:
Indications/Uses Of Streptomycin
- It was the first clinically used antitubercular drug.
- In subacute bacterial endocarditis, it is given in conjugation with penicillin.
- It causes rapid cures during the plague.
- It is also indicated in tularemia and brucellosis.
Contraindication Of Streptomycin
- Topical use is contraindicated due to far of contact sensitization.
- Oral use in diarrhea is contraindicated.
- It is contraindicated in UTIs, peritonitis, and septicemia due to low potency and widespread resistance.
- It is avoided in pregnancy as it can cause fetal ototoxicity.
Question 4. Write Side Effects And Contraindications Of Streptomycin.
Answer:
Side Effects Of Streptomycin
- Presence of vestibular disturbances.
- There is the presence of fever, eosinophilia, rashes, and exfoliative dermatitis.
- Pain at the injection site is common.
- Paresthesia and scotoma are occasionally present.
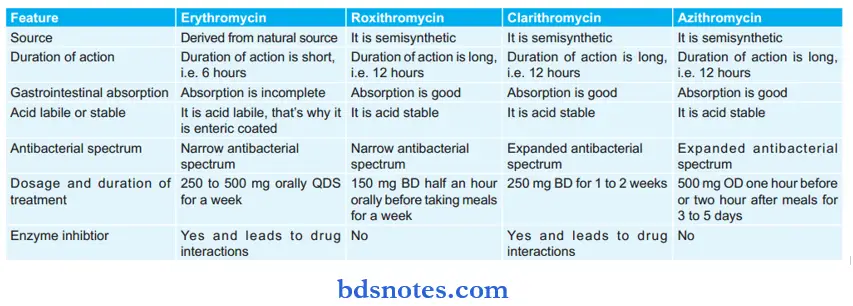
Question 5. Write A Short Note On Macrolide Antibiotics.
Answer:
These are the antibiotics having a macrocyclic lactone ring with the attached sugars.
- These include erythromycin, clarithromycin roxithromycin, and azithromycin which are bacteriostatic in low concentrations and bactericidal in large concentrations.
- They inhibit protein synthesis by binding to 50 S ribosomal RNA.
- Antibiotics are used against Gram-positive organisms.
Question 6. Write A Short Note On Gentamicin.
Answer:
It is a systemic aminoglycoside.
Gentamicin Mechanism Of Action
It is a bactericidal antibiotic. Its action is as follows:
- There is transport of aminoglycoside through the bacterial cell wall and cytoplasmic cell membrane.
- Binding to ribosomes result in the inhibition of protein synthesis.
Gentamicin Antibacterial Spectrum
- Gentamicin is used for gram-negative infections caused by E. coli, Klebsiella, Proteus, and Pseudomonas aeruginosa. The drug is also effective against Gram-positive infections caused by enterococci, streptococci, and staphylococci.
- Gentamicin also inhibits Streptococcus fecalis and various Staphylococcus aureus.
Uses Of Gentamicin
- Gentamicin is used in subacute bacterial endocarditis along with penicillin.
- It can be used alone or in combination with penicillin or cephalosporins in critically ill patients to prevent respiratory infections, in postoperative pneumonia. In patients with implants, community-acquired pneumonia.
- It can be used in burns, UTIs, pneumonia, lung abscess, osteomyelitis, septicemia, and middle ear infections.
- In infections caused by Gram-negative bacilli, i.e. urinary tract infections with pyelonephritis, pneumonia, meningitis, osteomyelitis, septicemia, and infected burns.
- In dentistry, gentamicin is used in combination with amoxicillin for prophylaxis of endocarditis in high-risk patients before the commencement of the dental procedure.
- Topically gentamicin is used as an ointment for skin lesions and burns. It is also used as an eye drop in conjunctivitis.
Adverse Effects Of Gentamicin
- Nephrotoxicity: It is encountered when therapy is continued for several days or in renal insufficiency, but this is reversible. Gentamicin binds to phospholipids of the renal brush border and leads to renal necrosis.
- Ototoxicity: When gentamicin gets concentrated in endolymph it leads to vestibular toxicity, i.e. vertigo and ataxia. The drug also gets concentrated in the perilymph of the inner ear and leads to cochlear toxicity, i.e. tinnitus and
hearing loss. - Neuromuscular blockade: Gentamicin blocks neuromuscular receptors of the motor endplate and leads to neuromuscular blockade.
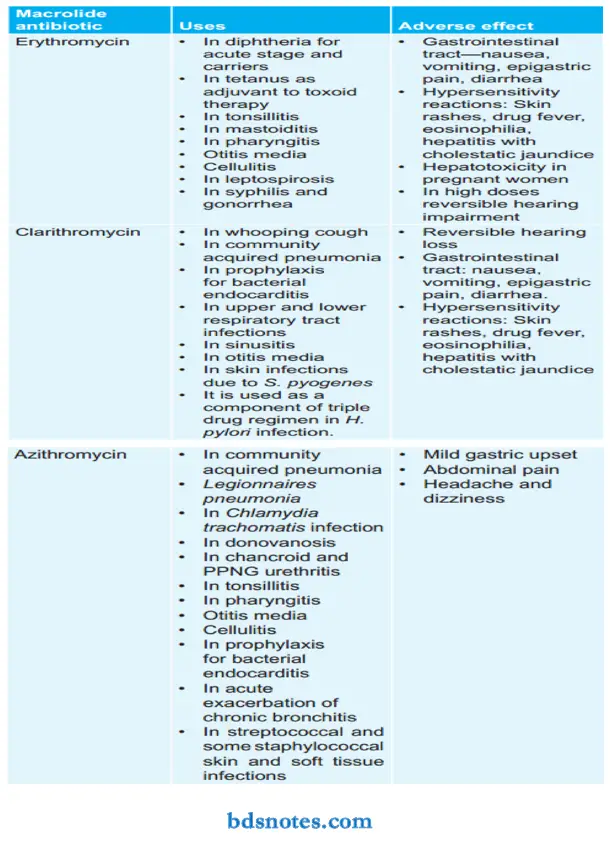
Question 7. Enumerate Macrolide Antibiotics. Describe The Important Uses And Adverse Effects Of Azithromycin.
Answer:
Enumeration Of Macrolide Antibiotics
- Older macrolide: Erythromycin
- Newer macrolide: Roxithromycin, clarithromycin, azithromycin.
Uses Of Azithromycin
- Legionnaires pneumonia: Azithromycin should be given 500 mg OD oral/IV for two weeks.
- Chlamydia trachomatis: In this, there is non-specific urethritis and genital infections are present in both men and women. 1 gm single dose of azithromycin is curative. It is also the drug of choice for chlamydial pneumonia.
- Donovanosis: It is treated with azithromycin 500 mg OD for 7 days.
- Chancroid and PPNG urethritis: Single 1 gm dose is highly curative.
- It is also used to cure pharyngitis, tonsillitis, sinusitis, otitis media, pneumonia, acute exacerbation of chronic bronchitis, streptococcal, and some staphylococcal skin and soft tissue infections.
- Prophylactic use: Azithromycin is given before surgical procedures to prevent bacterial endocarditis in patients with valvular lesions. It is also used for prophylaxis of recurrence in rheumatic fever.
Azithromycin Adverse Effects
- Mild gastric upset
- Abdominal pain
- Headache and dizziness.
Question 8. Classify Aminoglycoside Antibiotics. Describe The Important Uses And Adverse Effects Of Gentamicin.
Answer:
Classification Of Aminoglycoside Antibiotics
Systemic aminoglycosides: Streptomycin, gentamicin, kanamycin, tobramycin, amikacin, sisomicin, netilmicin
Topical aminoglycosides: Neomycin, framycetin.
Uses Of Gentamicin
- Gentamicin is used in subacute bacterial endocarditis along with penicillin.
- It can be used alone or in combination with penicillin or cephalosporins in critically ill patients to prevent respiratory infections, in postoperative pneumonia. In patients with implants, community-acquired pneumonia.
- It can be used in burns, UTIs, pneumonia, lung abscess, osteomyelitis, septicemia, and middle ear infections.
- In infections caused by Gram-negative bacilli i.e. urinary tract infections with pyelonephritis, pneumonia, meningitis, osteomyelitis, septicemia, and infected burns.
- In dentistry, gentamicin is used in combination with amoxicillin for prophylaxis of endocarditis in high-risk patients before the commencement of the dental procedure.
- Topically gentamicin is used as an ointment for skin lesions and burns. It is also used as an eye drop in conjunctivitis.
Adverse Effects Of Gentamicin
- Nephrotoxicity: It is encountered when therapy is continued for several days or in renal insufficiency, but this is reversible. Gentamicin binds to phospholipids of the renal brush border and leads to renal necrosis.
- Ototoxicity: When gentamicin gets concentrated in endolymph it leads to vestibular toxicity, i.e. vertigo and ataxia. The drug also gets concentrated in the perilymph of the inner ear and leads to cochlear toxicity, i.e. tinnitus and hearing loss.
- Neuromuscular blockade: Gentamicin blocks neuromuscular receptors of the motor endplate and leads to neuromuscular blockade.
Question 9. Write Short Note On Aminoglycosides.
Answer:
Aminoglycosides consist of two or more amino sugars which are attached by a glycosidic linkage to the hexose ring.
Classification Of Aminoglycoside
Antibiotics
Systemic aminoglycosides: Streptomycin, gentamicin, kanamycin, tobramycin, amikacin, sisomicin, netilmicin.
Topical aminoglycosides: Neomycin, framycetin.
Aminoglycoside Mechanism Of Action
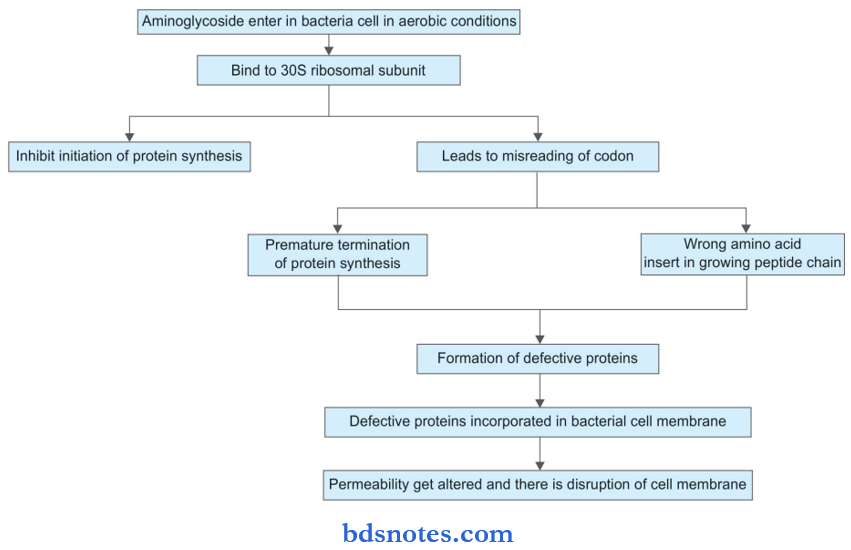
Aminoglycoside Pharmacokinetics
As aminoglycosides are polar compounds, they are poorly absorbed from the gastrointestinal tract, so they are given by the parenteral route for systemic effect.
They are mainly distributed into the extracellular fluid and poorly penetrate cerebrospinal fluid. Aminoglycosides are not metabolized in the body. These drugs are excreted unchanged in the urine.
Aminoglycoside Adverse Effects
- Ototoxicity: Aminoglycosides get concentrated inside the perilymph and endolymph of the inner ear which causes damage to vestibular and cochlear hair cells. Streptomycin and gentamycin mainly affect vestibular function while
amikacin, neomycin, and kanamycin affect auditory function. - Nephrotoxicity: Aminoglycosides become concentrated in the renal cortex and cause nephrotoxicity which is reversible. Nephrotoxicity is highest with neomycin and least with streptomycin.
- Neuromuscular blocking effect: Aminoglycoside inhibit the release of acetylcholine from the motor nerve ending and there is apnea and muscular paralysis.
- Hypersensitivity reactions: They are seen rarely in the form of skin rashes and drug fever.
- Aminoglycosides in pregnancy can lead to ototoxicity in the fetus.
Aminoglycoside Uses
They are mainly used in the following conditions:
- Burn
- Urinary tract infections
- Pneumonia
- Lung abscess
- Osteomyelitis
- Septicemia
- Meningitis
- Subacute bacterial endocarditis
- Tuberculosis
- Plague.
Question 10. Discuss The Adverse Effects Of Aminoglycosides.
Answer:
The following are the adverse effects of aminoglycosides:
- Ototoxicity: Aminoglycosides get concentrated inside the perilymph and endolymph of the inner ear which causes damage to vestibular and cochlear hair cells. Streptomycin and gentamycin mainly affect vestibular function while amikacin, neomycin, and kanamycin affect auditory function.
- Nephrotoxicity: Aminoglycosides become concentrated in the renal cortex and cause nephrotoxicity which is reversible. Nephrotoxicity is highest with neomycin and least with streptomycin.
- Neuromuscular blocking effect: Aminoglycoside inhibit the release of acetylcholine from the motor nerve ending and there is apnea and muscular paralysis.
- Hypersensitivity reactions: They are seen rarely in the form of skin rashes and drug fever.
- Aminoglycosides in pregnancy can lead to ototoxicity in the fetus.
Question 11. Describe The Mechanism Of Macrolide Antibiotics And Mention The Preferred Agent For Each Use And Their Adverse Effects.
Answer:
Mechanism Of Macrolide Antibiotics
Macrolides act by inhibiting bacterial protein synthesis. They combine with 50S ribosome subunits and interfere with translocation.
After peptide bond formation between the newly attached amino acid and nascent peptide chain at the acceptor site, the elongated peptide is translocated back to the peptidyl site making the acceptor site available for the next aminoacyl tRNA attachment.
This is prevented by macrolide and the ribosome fails to move along mRNA to expose the next codon. As an indirect consequence, the peptide chain may be prematurely terminated and the synthesis of larger proteins is specifically suppressed.
Basically, macrolides are bacteriostatic drugs but at high concentrations, they become bactericidal agents.
Preferred Macrolide Antibiotic Agent With Their Uses And Adverse Effects

Leave a Reply