Lower Limb Ischaemia
The majority of the individuals are conscious of the chest pain caused by myocardial ischaemia. However, patients present relatively late to the hospital with ischaemia of the lower limb.
The disease, even though benign, is not curable totally, thus causing financial, social and psychological burdens to the patient and his relatives.
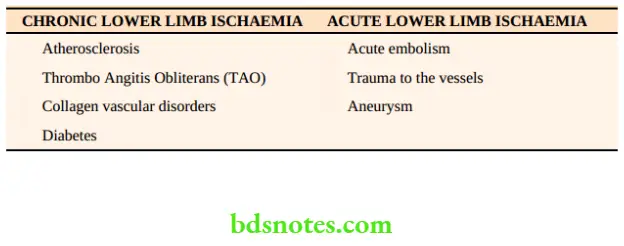
Causes Of Lower Limb Ischaemia
Other rare causes of lower limb ischaemia include popliteal entrapment syndrome and cystic medial degeneration. One should not forget that diabetes is also one of the common causes of peripheral vascular disease in elderly patients.
Lower Limb Ischaemia Collateral Circulation
- Collateral circulation is present in most of the organs. Hence, even if a major vessel is occluded the organ can still survive provided collaterals are well developed.
- Chronic ischaemia caused by TAO or atherosclerosis, allows sufficient time for collaterals to develop. Hence necrosis or gangrene which occurs is minimised. Thus, limbs often survive.
- In acute ischaemia caused by thrombus or embolism, there is no time for collaterals to develop. This results in gangrene of the limb, in untreated cases.
Read And Learn More: Clinical Medicine And Surgery Notes
Lower Limb Ischaemia Symptoms
1. Pain in the limb is the chief symptom of lower limb ischaemia. It is a severe cramp-like pain, due to ischaemia of the muscles, brought on mainly by exertion. It is called intermittent claudication.
Rest Pain
It is an intractable type of pain usually felt in the foot, toes, etc. It is an indication of severe ischaemia of the foot with impending gangrene. Typically, a patient with rest pain sits on the bed, holds his foot with both hands or may hang the foot out of bed. This gives him some kind of relief. Rest pain is worse at night time1. It may lead to suicidal tendencies.
Grades Of Intermittent Claudication
- Grade 1 Patient walks for a distance, gets the pain, continues to walk and the pain disappears. As a result of ischaemia, anaerobic metabolism takes place, which produces substance P, lactic acid, etc.
- Grade 2 Patient walks for a distance, gets the pain, and continues to walk with the pain. He has a limp.
- Grade 3 Patient walks, and gets the pain. He has to take a rest. This grade indicates severe muscle ischaemia.
- Grade 4 Pain at rest is due to ischaemia of nerves* in addition to ischaemia of the muscles.
Cry of the dying nerves, due to the involvement of vasa nervorum
- Claudication distance refers to the distance a patient is able to walk before the onset of pain. A patient with severe claudication may not be able to walk for a few yards.
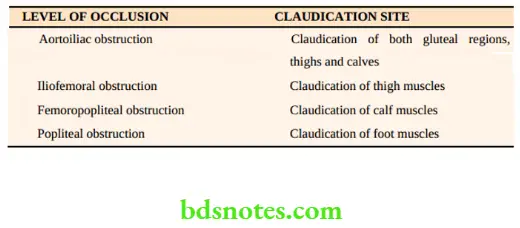
- The site of claudication depends upon the level of arterial occlusion
2. A nonhealing ulcer is the next common presenting symptom. It is usually precipitated by minor trauma and it occurs in the most distal part of the body such as the tip of the toes. Ischemic ulcers are very painful and deep.
Some patients present with gangrenous patches of skin or subcutaneous tissue. Gangrene affects distal parts such as the toes. However, gangrene is minimal because of collaterals.


1One of our TAO patients with sleepless nights due to rest pain committed suicide by jumping from the 2nd floor of the hospital.
4. A history of bilateral gluteal claudication with impotence can occur in a young patient due to a saddle thrombus at the bifurcation of the aorta. It is called Leriche’s syndrome. Impotence is due to failure to achieve an erection due to paralysis of the L1 nerve—which can have bilateral gangrene.

Gluteal claudication is confused for sciatica and many patients are referred to the orthopaedic department. This is neurogenic claudication which is present even at rest and aggravated on movements of the spine. Causes of neurogenic claudication are slipped discs, fractured vertebrae, tuberculosis of the spine, etc.
5. Coldness, numbness, paraesthesia and colour changes indicate chronic ischaemia.
6. The majority of patients with peripheral vascular disease are smokers. TAO occurs exclusively in male smokers1.
1A 26-year-old female, nonsmoker patient presented to the hospital with ischaemic features of the right upper limb. All causes of upper limb ischaemia were ruled out (Raynaud’s, cervical rib, etc.). On careful questioning, she admitted to using SNUFF DIPPING for 10 years (snuff contains nicotine).
Gluteal Claudication SIGNS
The Gluteal Claudication findings are appreciated better if a comparison is made with the opposite limb.
Evidence of chronic ischaemia of the leg is as follows.
- Flattening of the terminal pulp spaces of toes.
- Fissures, cracks in between the toes.
- Ulceration of toes, interdigital ulcers.
- Brittle, flat and ridged nails, and shiny skin Loss of hair and loss of subcutaneous fat.
- limb may appear more dark in dark-skinned patients or markedly pale in fair-skinned patients with vasospastic diseases like tao.
- Gangrene is usually dry with a clear line of demarcation. It indicates the junction of dead and living tissue. Since the blood supply to the muscle is better, usually the line of demarcation involves skin and subcutaneous tissue. Line of demarcation is very well appreciated in senile gangrene where it can be skin, muscle or bone deep.
- The limb may show atrophy of muscles.
Palpation
- Ulcer: Examination should be done as described in Chapter 6. Ischaemic ulcers are very tender.
- Gangrene is described according to its size, shape and extent. In dry gangrene, the part is dry and mummified or shrunken. Features of dry gangrene are summarised.
- Limb above2
-
- Ischaemic limb is cold: Careful palpation from above downwards will reveal the change in temperature from warm to the cold area. Temperature changes are appreciated better with the dorsum of the hand which is more sensitive as it has a lot of cutaneous nerve endings.
- Tenderness: It is tender due to the presence of inflammation.
- Sensation: Due to the irritation of nerve endings, the ischaemic limb is hypersensitive.3
- Pitting oedema can be due to thrombophlebitis or due to the nonfunctioning of the limb.
2It is better to palpate the entire limb from the thigh downwards.
Gangrene
- Loss of temperature
- Loss of pulsation
- Loss of sensation
- Loss of colour
- Loss of function
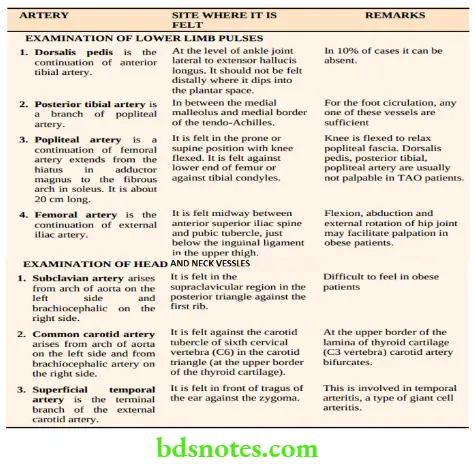
4. Palpation Of Pulses
- After examining the pulses, results are interpreted in a pulses chart as shown on the next page.
- In a similar manner, upper limb pulses, and head and neck pulses are also recorded in the pulses chart.
Other Tests Of Minor Importance
- Buerger’s postural test is relevant in fair-skinned patients. The patient (supine) is asked to raise his legs vertically upwards keeping the knees straight. In cases of chronic ischaemia, marked pallor develops within 2–3 minutes. The angle at which pallor develops is Buerger’s angle of circulatory insufficiency. In the ischaemic limb, pallor develops even on an elevation of leg up to 15–30 degrees.
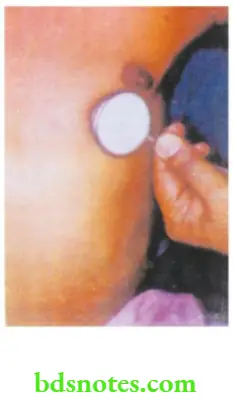
- Capillary refilling test: Apply pressure over the tip of the terminal pulp space for a few seconds and release the pressure. Rapid return of circulation is observed in normal persons.
-
- The test can also be done on the ischaemic foot by asking the patient to sit up and hang his legs down and observe for colour changes. The time taken for the ischaemic foot to become pink is described as capillary filling time. This is prolonged in an ischaemic foot.
Auscultation
Auscultation Of Heart
- Systolic bruit over the femoral artery can be heard in atherosclerotic occlusion of the ilio-femoral segment, due to turbulence created by the blood flow.
- Auscultation of the heart to rule out mitral stenosis (mid-diastolic murmur, loud 1st heart sound, etc.).

Ischaemic limb is like an irritable personality.
A thorough clinical examination of pulses includes not only lower limb vessels but also head, neck and upper limb vessels.
Classification Of Buerger’s Disease
- Type 1: Upper extremity
- Type 2: Crural (leg and foot)
- Type 3: Femoral type—femoropopliteal
- Type 4: Aortoiliac
- Type 5: Generalised type
Leo Buerger described TAO in 1908
Pulses Chart
(For example, a classical case of TAO left lower limb)
Lower Limb Pulses Right Left
- Dorsalis pedis ++++ –
- Posterior tibial ++++ –
- Popliteal ++++ ++
- Femoral ++++ ++++
++++ : Normal; ++ : Weak; – : Absent.
Auscultation Of Heart
Palpation Of Peripheral Arteries—Lower Limb Upper Limb Head And Neck








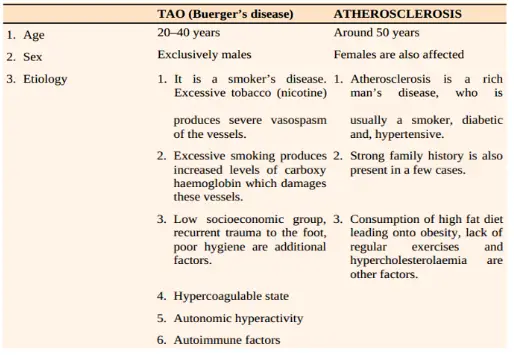
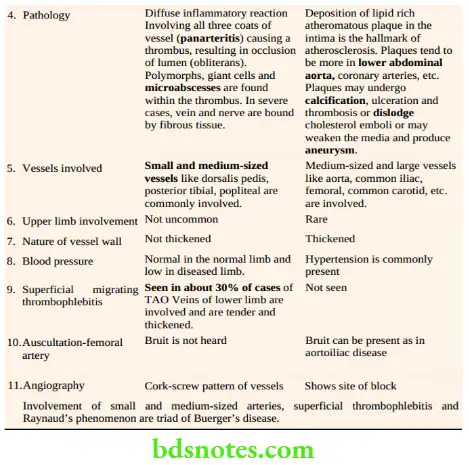
Differential Diagnosis
- Even though there are many causes of lower limb ischaemia, thromboangitis obliterans (TAO) and atherosclerotic vascular disease are the most common causes. Hence they have to be considered first before giving other diagnosis
- TAO is also called Buerger’s disease -the details are given.
- Atherosclerotic vascular disease is the most common cause of lower limb ischaemia. It can manifest as a simple ulcers to massive gangrene.
Auscultation Of Heart
Investigations
- Complete blood picture
- Blood sugar estimation
- Normal levels—FBS 80–120 mg/dl and PPBS 120–180 mg/dl. Mainly help in diabetic patients.
- Serum cholesterol
- Normal levels—150–250 mg/100 ml. Usually, they are altered in atherosclerotic patients.
- Angiography (Arteriography)
-
- It is not usually indicated in TAO patients where direct arterial surgery is not done. However, a few cases of presenile atherosclerosis that are misdiagnosed as TAO will require angiography to locate the site of obstruction which is suitable for arterial reconstruction. Angiography is indicated in patients with atherosclerotic vascular disease, to know the exact site of the block, and type of obstruction, and to define the collaterals, so as to plan for arterial reconstruction.
Types Of Angiography
- Percutaneous transfemoral retrograde angiography: This is done in unilateral obstruction. An incision is made in the upper thigh to expose the femoral artery on the normal side. A Seldinger needle and guide wire are used to introduce the arterial catheter and radioopaque dye is introduced after placing the catheter into the aorta. It visualises the entire aortoiliac segment and below (Seldinger technique).
- Direct trans lumbar angiography or aortography: It is indicated when an obstruction is bilateral, both femoral pulses are not palpable, clinically manifesting as bilateral lower limb ischaemia. The aorta is directly punctured from behind (trans lumbar) by using an ultrasound image intensifier.
Results: Arteriography establishes the site of the block and the nature of collaterals.
Complications Of Angiography
- Thrombosis at the puncture site results in ischaemia.
- Haemorrhage from the puncture site which needs to be stopped by pressure packing.
- Arterial dissection if the catheter is wrongly placed and advanced.
- Anaphylaxis—can be avoided by a trial injection.
- Paraplegia6 due to spasms of spinal arteries
- Infection
5. Digital subtraction angiography (DSA): This can be done by arterial or venous route. The arterial route is preferred.
DSA gives excellent pictures of carotid and large central vessels. However, the peripheral vessels may not reveal adequate information. Thus, conventional arteriography still has an important role in atherosclerotic vascular disease.
5Normal limb is selected for two reasons:
- Femoral pulse is palpable hence easy to locate the artery and introduce the catheter.
- If a thrombus occurs in the diseased limb due to angiography, it will worsen the ischaemia and may lead to gangrene.
6Because of these complications, angiography should be done carefully only when it is indicated.
6. Doppler ultrasound blood flow detector: This test is based on the Doppler principle. An ultrasound signal is beamed at an artery and the reflected beam is picked up by a receiver. Frequency changes of the beam due to the moving blood are converted into audio signals which can be heard by using a probe. Thus, a Doppler probe can be used to detect the pulse even when the pulse is clinically not palpable.
- By using a sphygmomanometer, systolic blood pressure (BP) of the limb can be measured by positioning the cuff at a suitable level and the pressure index can be calculated.
- Normal values are above 1. However, in patients with peripheral vascular disease values are below 1. Values below 0.9 indicate vascular obstruction.
- When ankle pressure is less than 30 mmHg, gangrene may be imminent.
Uses Of Doppler Probe
- To feel the normal pulse as in operation theatres.
- To feel clinically non-detectable pulse as in peripheral vascular disease.
- To measure BP in ischaemic limb.
- Remeasuring BP in the lower limb after exercise to differentiate ischaemic claudication from neurogenic claudication.
7. Duplex scan
This is the investigation of choice today. A duplex scan is a combination of Doppler with B-mode ultrasound. With the availability of colour Duplex, the direction of blood flow can be assessed. Red colour means the direction of flow towards the transducer and blue means away.

8. Plethysmography: In this method changes in the volume of the limb or digit can be assessed
- It is performed by placing the limb in an air and water-tight metal container which is connected to a floating needle. As the pressure pulse passes through one segment of the limb, a wave is generated and it is recorded.
- Thus, it is an accurate method to assess the changes in blood volume in the limb, indirectly estimating vasodilatation
- Oculoplethysmography is used to evaluate carotid artery disease.
Treatment Of Peripheral Vascular Disease (Tao And Atherosclerosis)
- In all patients with peripheral vascular disease, the following general measures are to be taken which will help in better perfusion of the lower limb tissues.
- Anaemia must be treated with hematinics and blood transfusion. If the ejection fraction is low, drugs are given to improve cardiac output.
Principles
1. To relieve the pain
As already discussed, the pain is very severe and distressing.
Some amount of pain relief can be obtained as follows:
- Analgesics: Simple analgesics may not help these patients.
- Aspirin (300 mg) one tablet 3 times a day can be used. It also has anti adhesive effect on platelets.
- Ketorolac 10–20 mg one tablet 3 times a day can be given in severe cases.
- Narcotic analgesics can be used judiciously in cases with rest pain.
- Buerger’s position by elevating the head end of the bed, causes venous congestion and reflex vasodilatation.
- Buerger exercises by elevation and dependency of the limb for a few minutes.
- Heel raise: By raising the heels of shoes by 1–2 cm, claudication distance can be increased as it decreases the load on the calf muscles.
2. To Arrest The Progression Of The Disease
- Stop smoking. This is more beneficial in TAO patients than in atherosclerotic patients.
- Regular exercises
- Reduce obesity
- Diet: To avoid fatty food to avoid choices tool. It is more useful in patients with hyperlipidaemia.
- Avoid injuries.
3. Role Of Vasodilators
- Vasodilators have not been found to be useful in atherosclerotic vascular disease.
Principles Of Treatment
- To relieve pain
- To arrest the progress of the disease
- Role of vasodilators
- Chemical sympathectomy
- Surgical methods
Some degree of improvement in reducing pain and healing of cutaneous ulcers has been
- Found in TAO patients.
- The drugs are pentoxyphylline, prostacyclin or Xanthinol nicotinate (Complamina).
- A few cases of Buerger’s disease benefit from the injection of xanthinol nicotinate (Complamina) given in a graded dose, for example. 3000 mg on the 1st day, 4500 mg on the 2nd day, 6000 mg on the 3rd day, 7500 mg on the 4th day and 9000 mg on the 5th day followed by an injection of low molecular weight dextran. Injection of xanthinol nicotinate helps in the following ways.
- In a few cases, it helps in the healing of cutaneous ulcers.
- To improve claudication distance
- To postpone lumbar sympathectomy
- Repeat courses of vasodilators are necessary to control the disease.
- However, it should be remembered that the treatment is only temporary.
4. Chemical sympathectomy
- It acts by producing vasodilatation of the blood vessels of the lower limb.
- In this procedure, 5 ml of phenol in water is injected beside the bodies of 2nd, 3rd and 4th lumbar vertebrae.
- The effect of the drug can be judged immediately by feeling the warm feet.
- It helps in the healing of ulcers and may improve rest pain probably by interfering with afferent sensory circuits.
Precautions
- Lateral injection by using a lumbar puncture needle
- Injection should be in front of the lumbar fascia which contains the sympathetic trunk.
- Avoid injuries to the aorta and inferior vena cava
- The procedure is to be done under X-ray control (Screening) Since phenol has replaced lignocaine because of its long-lasting effect, it is also called phenol sympathectomy.
5. Surgical procedures in TAO
1. Lumbar sympathectomy is the indirect surgery done for TAO patients since direct arterial surgery is not possible.
- Indications: Cutaneous ulcer and rest pain.
- Structures which can be confused for the lumbar sympathetic trunk are:
- Genitofemoral nerve
- Tendon strip of psoas muscle
- Lymphatic chain and fatty tissue
- One should be careful not to damage lumbar veins7 which join the inferior vena cava.
- By depriving the sympathetic nerve supply to lower limb blood vessels, vasomotor tone is reduced so that some amount of vasospasm is reduced. Thus, rest pain improves, and minor ulcerations heal due to cutaneous vasodilatation. However, the duration of the effect of lumbar sympathectomy is not clear.
- Both sides can be done in one sitting. However, during bilateral operation, the 1st lumbar ganglion on one side should be left since removal of both ganglia may cause sterility due to paralysis of the ejaculatory mechanism.
Salient Features Of Lumbar Sympathectomy
- Transverse loin incision
- Extraperitoneal approach and it is a preganglionic sympathectomy.
- The Lumbar sympathetic trunk is identified in the paravertebral gutter lateral to the psoas muscle as a cord-like structure.
- 2nd lumbar ganglion is large and has white rami joining it.
- The sympathetic trunk is divided below the first lumbar vertebra and removed up to the 4th lumbar vertebra.
- This is a preganglionic sympathectomy because fibres supplying the vessels of the limb have their cell stations in the sacral ganglia which are not disturbed.
2. Omentoplasty has been tried in TAO patients. In most of these patients, vasodilator therapy and lumbar sympathectomy have been done with almost no relief of symptoms. In such cases, before a merciful amputation is done, omentoplasty is done.
- By careful division of the vascular arcade of the omentum, it can be lengthened based on one of the epiploic arteries, brought out of the laparotomy incision, tunnelled in the subcutaneous plane and can be brought up to the calf or even to the ankle joint level in some patients.
- The greater omentum is supposed to produce neovascularisation and thus help in the healing of the cutaneous ulcers. The effect seems to be temporary (Not done nowadays).
3. Conservative amputations should be done if the toes are gangrenous.
4. Below knee amputation8 is the last resort. It is indicated in severe rest pain cases where in all other modalities of treatment have failed. The risk of amputation after ten years of the disease is around 10%.
6. Surgery in atherosclerotic vascular disease
- The decision to revascularise the limb is taken after an angiography. The success of reconstruction depends upon a number of factors. They are given.
- Intermittent claudication alone is not an indication for surgery. Rest pain and gangrenous changes in the limb are definite indications for reconstruction with accepted mortality and morbidity.
- Surgery can be classified into surgery for aortoiliac disease and surgery for iliofemoral stenotic disease.
7Lumbar veins, if cut accidentally, retract and troublesome bleeding can occur from the inferior vena cava. Pressure packing, wait for 3–5 minutes and then see and ligate should be the policy.
8Students are requested not to tell this first as a treatment.
Prognostic Factors For Limb Revascularisation
- Severity of the disease
- Site of occlusion
- Presence of collaterals
- Age of the patient
- Presence of diabetes
- Angina pectoris
- Chronic smoking
- Fitness for anaesthesia
Summary Of The Revascularization Surgery
- Aortoiliac disease
- Aortobifemoral or aortofemoral graft and endarterectomy
- Iliofemoral disease
- iliofemoral bypass graft Balloon angioplasty
- Femoropopliteal disease
- Bypass graft
- Profunda artery stenosis
- Profundoplasty
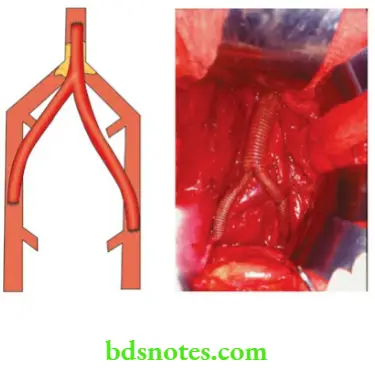
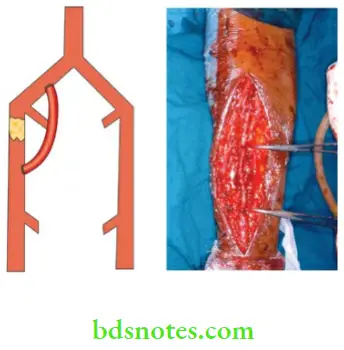
Aortoiliac Disease
It is treated by bypass grafts or endarterectomy.
- Bypass Grafts
- Usually, it is bilateral and it is treated by using aortobifemoral graft to bypass the stenosis. The graft either made from Teflon or dacron is used. It is also called y-graft or trouser graft. It typically has commonly 16 mm trunk and two 8 mm diameter limbs.
- In unilateral cases, unilateral graft is applied.
- Aortoiliac endarterectomy is indicated when the disease affects
- Short segment
- Big arteries like the aorta
- One artery.
Aortoiliac DiseaseTypes
Open endarterectomy: An arteriotomy is done first and the diseased intima, atheromatous plaque and the thrombus are removed. An arteriotomy incision can be closed directly or a vein patch graft is used to close the defect, so as to avoid narrowing.
2. Closed endarterectomy is indicated in a longer diseased segment. In this procedure, after an arteriotomy, a wire loop is used to strip out a core of atheroma by introducing it through the lower arteriotomy and removing the atheromatous plaque from the upper end.
However, the results of bypass grafts are better than endarterectomy and the modern tendency is to do bypass grafts.
Iliofemoral Stenotic Disease
- This can be repaired by a bypass graft which is sutured to the normal common iliac above and to the normal femoral artery below.
- If patients are unfit for a major vascular bypass, angioplasty can be done.
- In this procedure, a balloon catheter is inserted into the artery and it is inflated and its correct position is confirmed by radio-opaque markers which are present in the balloon. By inflation and dilation technique 2–3 times, the stenosed segment can be dilated.
- Any arterial stenosis can be dilated in angioplasty.
- The technique can be repeated if stenosis recurs. The procedure is done under local anaesthesia and is indicated in poor-risk patients.
- Ideally suitable for the iliofemoral segment, but not suitable for below knee stenosed vessels.
- Internal dissection, distal embolization, thrombosis and even rupture of vessels can occur.
- Recently, angioplasty combined with a Laser to drill holes through short stenosis has been employed.
Femoropopliteal Occlusion
- This is treated by using a graft extending from the femoral artery above to the popliteal artery below.
- Reversed long saphenous vein is better than other grafts.
- Dacron graft, polytetrafluoroethylene graft (PTFE), and human umbilical vein graft are the other grafts.
Profunda Artery Stenosis
Significant occlusion of the profunda is demonstrated by oblique views in an arteriography. If there are no significant vessels available below the stenosis for reconstruction, profundoplasty is considered. It is done by using a patch of Dacron or vein to widen the origin of this vessel after doing an endarterectomy.
Acute Arterial Occlusion
Sudden occlusion of an artery is commonly due to emboli, increased incidence of road traffic accidents, falls or war injuries. Trauma to the artery also produces occlusion.
Embolic Occlusion
- This commonly occurs in the peripheral arteries such as the common iliac, femoral and popliteal.
- An embolus is a foreign body to the bloodstream, it gets lodged in a vessel produces obstruction and clinically manifests as severe ischaemia or gangrene, resulting in Critical Limb Ischaemia (CLI).
What is Critical Limb Ischaemia (CLI)?
It is defined as persistently recurring ischaemic rest pain requiring regular, adequate analgesia for more than 2 weeks or ulceration or gangrene of the foot or toes with an ankle pressure of < 50 mmHg or a toe systolic pressure of < 30 mmHg.
Atherosclerotic vascular disease, thromboangitis obliterans, acute embolic ischaemia and even diabetes etc. at one stage or another can present as CLL
Critical Limb Ischaemia Clinical Features
- No previous history suggestive of intermittent claudication
- Sudden dramatic symptoms which are described in the form of 5P’s
- Pain
- Pallor
- Paresis
- Pulselessness
- Paraesthesia
- Pain is severe, unbearable, burning or bursting type.
- The limb is pale, and cold and superficial veins are collapsed.
- Paresis: Depending on the level of occlusion, the function of the limb is lost. Movement of the toes becomes difficult, followed by total paralysis.
- Pulselessness: Characteristically, peripheral pulses below the level of embolism are not palpable.
- Altered sensation in the limb.
-
- If left untreated, necrosis of the muscles followed by gangrene of the limb can occur within a few hours (6–24 hours).
- A cardiac examination may reveal the source of the emboli.
Causes Of Emboli
- Mural thrombus following a myocardial infarction (Ml)
- Mural thrombus due to mitral stenosis and atrial fibrillation
- Atheromatous plaque
- Aneurysm
- Emboli from myxoma of the heart
- Valve vegetations
Emboli Pathology
Investigations
- Peripheral circulation should be assessed by Doppler ultrasound, which is an excellent noninvasive investigation to judge the severity, level, position, and length of superficial femoral artery stenosis.
- Digital subtraction angiography is indicated in aortoiliac lesions.
Emboli Treatment
1. Angioplasty: Percutaneous transluminal angioplasty (PTA) is indicated in short stenotic lesions in large vessels, for example, iliac and femoropopliteal lesions.
- First, the balloon catheter is introduced percutaneously over a guidewire across the lesion. Under fluoroscopic control, the balloon is dilated, till satisfactory widening of lumen is achieved.
- Relatively safe and simple procedure.
- Immediate intravenous infusion of heparin (5000-10000 units) is necessary to reduce the extension of the thromboembolism.
2. Emergency embolectomy is done under G/A or local anaesthesia either by direct arteriotomy incision removing the clot or by using a Fogarty balloon catheter to remove an embolus from a vessel remote from arteriotomy.
3. Thrombolysis: It is indicated in acute or acute or chronic ischaemia. A fine lysis catheter is passed percutaneously into the blocked vessel. Streptokinase is infused at a rate of 5000 I.U. in 10 ml per hour. It will reopen the occluded lumen within 24 hours. A repeat angiogram is necessary to check for patency.
For contraindications see.
Pulmonary Embolism Symptoms
Peripheral Aneurysms
- These can affect the popliteal artery, femoral artery iliac artery, etc., 70% of peripheral aneurysms affect the popliteal artery, and two-thirds of them are bilateral.
- However, students should realise that aneurysms are uncommon (rare) causes of lower limb ischaemia. Early diagnosis and effective treatment is essential to save the limb.
Contraindications To Thrombolytic Therapy
Absolute
- Recent major bleeding
- Recent major surgery
- Recent ophthalmologic procedure
- Recent stroke
Relative
- Active peptic ulcer disease
- Pregnancy
- Uncontrolled hypertension
- Coagulation abnormalities
Pulmonary Embolism Symptoms
Popliteal Aneurysms
They are the most common peripheral aneurysms for the following reasons:
- Turbulence beyond stenosis at the adductor magnus hiatus
- Repeated flexion at the knee.
Popliteal Aneurysms Clinical features
- They affect elderly patients and atherosclerosis is the cause. One-third of the cases are associated with aortic aneurysm.
- The age at presentation is 65 years
- Striking preponderance in males. Male female ratio is 20–30:1. Presents as a swelling behind the knee
- Dull aching pain is common
- Severe bursting pain indicates rapid expansion and impending rupture.
- Pulsatile, tense, cystic, fluctuant swelling behind the knee, in the popliteal fossa in the line of the popliteal artery.
- Size diminishes on extending the knee as the aneurysm is deep to popliteal fascia.
- Proximal compression test: On occluding the femoral artery proximally the swelling may diminish in size.
Popliteal Aneurysms Investigations
- Duplex ultrasonography is the investigation of choice which can measure diameter and determine the extent of mural thrombus.
- Angiography can demonstrate the extent of the involved segment to look for patency and quality of run-off vessels.
Popliteal Aneurysms Complications
- Thrombosis causes severe acute ischaemia of the lower limb (incidence—40%)
- Embolization causes ischaemic ulceration of the lower limb.
- Rupture causes pain and haematoma. (rare—2–5%)
- Compression on the popliteal vein causes pain, tenderness and swelling of the leg.
- Compression on the lateral peroneal nerve causes foot drop, due to paralysis of the peronei and the extensors of the foot.
Popliteal Aneurysms Treatment
- Proximal and distal ligation of the artery followed by reversed saphenous vein bypass graft is the treatment of choice. This method results in total obliteration of the sac with revascularisation of the limb.
- Excision of the sac is better avoided because of the chances of injury to the popliteal vein and nerves. Lateral popliteal nerve injury causes foot drop and tibial (medial popliteal) nerve injury causes thinning of the calf region, inability to plantar flex the ankle and clawing of the toes due to paralysis of the intrinsic muscles of the foot.
Miscellaneous Ainhum
It affects those who do not use footwear or walk barefoot. It starts as a fissure at the level of the interphalangeal joint of a toe, usually fifth. Repeated trauma of a minor degree may be present. The tissue becomes a fibrous band resulting in tight constriction and necrosis. If it continues it may land with autoamputation.

- The division of a band or early Z-plasty may be needed to avoid amputation.
- Thrombolysis with catheter in situ, in early cases.
Frostbite
- It occurs due to too much exposure to cold weather.
- High altitudes with excessive cold precipitate vasospasm and damage to the blood vessel wall. It causes sludging of blood and thrombosis.
- Malnutrition and the ageing process are the other precipitating factors. Severe burning pain, discolouration of the foot, and development of blisters suggest gangrene is imminent.
Frostbite Treatment
- Slow warming of the parts and protection with cotton wool. Analgesics, antibiotics.
- Paravertebral injection into the sympathetic chain helps in a few patients.
- Elevation of the foot to reduce oedema.
- Frank cases of frostbite with gangrene require conservative amputation.
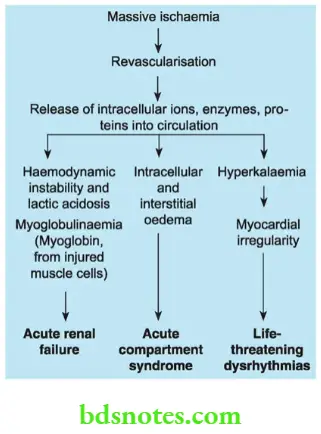
Reperfusion Injuries Or Syndrome
- This dangerous event follows the revascularisation of limbs, resulting in acute compartment syndrome with pressure beyond capillary pressure (30 mmHg).
- The sequence of events is as follows.
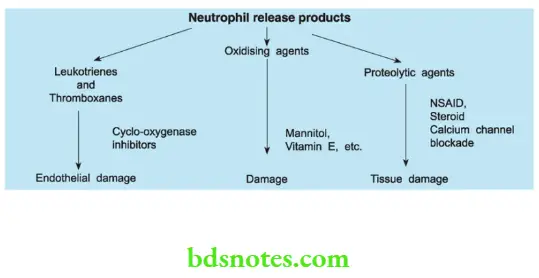
- However, most of the injury is believed to be due to oxygen-derived free radicals—the most important ones include superoxide radicals, hydrogen peroxide and hydroxyl radicals. These radicals attach unsaturated bonds of fatty adds within the phospholipid membranes resulting in damage.
Reperfusion Injuries Management
- Diagnosis by severe pain in the limb, oedema of the leg, muscle tenderness, and raised intra-compartmental pressure measured by transducer cannula.
- Treated by multiple fasciotomy.

Leave a Reply