Aggressive Periodontitis
Question 1. Write about aggressive periodontitis and give in detail about localized aggressive periodontitis.
Answer. Aggressive periodontitis is defined as a disease of periodontium occurring in an otherwise healthy adolescent which is characterized by rapid loss of alveolar bone but more than one tooth of permanent dentition. The amount of destruction present does not commensurate with the amount of local irritants. Aggressive periodontitis was classified as: Early onset periodontitis, therefore localized juvenile periodontitis has been changed to localized aggressive periodontitis, generalized aggressive periodontitis was classified as generalized juvenile periodontitis and rapidly progressive periodontitis.
Localized Aggressive Periodontitis
A disease occurring in otherwise healthy individuals, under the age of 30, with destructive periodontitis localized to the first permanent molars and the incisors, and not involving more than two other teeth. The severity of periodontal destruction is inconsistent with the amount of local factors present.
In 1923, Gottieb reported a disease that he called diffuse atrophy of alveolar bone. The disease is characterized by:
Stage 1. Degeneration of principle fiber of PDL which induce cessation of cementum formation and resorption of alveolar bone. Which cause tooth migration without any inflammatory involvement.
Stage 2. Lack of periodontal fiber result in the rapid proliferation of junctional epithelium along the root as the sign of inflammation appear.
Stage 3. inflammation progresses and there is development of deep infrabony periodontal pocket.
Read And Learn More: Periodontics Question And Answers
Aggressive Periodontitis Clinical Features
- Age and sex distribution: Both the sexes with female predilection from puberty to 20 years of age.
- Distribution of lesion: Three areas of localization of bone loss has been described.
- 1st molar or incisor.
- 1st molar or Incisor + Additional teeth not exceeding 14 teeth.
- Generalized involvement.
For localized juvenile periodontitis, classical distribution in the first molar and the incisors, with least destruction in cuspid and premolar area.
- Most striking feature is lack of clinical inflammation with presence of deep periodontal pocket.
- Formation of plaque which mineralizes to become calculus.
- Most common initial symptoms are movability and migration of 1st molar and incisors.
- As disease progresses other symptom-like root surface sensitivity, dull radiating pain, periodontal abscess formation and lymph node enlargement may occur.
- Presence of distolabial migration of maxillary incisors resulting in diastema formation.
- There is increase in the mobility of maxillary and mandibular incisors as well as first molars.
- There is presence of deep, dull radiating pain at the time of mastication due to irritation of supporting structures by mobile teeth and impacted food. Now the periodontal abscess may form and regional lymph node enlargement can occur.
- Patient may complaint of sensitivity of denuded root surfaces to thermal as well as tactile stimuli.
- In various cases of localized aggressive periodontitis, disease appears to be self limiting. Attachment loss and bone destruction do not spread to other teeth. This phenomenon of self-limiting activity along with advanced age is known as burn-out phenomenon.
- Isolated areas of attachment loss in otherwise healthy dentitions including recession associated with traumatic injuries, tooth position, impacted third molars, endodontic infection, root fractures, subgingival caries and subgingival restorations.
Aggressive Periodontitis Radiographic Finding
- Vertical or angular bone loss around the 1st molar and incisors.
- Presence of ‘Arc-shaped’ alveolar bone loss around first molars which extend from distal surface of second premolar to mesial surface of second molar. So, the bilateral “arc shaped’ bone loss is the mirror image and is characteristic of localized aggressive periodontitis.
- Presence of widening of periodontal ligament.
Aggressive Periodontitis Histopathological Features
These are same as seen during pocket formation:
- Ulceration of pocket epithelium
- Accommodation of inflammatory cells
- Bacterial invasion of connective tissue that reaches bone surface
Two types of bacteria are considered to be pathogens in localized aggressive periodontitis. - A. actinomycetemcomitans and Capnocytophaga.
Aggressive Periodontitis Treatment
Treatment for localized aggressive periodontitis is divided into two categories, i.e. non-surgical and surgical.
Nonsurgical Treatment
- Phase 1 therapy:
- Educate and motivate the patient.
- Oral hygiene instructions are given to the patient and counseling of the family members should be done.
- Scaling and root planning should be done.
- Anatomical factors should be corrected and occlusal adjustment should be done, if needed.
- Recall appointments should be kept for maintenance.
- Full mouth disinfection:
- Full mouth scaling and root planning (two visits under 24 hours)
- Dorsum of tongue should be brushed by the patient for 60 seconds with 1% chlorhexidine gel.
- Peritonsillar region should be sprayed by chlorhexidine for two times a day.
- 1% of chlorhexidine should be applied subgingivally in full depth of periodontal pockets till 10 minutes.
- Mouth should be rinsed by 0.2% chlorhexidine mouthwash for 2 minutes.
- Antibiotic therapy:
- Doxycycline 100 mg twice daily for 14 days is given in conjunction with periodontal therapy.
- Metronidazole 200 mg thrice daily for 10 days is given in combination with scaling and root planning.
- Combination of metronidazole 250 mg and amoxicillin 250 mg three times a day for 7 days along with surgical therapy show promising results.
- Local drug delivery system: In this small total doses of topical agents are delivered inside the pocket, thereby avoiding the side effects of systemic antibacterial agents. Additional direct delivery enhances the exposure of target microorganism to higher concentration, and subsequently gives more therapeutic outcomes. Various local drug delivery agents are formulated in form of solutions, gels, chips and fibers.
- Host modulation: Agents are administered which modulate the host response towards the disease. Administration of subantimicrobial – dose doxycycline may help to prevent periodontal tissue destruction by controlling action of matrix metalloproteinases.
- Photodynamic therapy: It eradicates the target cells, i.e. periodontal pathogens by reactive oxygen particles produced by photosensitizing compounds.
Surgical Therapy
- Modified Widman flap surgery can be done along with systemic tetracycline therapy.
- Regenerative procedures, i.e.
- Flap surgery + bone graft +antibiotic therapy + maintenance therapy
- Flap surgery + bone graft + GTR membrane + antibiotics + maintenance therapy
- Root resection or hemisection of affected first molar tooth, depending on the indication.
- Autotransplantation, i.e. extraction of involved mandibular first molar and autotransplantation of incompletely erupted third molar in socket.
- Extraction of hopeless teeth.
- Implant therapy is a good option in such cases.
Periodontal Maintenance Care
- Recall visits should be kept frequently.
- In every 3 to 4 months, a medical history review, periodontal and oral examination, scaling and root planning and last but not the least reinforcement of oral hygiene instructions.
- Presence of poor serum antibody response.
Question 2. Define aggressive periodontitis (local juvenile periodontitis). Write in detail on the etiology behind local juvenile periodontitis and elaborate on its clinical features, radiological features and treatment plan.
Answer.
Etiology of Local Juvenile Periodontitis
Microbiological
Presence of Aggregatibacter actinomycetemcomitans is a key factor which present in high numbers. Virulence factors produced by Aggregatibacter actinomycetemcomitans such as leucotoxin, lipopolysaccharide, proteases, collagenases, surface associated material affect immune response and lead to connective tissue destruction and bone resorption.
Immunological
- Defective chemotaxis due to functional defect in polymor-phoneutrophils.
- Presence of hyper-responsive monocytes which increases prostaglandin IL-1α and IL-1β production which causes bone resorption.
Genetic
- Familial aggregation is seen.
- As there is presence of specific gene which causes neutrophil abnormalities.
- Transmission through autosomal dominant mode of inheritance.
Environmental
Smoking causes progression of generalized aggressive periodontitis.
Current Concept
- Aggressive form of periodontitis is a multifactorial disease developing as a result of complex interaction between specific host genes and the environment.
- Interaction between disease process, environment and genetically controlled modifying factors contribute to specific clinical manifestations of the disease.
Question 3. Classify periodontal disease and write in detail localized aggressive periodontitis.
Or
Classify periodontal diseases. Write in detail about the clinical features and radiographic fidings of localized aggressive periodontitis.
Or
Describe clinical and radiological features of localized aggressive periodontics.
Answer.
Classification of Periodontal Disease
- Chronic Periodontitis
- Localized: Less than 30% of sites involved.
- Generalized: More than 30% of sites involved.
- Slight: 1–2 mm clinical attachment loss.
- Moderate: 3–4 mm clinical attachment loss.
- Severe: More than 5 mm clinical attachment loss.
- Aggressive Periodontitis
- Localized: Slight, moderate or severe.
- Generalized.
- Periodontitis as a Manifestation of Systemic Diseases
- Associated with hematological disorders:
- Acquired neutropenia.
- Leukemias.
- Others.
- Associated with genetic disorders:
- Familial and cyclic neutropenia.
- Down syndrome.
- Leukocyte adhesion defiiency syndrome.
- Papillon-Lefévre syndrome.
- Chèdiak-Higashi syndrome.
- Histiocytosis syndrome.
- Glycogen storage disease.
- Infantile genetic agranulocytosis.
- Cohen syndrome.
- Ehlers-Danlos syndrome (Types 4 and 8).
- Hypophosphatasia.
- Others.
- Associated with hematological disorders:
- Necrotizing Periodontal Diseases
- Necrotizing ulcerative gingivitis.
- Necrotizing ulcerative periodontitis.
- Abscesses of the Periodontium
-
- Gingival abscess.
- Periodontal abscess.
- Pericoronal abscess.
- Periodontitis Associated with Endodontic Lesions
Combined periodontic-endodontic lesions.
- Developmental or Acquired
- Deformities and Conditions:
- Localized tooth-related factors that modify or predispose to plaque-induced gingival diseases/periodontitis:
- Tooth anatomic factors.
- Dental restorations/appliances.
- Root fractures.
- Cervical root resorption and cemental tear.
- Mucogingival deformities and conditions around teeth:
- Gingival/soft tissue recession, facial or lingual surfaces, interproximal (papillary).
- Lack of keratinized gingiva.
- Decreased vestibular depth.
- Aberrant frenum/muscle position.
- Gingival excess:
- Pseudopocket
- Inconsistent gingival margin
- Excessive gingival display
- Gingival enlargement.
- Abnormal color.
- Mucogingival deformities and conditions on edentulous ridges:
- Vertical and/or horizontal ridge deficiency.
- Lack of gingival/keratinized tissue.
- Gingival/soft tissue enlargement.
- Aberrant frenum/muscle position.
- Decreased vestibular depth.
- Abnormal color.
- Occlusal trauma:
- Primary occlusal trauma.
- Secondary occlusal trauma.
- Localized tooth-related factors that modify or predispose to plaque-induced gingival diseases/periodontitis:
- Deformities and Conditions:
Question 4. Define aggressive periodontitis and write in detail on generalized aggressive periodontits.
Answer.
Generalized Aggressive Periodontitis
- It is usually characterized by the ‘general interproximal attachment loss affecting atleast three permanent teeth other than first molars and incisors.’
- Patients with generalized aggressive form may exhibit minimal amounts of microbial plaque associated with the affected teeth, i.e. quantitatively, the amount of plaque seems to be inconsistent with the amount of periodontal destruction; qualitatively, most pathogenic organisms may be associated, e.g. Porphyromonas gingivalis, A. actinomycetemcomitans, and Bacteroids forsythus.
Clinical Features
- Age and sex distribution: It affects person between puberty and 30 years, no sex discrimination.
- No specific pattern, all or most of the teeth are affected.
- Two types of gingival responses are seen, i.e. one is severe; acutely inflamed tissue which is often proliferating, ulcerated and fiery red, spontaneous bleeding and suppuration are commonly seen. In other cases, gingival tissue may appear pink and free of inflammation but deep pockets are seen by probing.
- Some of the persons may have systemic manifestations such as weight loss, mental depression and general malaise.
- Presence of poor serum antibody response.
Generalized Aggressive Periodontitis Radiographic Findings
Radiographic picture can range from severe bone loss associated with the minimal number of teeth, to advanced bone loss affecting the majority of teeth in the dentition.
Question 5. Write in detail about aggressive periodontitis its pathogenesis, clinical features, microbiologic findings and underlying immune mechanism.
Answer.
Aggressive Periodontitis Pathogenesis
- Bacterium A. actinomycetemcomitans is the primary organism in causing aggressive periodontitis. A. actinomycetemcomitans releases various virulence factors which leads to aggressive periodontitis.
- Bacterium produces a strong leukotoxin that kill neutrophils and macrophages which provides important defense against periodontal infections.
- Endotoxin produced by bacterium leads to activation of host cells to secrete inflammatory mediators such as prostaglandins, interleukin 1 and 3, TNF-α.
- Bacteriocin released by bacterium leads to inhibition of IgG and IgM production.
- Collagenases lead to degradation of collagen.
- Chemotactic inhibition factors leads to inhibition of neutrophil chemotaxis.
Aggressive Periodontitis Microbiologic Findings
- A. actinomycetemcomitans is the key microorganism in aggressive periodontitis. It shows virulence factors such as collagenases, leucotoxin, endotoxin, bacteriocin and chemotactic inhibition factors which leads to extensive periodontal destruction.
- Gram-positive organisms such as streptococci, actinomyces and peptostreptococci.
- Capnocytophaga species are seen.
- Eikenella corrodens and Prevotella intermedia are also seen.
Aggressive Periodontitis Immune Mechanism
- There is an intense infiltration of polymorphonuclear neutrophils which suggests the importance of polymorphonuclear neutrophils in local defense against the bacterial aggression and their major role during host mediated tissue destruction.
- B-lymphocytes and plasma cells constitute the mononuclear defense cells. Plasma cell majorly produces IgG and minor amount of IgA.
- Gingival crevicular fluid consists of active IgG which forms a line of defense against the initial bacterial invasion.
- Peripheral blood monocytes in patients suffering with aggressive periodontitis may demonstrate reduced autologous mixed lymphocyte reactions.
- High level of PGE2 and IL-lβ is observed in aggressive periodontitis patients.
- This demonstrates that T-helper cells are depressed in numbers compared to T-suppressor cells.
- Titer of antibodies is raised which is specificc to aggressive periodontitis associated microorganisms have been found in crevicular fluid than compared to peripheral blood.
- In aggressive periodontitis, there is decreased migration and function of polymorphonuclear neutrophils. These abnormalities are usually minor. These abnormalities in PMNs have been found to have familial aggregation.
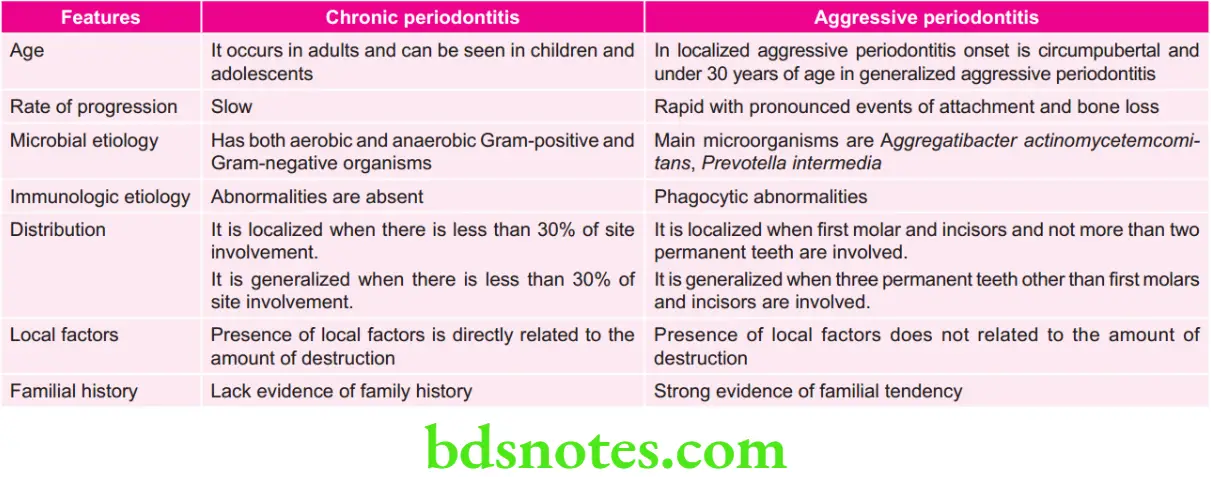
Question 6. Il lustrate the differences between chronic periodontitis and aggressive periodontitis.
Answer.
Question 7. Classify periodontitis. Describe the etiology, clinical features, radiographic appearance and management of generalized aggressive periodontitis.
Answer.
Classification of Periodontitis
- Chronic Periodontitis
- Localized: Less than 30% of sites involved.
- Generalized: More than 30% of sites involved.
- Slight: 1–2 mm clinical attchment loss.
- Moderate: 3–4 mm clinical attchment loss.
- Severe: More than 5 mm clinical attchment loss.
- Aggressive Periodontitis
- Localized: Slight, moderate or severe.
- Generalized.
- Periodontitis as a Manifestation of Systemic Diseases
- Associated with hematological disorders:
- Acquired neutropenia.
- Leukemias.
- Others.
- Associated with genetic disorders:
- Familial and cyclic neutropenia.
- Down syndrome.
- Leukocyte adhesion defiiency syndrome.
- Papillon-Lefévre syndrome.
- Chèdiak-Higashi syndrome.
- Histiocytosis syndrome.
- Glycogen storage disease.
- Infantile genetic agranulocytosis.
- Cohen syndrome.
- Ehlers-Danlos syndrome (Types 4 and 8).
- Hypophosphatasia.
- Others.
- Associated with hematological disorders:
- Necrotizing Periodontal Diseases
- Necrotizing ulcerative gingivitis.
- Necrotizing ulcerative periodontitis.
- Abscesses of the Periodontium
- Gingival abscess.
- Periodontal abscess.
- Pericoronal abscess.
- Periodontitis Associated with Endodontic Lesions
- Combined periodontic-endodontic lesions.
- Developmental or Acquired
- Deformities and Conditions:
- Localized tooth-related factors that modify or predispose to plaque-induced gingival diseases/periodontitis:
- Tooth anatomic factors.
- Dental restorations/appliances.
- Root fractures.
- Cervical root resorption and cemental tear.
- Mucogingival deformities and conditions around teeth:
- Gingival/soft tissue recession, facial or lingual surfaces, interproximal (papillary).
- Lack of keratinized gingiva.
- Decreased vestibular depth.
- Aberrant frenum/muscle position.
- Gingival excess:
- Pseudopocket
- Inconsistent gingival margin
- Excessive gingival display
- Gingival enlargement.
- Abnormal color.
- Mucogingival deformities and conditions on edentulous ridges:
- Vertical and/or horizontal ridge deficiency.
- Lack of gingival/keratinized tissue.
- Gingival/soft tissue enlargement.
- Aberrant frenum/muscle position.
- Decreased vestibular depth.
- Abnormal color.
- Occlusal trauma:
- Primary occlusal trauma.
- Secondary occlusal trauma.
- Localized tooth-related factors that modify or predispose to plaque-induced gingival diseases/periodontitis:
- Deformities and Conditions:
Generalized Aggressive Periodontitis
Generalized aggressive periodontitis is characterized by “generalized interproximal attachment loss affecting atleast three permanent teeth other than first molars and incisors”.
Generalized Aggressive Periodontitis Etiology
Patients with generalized aggressive form may exhibit minimum amount of microbial plaque associated with the affected teeth, i.e. quantitatively the amount of plaque seems to be inconsistent with amount of periodontal destruction; qualitatively most pathogenic organisms are associated, i.e. Porphyromonas gingivalis, A. actinomycetemcomitans and Bacteroides forsythus.
Generalized Aggressive Periodontitis Clinical Features
- It affects the individuals under the age of 30 years but older patients may also be affected.
- Two types of gingival responses are seen, i.e. one is severe, acutely inflamed tissue, oftn proliferating, ulcerated and firy red. Bleeding may occur spontaneously or with slight stimulation. The tissue response is believed to occur in destructive stage in which attchment and bone are actively lost. In other cases, gingival tissues may appear pink, free of inflammation and occasionally some degree of stippling along with deep pockets. Tissue response coincides with periods of quiescence in which bone level remain stationary.
- Presence of generalized interproximal attchment loss affecting at least three permanent teeth other than first molar and incisor.
- Some of the patients show systemic manifestations such as weight loss, mental depression and general malaise.
Generalized Aggressive Periodontitis Radiographic Appearance
Radiographic picture ranges from severe bone loss associated with minimum number of teeth to advance bone loss affecting majority of teeth in dentition.
Generalized Aggressive Periodontitis Management
Treatment for generalized aggressive periodontitis is divided into two categories i.e. non-surgical and surgical.
Nonsurgical Treatment
- Phase 1 therapy
- Educate and motivate the patient.
- Oral hygiene instructions are given to the patient and counseling of the family members should be done.
- Scaling and root planning should be done.
- Anatomical factors should be corrected and occlusal adjustment should be done if needed.
- Recall appointments should be kept for maintenance.
- Full mouth disinfection
- Full mouth scaling and root planning (two visits under 24 hours)
- Dorsum of tongue should be brushed by the patient for 60 seconds with 1% chlorhexidine gel.
- Peritonsillar region should be sprayed by chlorhexidine for two times a day.
- 1% of chlorhexidine should be applied subgingivally in full depth of periodontal pockets till 10 minutes.
- Mouth should be rinsed by 0.2% chlorhexidine mouthwash for 2 minutes.
- Antibiotic therapy
- Doxycycline 100mg twice daily for 14 days is given in conjunction with periodontal therapy.
- Metronidazole 200mg thrice daily for 10 days is given in combination with scaling and root planning.
- Combination of metronidazole 250mg and amoxicillin 250mg three times a day for 7 days along with surgical therapy show promising results.
- Local drug delivery system: In this small total doses of topical agents are delivered inside the pocket, thereby avoiding the side effects of systemic anti – bacterial agents. Additional direct delivery enhances the exposure of target microorganism to higher concentration and subsequently gives more therapeutic outcomes. Various local drug delivery agents are formulated in form of solutions, gels, chips and fibers.
- Host Modulation: Agents are administered which modulate the host response towards the disease. Administration of subantimicrobial – dose doxycycline may help to prevent periodontal tissue destruction by controlling action of matrix metalloproteinases.
- Photodynamic therapy: It eradicates the target cells i.e. periodontal pathogens by reactive oxygen particles produced by photosensitizing compounds.
Surgical Therapy
- Modified Widman flap surgery can be done along with systemic tetracycline therapy.
- Regenerative procedures, i.e.
- Flap surgery + bone graft +antibiotic therapy + maintenance therapy
- Flap surgery + bone graft + GTR membrane + antibiotics + maintenance therapy
- Root resection or hemisection of affected first molar tooth, depending on the indication.
- Autotransplantation i.e. extraction of involved mandibular first molar and autotransplantation of incompletely erupted third molar in socket.
- Extraction of hopeless teeth.
- Implant therapy is a good option in such cases.
Periodontal Maintenance Care
- Recall visits should be kept frequently.
- In every 3 to 4 months, a medical history review, periodontal and oral examination, scaling and root planning and last but not the least reinforcement of oral hygiene instructions.
Question 8. Define aggressive periodontitis. Discuss in detail about microbiology, clinical features, radiographic features and management of aggressive periodontitis.
Or
Write short note on aggressive periodontitis.
Or
Write short note on clinical and radiographic features of aggressive periodontitis.
Or
Discuss the etiology, clinical features and treatment of aggressive periodontitis.
Answer. Aggressive periodontitis is defined as a disease of periodontium occurring in an otherwise healthy adolescent which is characterized by rapid loss of alveolar bone but more than one tooth of permanent dentition. The amount of destruction present does not commensurate with the amount of local irritants.
Microbiology/Etiology
Localized Aggressive Periodontitis
- A. actinomycetemcomitans is a Gram-negative, facultative, non-motile, capnophilic, short coccobacilli which strongly caused strongly causing localized aggressive periodontitis. It is the key microorganism. There are fie sterotype antigen may be related to specificc sites of infection. Five sterotypes i.e. a, b, c, d, e of A. actinomycetemcomitans are identifid in localized aggressive periodontitis.
- Gram-positive organisms such as streptococci, actinomyces and peptostreptococci.
- Capnocytophaga species are seen.
- Campylobacter rectus
- Fusobacterium nucleatum
- Eikenella corrodens are also seen.
- P. gingivalis: It is the main organism associated with
- localized aggressive periodontitis
- Spirochetes
- Viruses: Cytomegalovirus, Epstein-Barr Virus
Generalized Aggressive Periodontitis
- P. gingivalis
- Aggregatibacter actinomycetemcomitans
- Tannerella forsythia
Aggressive Periodontitis Clinical Features
- Age and sex distribution: Both the sexes with female predilection from puberty to 20 years of age.
- Distribution of lesion: Three areas of localization of bone loss has been described.
- 1st molar or incisor.
- 1st molar or Incisor + Additional teeth not exceeding 14 teeth.
- Generalized involvement.
- For localized Juvenile periodontitis classical distribution in the first molar and the incisors, with least destruction in cuspid and premolar area.
- Most striking feature is lack of clinical inflammation with presence of deep periodontal pocket.
- Formation of plaque which really mineralize to become calculus.
- Most common initial symptoms are movability and migration of 1st molar and incisors.
- As disease progress other symptom like root surface sensitivity, dull radiating pain, periodontal abscess formation and lymph node enlargement may occur.
- Presence of distolabial migration of maxillary incisors resulting in diastema formation.
- There is increase in the mobility of maxillary and mandibular incisors as well as first molars.
- There is presence of deep, dull radiating pain at the time of mastication due to irritation of supporting structures by mobile teeth and impacted food. Now the periodontal abscess may form and regional lymph node enlargement can occur.
- Patient may complaint of sensitivity of denuded root surfaces to thermal as well as tactile stimuli.
- In various cases of localized aggressive periodontitis, disease appears to be self limiting. Attachment loss and bone destruction do not spread to other teeth. This phenomenon of self limiting activity along with advanced age is known as Burn out phenomenon.
- Isolated areas of attachment loss in otherwise healthy dentitions including recession associated with traumatic injuries, tooth position, impacted third molars, endodontic infection, root fractures, subgingival caries and subgingival restorations.
Generalized Aggressive Periodontitis
- Age and sex distribution: It affects person between puberty and 30 years, no sex discrimination.
- No specific pattern, all or most of the teeth are affected.
- Two types of gingival responses are seen, i.e. one is severe; acutely inflamed tissue which is often proliferating, ulcerated and fiery red, spontaneous bleeding and suppuration are commonly seen. In other cases, gingival tissue may appear pink and free of inflammation but deep pockets are seen by probing.
- Some of the persons may have systemic manifestations such as weight loss, mental depression and general malaise.
- Presence of poor serum antibody response.
Aggressive Periodontitis Radiographic Features
Localized Aggressive Periodontitis
- Vertical or angular bone loss around the 1st molar and incisors.
- Presence of ‘arc-shaped’ alveolar bone loss around first molars which extend from distal surface of second premolar to mesial surface of second molar. So, the bilateral “arc shaped’ bone loss is the mirror image and is characteristic of localized aggressive periodontitis.
- Presence of widening of periodontal ligament.
Generalized Aggressive Periodontitis
Radiographic picture can range from severe bone loss associated with the minimal number of teeth, to advanced bone loss affecting the majority of teeth in the dentition.
Management/Treatment of Aggressive Periodontitis
Treatment for aggressive periodontitis is divided into two categories, i.e. nonsurgical and surgical.
Nonsurgical Treatment
- Phase 1 therapy
- Educate and motivate the patient.
- Oral hygiene instructions are given to the patient and counseling of the family members should be done.
- Scaling and root planning should be done.
- Anatomical factors should be corrected and occlusal adjustment should be done if needed.
- Recall appointments should be kept for maintenance.
- Full mouth disinfection
- Full mouth scaling and root planning (two visits under 24 hours)
- Dorsum of tongue should be brushed by the patient for 60 seconds with 1% chlorhexidine gel.
- Peritonsillar region should be sprayed by chlorhexidine for two times a day.
- 1% of chlorhexidine should be applied subgingivally in full depth of periodontal pockets till 10 minutes.
- Mouth should be rinsed by 0.2% chlorhexidine mouthwash for 2 minutes.
- Antibiotic therapy
- Doxycycline 100 mg twice daily for 14 days is given in conjunction with periodontal therapy.
- Metronidazole 200 mg thrice daily for 10 days is given in combination with scaling and root planning.
- Combination of metronidazole 250 mg and amoxicillin 250mg three times a day for 7 days along with surgical therapy show promising results.
- Local drug delivery system: In this small total doses of topical agents are delivered inside the pocket, thereby avoiding the side effects of systemic anti – bacterial agents. Additional direct delivery enhances the exposure of target microorganism to higher concentration and subsequently gives more therapeutic outcomes. Various local drug delivery agents are formulated in form of solutions, gels, chips and fibers.
- Host Modulation: Agents are administered which modulate the host response towards the disease. Administration of subantimicrobial – dose doxycycline may help to prevent periodontal tissue destruction by controlling action of matrix metalloproteinases.
- Photodynamic therapy: It eradicates the target cells i.e. periodontal pathogens by reactive oxygen particles produced by photosensitizing compounds.
Surgical Therapy
- Modified Widman flap surgery can be done along with systemic tetracycline therapy.
- Regenerative procedures i.e.
- Flap surgery + bone graft +antibiotic therapy + maintenance therapy
- Flap surgery + bone graft + GTR membrane + antibiotics + maintenance therapy
- Root resection or hemisection of affected first molar tooth, depending on the indication.
- Autotransplantation i.e. extraction of involved mandibular first molar and autotransplantation of incompletely erupted third molar in socket.
- Extraction of hopeless teeth.
- Implant therapy is a good option in such cases.
Periodontal Maintenance Care
- Recall visits should be kept frequently.
- In every 3 to 4 months, a medical history review, periodontal and oral examination, scaling and root planning and last but not the least reinforcement of oral hygiene instructions.

Leave a Reply