Question 1. Write a short note on carbuncle.
Or
Write in short about carbuncle.
Or
Write brief notes on carbuncle.
Or
Define, and describe clinical features and principles of treatment of carbuncle.
Answer. The word meaning of carbuncle is charcoal. It is caused by extensive infectious gangrene of the adjacent hair follicle and subcutaneous tissue by Staphylococcus aureus.
- It commonly occurs in diabetic patients.
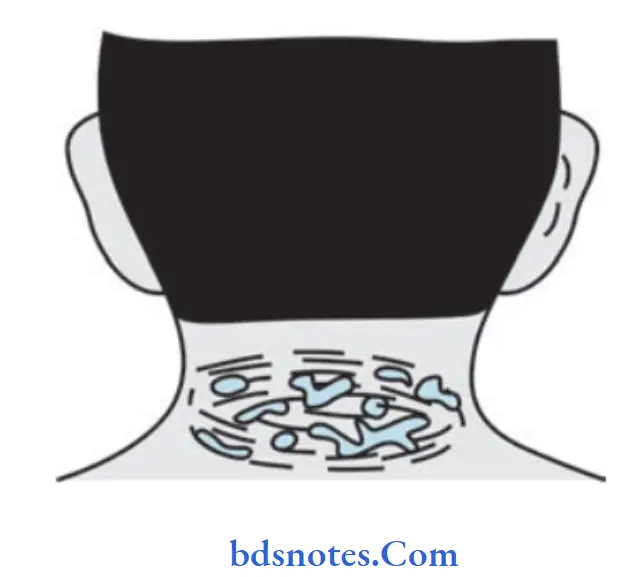
- The Nape of the neck is the most common site followed by the back and shoulder region. The skin of the site is coarse and has poor vascularity.
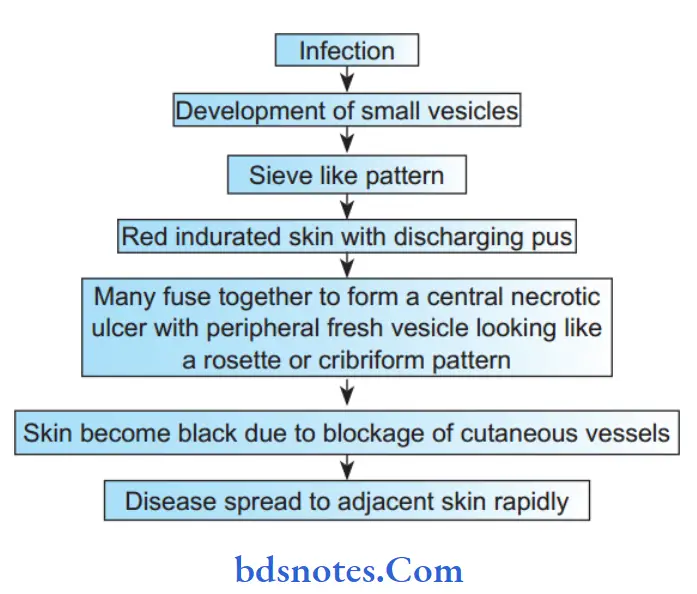
Carbuncle Pathology
Carbuncle Clinical Features
- It is common in diabetics after 40 years of age
- The surface is red and looks like a red-hot coal.
- Symptoms like fever with chills.
- Severe pain and swelling in the nape of the neck and back.
- The surrounding area is indurated.
- The skin on the center of the carbuncle softens and a peripheral satellite vesicle appears, if rupture discharging pus and giving rise to a cribriform appearance.
- Later development of large crateriform ulcer with center slough.
Carbuncle Complications
- Worsening diabetic status resulting in diabetic ketoacidosis
- Extensive necrosis of skin overlying carbuncle. Hence, it is included under acute infective gangrene.
- Septicemia and toxemia.
Carbuncle Management
The principles of treatment of carbuncle are:
- Control of diabetes
- Parenteral antibiotics
- Surgical management:
- Diabetes control preferably with injectable insulin.
- Appropriate parenteral antibiotics are given till complete resolution occurs.
Most strains of Staphylococcus aureus are sensitive to cloxacillin, flucloxacillin, erythromycin, and some of the cephalosporins.
However, methicillin-resistant Staphylococcus aureus (MRSA) is resistant to the drugs mentioned above.
They are sensitive only to expensive drug vancomycin which has to be given intravenously. - Improve the general health of the patient
- If the carbuncle does not show any softening or if it shows evidence of healing, it is not incised. It can be left open to the exterior or saline dressings are applied to reduce edema. Complete resolution may take place within l0–l5 days.
Question 2. Write the management of carbuncle.
Or
Carbuncle Treatment
Answer. Management of Carbuncle
- Diabetes control preferably with injectable insulin.
- Appropriate parenteral antibiotics are given till complete resolution occurs.
Most strains of staphylococcal aureus are sensitive to cloxacillin, flucloxacillin, erythromycin, and some of the cephalosporins.
However, methicillin-resistant Staphylococcus aureus (MRSA) is resistant to the drugs mentioned above.
They are sensitive only to expensive drug Vancomycin which has to be given intravenously. - Improve the general health of the patient
- If the carbuncle does not show any softening, or if it shows evidence of healing, it is not incised.
It can be left open to the exterior or saline dressings are applied to reduce edema.
Complete resolution may take place within l0-l5 days.
Carbuncle Surgical Management
- Surgery is required when there is pus.
The cruciate incision is preferred because of multiple abscesses and extensive subcutaneous necrosis.
Edges ofthe skin flap are excised, pus is drained, loculi are broken down, the slough is excised, and the cavity is treated with antiseptic agents.
Once the wound granulates well, skin grafting may be required.
Question 3. Describe the bacteriology of perimandibular space infection, its spread, and management.
Answer.
Submandibular, sublingual, and submental spaces are collectively called perimandibular spaces.
When the perimandibular spaces are involved in an infection, it is known as Ludwig’s angina.
Bacteriology
- As Ludwig’s angina is of dental origin streptococci or mixed oral flora are the most commonly reported microorganisms.
- The presence of staphylococci, E. coli, Pseudomonas, and anaerobes including Bacteroides and Peptostreptococcus, Prevotella species have also been isolated.
- The role of anaerobes as primary or synergistic organisms should not be omitted in the culture.
Spread of Perimandibular Space infection
- Infection from a lower third molar reaches the submandibular space.
- From here it spreads along the submandibular salivary gland above the mylohyoid muscle to reach the sublingual space.
- From one side of the sublingual space, it moves across the genioglossus muscles and reaches the sublingual space on the other side. It can then cross over the mylohyoid muscle and reach the opposite side submandibular space.
- The submental space gets involved via the lymphatics.
Since it is cellulitis and not an abscess, it does not remain localized but rapidly spreads along the fascial planes and tissue spaces. - After involving the three spaces, the cellulitis spreads within the substance of the tongue posteriorly along the course ofthe sublingual artery in the cleft between the genioglossus and geniohyoid muscles. This reaches the region of the epiglottis producing edema and inflammation of the laryngeal inlet. This causes severe airway compromise.
- Also from the submandibular space, it can pass along the investing layer of the deep cervical fascia all along the anterior aspect of the neck to the clavicle and continue into the mediastinum.
- Communication of the submandibular space with the pterygomandibular, masseteric, and lateral pharyngeal spaces causes trismus and further enhances airway compromise.
Perimandibular Space Infection Management
The main aspects of management are:
- Airway maintenance
- Parenteral antibiotics
- Surgical decompression of tissues
- Hydration of patient
- Removal of cause
Perimandibular Space Infection Airway Maintenance
- Edema of the glottis is what leads to airway obstruction and death of the patient, if untreated. Maintaining a patent airway is thus of prime importance.
- Intubation is done by an experienced anesthetist.
- Bulging of the posterior pharyngeal wall makes intubation difficult. Perforation may lead to aspiration of pus if an endotracheal tube is forced in blindly.
- A tracheotomy or cricothyroidotomy may be advisable.
Tracheostomy is usually difficult because the anatomical landmarks on the neck are not easily identifiable with the swelling.
Perimandibular Space infection Parenteral antibiotics
- Penicillin is the antibiotic of choice.
- Others such as Amoxicillin and cloxacillin may also be used.
- Metronidazole is given against anaerobic organisms.
- Gentamycin can also be given along with penicillin for coverage of Pseudomonas.
Perimandibular Space infection Surgical decompression
- It is usually preferred under LA instead of GA. The main aim is to relieve the pressure within the tissues for the edema to reduce. Also, the pressure within the tissues compresses the blood vessels preventing the penetration of antibiotics in the area of interest. Thus decompression improves vascularity and potentiates the action of antibiotics.
- If there is pus, it provides a channel for the drainage of pus.
- Pus obtained from a drainage may be sent for culture and sensitivity testing.
- A decrease in edema reduces respiratory embarrassment.
- Ethyl chloride spray may be used or LA may be injected locally in the area of incision.
- Bilateral submandibular incisions with a midline submental incision may be placed.
- Blunt dissection through the skin, superficial fascia, platysma, deep fascia, and mylohyoid muscle is done to reach the sublingual space. The sublingual space may alternatively be drained intraorally by an incision in the floor of the mouth if the mouth opening is adequate.
- A drain is inserted through all these layers and stabilized.
There may be no pus at all in most cases of Ludwig’s angina. Pus may only be seen at later stages.
A loose dressing is placed which is changed every day after careful cleaning of the drain.
Perimandibular Space Infection Hydration of the Patient
- Pyrexia and dysphagia may lead to dehydration of the patient.
- It is necessary to put the patient on IV fluids.
Removal Of Cause
Once the patient is stabilized and the trismus relieved to an extent, the offending tooth may be removed
Question 4. Describe pathology, clinical features, treatment, and complications of alveolar abscess.
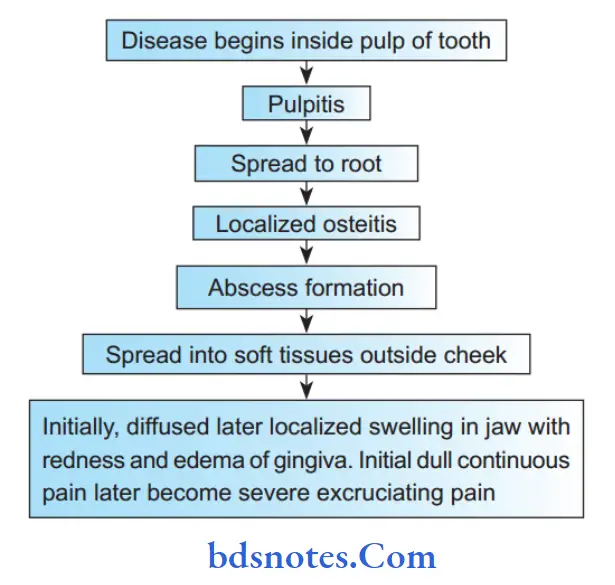
Answer. Alveolar abscesses occur due to the spread of infection from the root of the tooth in periapical tissue. Initially, it forms a periapical abscess which later spreads through the cortical part of bone into soft tissues and forms an alveolar abscess.
Alveolar Abscess Pathology
Alveolar Abscess Clinical Features
- It is a common odontogenic infection and constitutes 2% of apical radiolucencies.
- Due to an acute abscess, there is pain in the affected tooth.
- Localized swelling and an erythematous change in overlying mucosa are present.
- The affected area of the jaw may be tendered during palpitation.
- Pain aggravates during percussion and when pressure is applied to the opposing tooth.
- The application of heat intensifies pain, whereas application of cold relieves pain temporarily.
- Pus discharging sinus often develops on alveolar mucosa over the affected root apex and sometimes on the skin overlying the jaw bone.
- Infection from acute periapical abscess often spreads to facial spaces, leading to space infections.
Alveolar Abscess Treatment
- Rest is given
- Incision and drainage under general anesthesia
- Appropriate antibiotics
- 4 fluids to correct dehydration.
- Extraction of the tooth at a later period
- Extraction of sinus when required.
Alveolar Abscess Complications
- Septicemia.
- Spread of infection into other spaces such as parapharyngeal spaces; sublingual and submandibular spaces causing Ludwig’s angina; edema of epiglottis and respiratory distress; spread to pterygoid space and along pterygoid muscles through emissary vein leading to cavernous sinus thrombosis; upper canine tooth abscess spreading to corner of eye causing angular vein thrombophlebitis which further progress to cavernous sinus thrombosis; sub masseteric abscess.
- Lower incisor abscess can cause abscess in the chin and median mental sinus; and chronic osteomyelitis of the jaw with discharging sinuses.
Osteomyelitis is common in the mandible horizontal process near the mentum, presenting with pain, swelling, discharging sinuses, bone thickening, loose teeth, and trismus. Sequestrum is commonly seen.
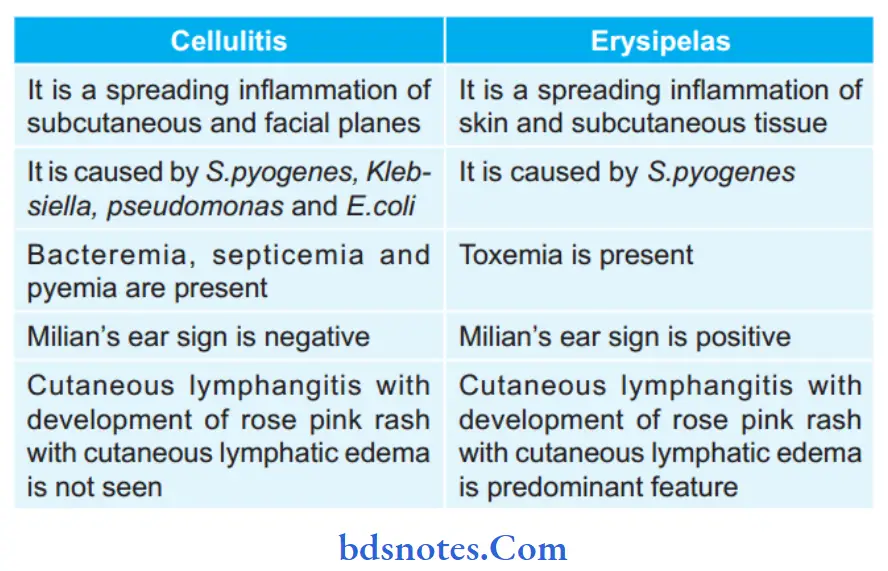
Question 5. Enumerate differences between cellulitis and erysipelas.
Answer.
Question 6. Write a short note on Erysipelas.
Answer. Erysipelas is an acute spreading inflammation of the skin and subcutaneous tissues that is caused by Streptococcus pyogenes and is associated with severe lymphangitis.
Infection occurs through small scratches or abrasions and spreads rapidly causing toxemia.
Erysipelas Clinical Features
- It occurs commonly in children and old people.
- Sites commonly affected are the face, eyelids, scrotum in infants, and the umbilicus.
- There is the presence of a rose pink rash with a raised edge and its consistency is of a button hole.
- Features of toxemia are commonly present.
- The redness of the lesion becomes brown and later on yellow with the presence of vesicles.
- Discharge from the lesion is serious.
- There is the presence of edema of the face and orbit.
- When erysipelas occur on the face involves pinna since it is cuticular lymphangitis.
This is called Milian’s ear sign positive.
This sign diffrentiate erysipelas from cellulitis. - Tender, regional lymph nodes are palpable.
Erysipelas Complications
- Toxemia and septicemia.
- Gangrene of skin and subcutaneous tissue.
- Lymphoedema of the face and eyelids occurs due to lymphatic obstruction.
- Abscess pneumonia and meningitis may develop.
Erysipelas Treatment
Injection of crystalline penicillin 10 lakh units 6 hourly IM/IV for 5 to 10 days.
Question 7. Name etiological agent, pathognomic diagnostic feature, and treatment (only modalities) of erysipelas.
Answer.
Erysipelas Etiological Agent
Beta hemolytic Streptococcus pyogenes
Erysipelas Pathognomic Diagnostic Feature
When erysipelas occur on the face, it involves the pinna because
erysipelas a cuticular lymphangitis. It is described as Milian’s ear sign positive.
This sign diffrentiates cellulitis of face from facial erysipelas.
In cellulitis of the face, the pinna does not get involved because of the close adherence of skin to cartilage.
Erysipelas Treatment (Only Modality)
Antibiotic treatment should be given.
Question 8. Define, and describe clinical features and principles of treatment of Cavernous Sinus Thrombosis
Answer. In cavernous sinus thrombosis, the infection from the maxillary anterior region is carried via facial, angular, and nasofrontal veins to the superior ophthalmic veins which enter the cavernous sinus via superior orbital fissure.
Veins of the dangerous areas of the face are valveless and allow retrograde infection in the form of cavernous sinus thrombosis.
Cavernous Sinus Thrombosis Clinical Features
- The patient had sinusitis or midfacial infection which was manipulated.
- Before ocular symptoms, there is the presence of headache, fever, and malaise.
- Patient complaints of orbital fullness and pain along with visual disturbances.
- If the complaints remain untreated for a long time symptoms get spread to other eyes and it can be fatal too.
- Signs of venous congestion are present, i.e. chemosis, edema of the eyelid, and periorbital edema.
- Signs of retrobulbar pressure are present such as exophthalmos, ophthalmoplegia, and loss of corneal reflex
- Meningeal signs are present, i.e. nuchal rigidity, Brudzinski’s sign.
- Systemic signs are also present such as chills, fever, delirium, and shock.
Cavernous Sinus Thrombosis Principles of treatment
- Aggressive antibiotic therapy with broad-spectrum antibiotics.
- Anticoagulation is done by giving heparin.
- Steroids are given to reduce the inflammation.
- The primary source of the infection should be eliminated.
Question 9. Describe etiopathogenesis and the principle of management of acute Pyogenic Abscess.
Answer. Pyogenic *abscess: It is the most common form of an abscess, subcutaneous, deep or it can occur within the viscera such as the liver or kidney.
Pyogenic Abscess Etiopathogenesis
- It is usually produced by staphylococcal infections.
- The organism enters in the soft tissue by an external wound, minor or major.
- It can also be due to hematogenous spread from a distant focus like tonsillitis or carious tooth, etc.
- Pyogenic abscess can also be due to cellulitis.
- Following an injury, there is inflammation of the part brought about by the organisms.
- The result is the production of pus, which is composed of dead leukocytes, bacteria, and necrotic tissue.
- The area around the abscess is encircled by firin products and it is infiltrated with leukocytes and bacteria.
It is called a pyogenic membrane.
Pyogenic Abscess Management
- When pus is not localized: Conservative treatment is needed.
Proper antibiotics and anti-inflammatory agents. - When pus is localized: There is a golden rule that “Pus should be drained”.
Incision and drainage(IandD) under general anesthesia.
- General anesthesia is preferred because of the presence of infection.
Pyogenic Abscess Infection:
Pyogenic Abscess Free or liberal incision:
- It is made on the most prominent part to avoid damage to healthy tissue. The incision should be adequate for easy drainage of pus.
- In case, if nerve and vessels are present below or surrounding the abscess, an incision parallel to the nerve and vessel is given to avoid these structures.
Pyogenic Abscess Incision by Hilton method:
- This method is used when there are plenty of nerves and vessels around the abscess cavity, which could be injured.
- In this method, an incision is given on the most prominent and most dependent part.
- A pair of artery forceps or sinus forceps is introduced and then the blades are open.
It is swiped in the abscess cavity to break abscess loculi. - After the removal of forceps, figer is introduced to explore the abscess cavity.
Pyogenic Abscess Counter Incision:
- When a prominent part is not the most dependent
part, a counter incision is made on the most dependent part to facilitate pus-drainage under gravity.
In the case of counterintuition, sinus forceps are introduced on the most dependent part rather than the most prominent part.
Pyogenic Abscess Drainage:
- A corrugated rubber drain is usually used for drainage of pus.
- It is removed when pus stops coming out.
Follow-up: Proper antibiotics and analgesics are given.
Question 10. Describe the clinical features and treatment of Acute Abscess.
Answer.
Acute Abscess Clinical Features
- Fever with chills and rigors.
- Localized swelling which is smooth, soft, and fluctuant.
- Pus is visible
- Throbbing pain and pointing tenderness
- Brawny induration around
- Redness and warmth with restricted movement around a joint
- Rubor (redness), Dolor (pain), calor (warmness), tumor (swelling), and function laesa (loss of localized and adjacent tissue/joint function) are quite obvious.
Question 11. Write short notes on various types of abscesses and Hilton’s method of Drainage.
Answer. An abscess is a pathological thick-walled tissue cavity filled with necrotic tissue, bacteria, and leukocytes caused by a localized collection of purulent inflammatory tissue and suppuration from infection in a buried tissue, organ, or confined space.
Hilton’s method of Drainage – Types Of Abscess
- Pyogenic abscess: It is produced by staphylococcal bacteria.
Organisms enter soft tissues by an external wound. It can be subcutaneous, deep or it can be a viscera. - Pyemic abscess: It is due to pus-producing organisms in circulation. It is the systemic effect of sepsis. It commonly occurs in diabetics and patients receiving chemotherapy and radiotherapy.
- Cold abscess: It means an abscess with no signs of inflammation. It is caused due to tuberculosis.
Hilton’s Method of drainage
- Initially, broad-spectrum antibiotics are started.
- Under general anesthesia or regional block anesthesia after cleaning and draping, the abscess is aspirated and the presence of pus is confirmed.
- Skin is incised adequately in a line parallel to the neurovascular bundle.
- The pyogenic membrane is opened using sinus forceps and all loculi are broken up.
- The abscess cavity is cleared of pus and washed with saline.
- A drain is placed
- The wound is not closed, wound is allowed to heal and granulate.

Leave a Reply