Acute Infections
Since the time surgery has evolved as a speciality, infection and haemorrhage have been recognised as two well-known enemies of surgeons. Over a period of time, many newer antibiotics have come into existence. However, infection still dominates and it is one of the major causes of mortality and morbidity in a patient who has a ‘benign disease’. This is the sad part of the disease. Hence, it is important to diagnose and treat infections effectively as early as possible.
Read And Learn More: Clinical Medicine And Surgery Notes
Cellulitis
Cellulitis is a spreading subcutaneous inflammation caused by haemolytic streptococcus. Streptococci produce hyaluronidase and streptokinase. The net result is that the inflammatory exudate spreads in the subcutaneous and fascial planes resulting in a gross swelling of the affected part. Wherever there is loose subcutaneous tissue as in the scrotum or loose connective and interstitial tissue as in the face, or forearm, it spreads fast.
Cellulitis Sources of Infection
- Injuries—minor or major
- Graze or scratch
- Snakebite, scorpion bite, etc.
Precipitating factors
- Diabetes
- The low resistance of an individual.
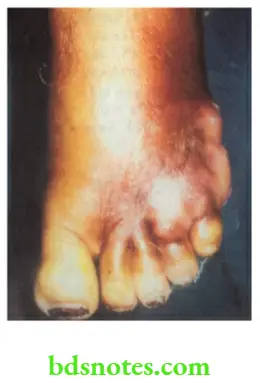
Cellulitis Common Sites
- Lower limbs
- Face
- Scrotum.
Clinical Features
- The affected part shows evidence of inflammation such as redness and itching followed by diffuse swelling. Skin is stretched and shiny. Pain, fever, and toxaemia follow later. It is differentiated from an abscess by the features mentioned below.
- In untreated cases, suppuration, sloughing and gangrene can occur.
Cellulitis Treatment
- Bed rest with legs elevated. This reduces the oedema of the legs.
- Glycerine MgSO4 dressing reduces oedema of part by osmotic effect.
- Diabetes mellitus, if present, is treated with insulin usually given subcutaneously.
- Appropriate antibiotics such as Injection Crystalline Penicillin 10 lakh units, intramuscular (IM) or intravenous (4), 6th hourly for 5–7 days or Ciprofloxacin 500 mg twice a day can be given.
- Anti-snake venom is given in snake bite cases.
Cellulitis Complications
- Cellulitis can turn into an abscess which needs to be drained.
- Necrotising fasciitis: Certain highly invasive strains of Streptococcus pyogenes can cause extensive necrosis of skin, and subcutaneous tissues and may result in necrotising fasciitis. It is treated by debridement followed by skin grafting at a later date.
- Toxaemia and septicaemia: Streptococcal toxic shock syndrome can result if exotoxins are produced by the organisms.
Cellulitis
- No edge (diffuse swelling)
- No limit
- No pus
- No fluctuation
Abscess
- Well-circumscribed has an edge
- Limit is present
- Pus is present
- Fluctuation is positive
Cellulitis Precipitating Factors
- Caries tooth
- Cancer of the oral cavity
- Calculi in the submandibular gland
- Chemotherapy patients
- Cachexia
- Chronic disease—diabetes
4. Cellulitis can precipitate ketoacidosis in a patient who has diabetes
Ludwig’S Angina
It refers to cellulitis of submental and submandibular regions combined with inflammatory oedema of the mouth. Virulent streptococcal organisms are responsible for infection surrounding the submandibular region. Anaerobes also play a major role.
Ludwig’S Angina Clinical Features
- An elderly patient presents with diffuse swelling in the submandibular and submental regions (Brawny oedema).
- Oedema of the floor of the mouth, as a result of which the tongue is pushed upwards resulting in difficulty in swallowing.
- High-grade fever with toxicity
- Putrid halitosis is characteristic of this condition.
Ludwig’S Angina Treatment
- Rest and hospitalisation
- Appropriate antibiotics
- Intravenous fluids to correct the dehydration and Ryle’s tube feeding
- If it does not respond to conservative treatment, surgical intervention is recommended.
Ludwig’S Angina Surgery
Under general anaesthesia, a 5–6 cm curved incision is made below the mandible in the submandibular region over the most prominent part of the swelling. The submandibular gland is mobilised, the mylohyoid muscle is divided and the pus is drained. Even if pus is not found, the oedematous fluid comes out greatly improving the condition of the patient. A wound is closed with loose sutures after irrigating the cavity with antiseptic agents and a drainage tube is kept in place.
Ludwig’S Angina Complications
- Mediastinitis and septicaemia
- Oedema of the glottis due to the spread of the cellulitis via a tunnel occupied by stylohyoid to the submucosa of the glottis
Abscess
An abscess is a localised collection of pus (dead and dying neutrophils with proteinaceous exudate).
Abscess Classification
- Pyogenic abscess: It is the commonest form of an abscess. It can be subcutaneous or deep. It can occur within the viscera such as the liver or kidney, etc. In this chapter, pyogenic abscess refers to soft tissue abscess.
- Pyaemic abscess: It occurs due to the circulation of pyaemic emboli in the blood (pyaemia).
- Cold abscess: Usually refers to tubercular abscess either due to involvement of lymph nodes or involvement of spine.
Pyogenic Abscess
It is usually produced by staphylococcal infections. The organisms enter soft tissues by an external wound, minor or major. It can also be due to haematogenous spread from a distant focus such as tonsillitis or caries tooth, etc. Pyogenic abscess can also be due to cellulitis.
Pathophysiology
Following an injury, there is inflammation of the part brought about by the organism such as Staphylococcus. Pathological events are summarised below.
Pathological events during inflammation
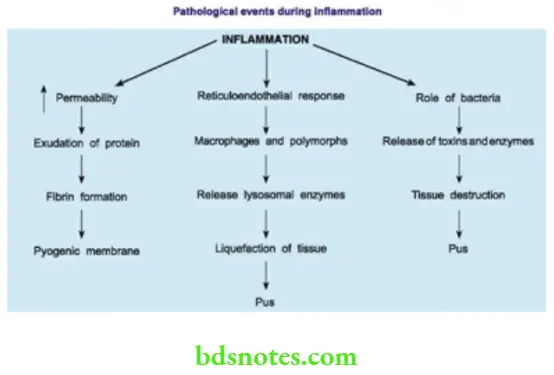
The end result is a production of pus which is composed of dead leukocytes, bacteria and necrotic tissue. The area around the abscess is encircled by fibrin products and it is infiltrated with leukocytes and bacteria. It is called a pyogenic membrane.
Pyogenic Abscess Symptoms
The patient feels ill and complains of throbbing pain at the site. Throbbing pain is indicative of pus and is due to pressure on the nerve endings by the pus. Fever, with or without chills and rigours can be present.
Pyogenic Abscess Signs
- Calor-heat: The affected part is warmer due to a local rise in temperature.
- Rubor-redness: It is due to inflammation resulting in hyperaemia.
- Dolor-pain: An abscess is extremely tender.
- Tumor-swelling: It consists of pus. It is tensely cystic with surrounding brawny oedema.
- Loss of function: The function of the part is impaired, due to pain.
- Fluctuation can be elicited. However, in a deep-seated abscess, it may be negative, as in the thigh.
Pyogenic Abscess Treatment
An untreated abscess tends to point spontaneously towards an area of least resistance —nearest an epithelial surface, for example. skin, gut, oral cavity, etc. However, deep-seated abscesses—such as breast abscesses, may cause much tissue destruction before pointing.

Incision and drainage (I and D) under general anaesthesia. General anaesthesia is preferred because in the presence of infection, local anaesthesia may not act and it is difficult to break all the loculi of an abscess without causing pain.
Pyogenic Abscess Procedure
- A stab incision is made over the most prominent (pointing) part of an abscess. The pus which comes out is collected and sent for culture and sensitivity. A sinus forceps or a finger is introduced within the abscess cavity and all the loculi are broken down.
- Fresh bleeding which is seen is an indication of the completeness of the procedure. The abscess cavity is irrigated with mild antiseptic agents like iodine solution or hydrogen peroxide. Hydrogen peroxide acts by liberating nascent oxygen.
- H2O→H2O+[O]
- Nascent oxygen bubbles out and helps in separating the slough. The cavity, if large may need to be packed with roller gauze dipped in iodine solution which is removed 1–2 days later.
- Roller gauze packing prevents the premature closure of the skin, thus facilitating the healing to take place from the depth of the cavity by granulation tissue.
- With appropriate antibiotics and proper dressings, the wound heals within 5–7 days. The antibiotic of choice is cloxacillin for staphylococcus abscesses. Dosage: 500 mg 6th hourly for
- 5–7 days.
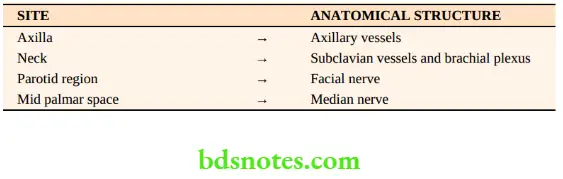
- Modified Hilton’s method for I & D. This method is followed when an abscess is situated in the vicinity of important anatomical structures like vessels or nerves.
- In this method, skin and superficial fascia are incised, instead of a stab incision, followed by opening the abscess by sinus forceps, so as to avoid damage to vital structures like vessels and nerves.
Pyogenic Abscess Differential Diagnosis
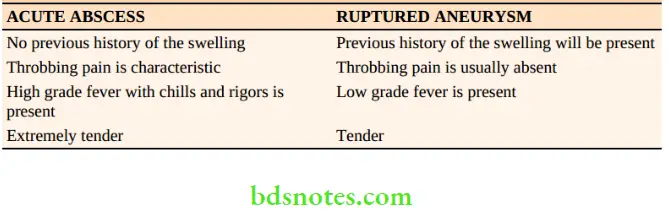
- A ruptured aneurysm can present as a subcutaneous abscess with pain, redness and a local rise in temperature. There may be leukocytosis also. A ruptured vertebral artery aneurysm in the posterior triangle and a popliteal artery aneurysm in the popliteal fossa have been incised, mistaking them for an abscess.
Caution: When in doubt, before incising an abscess, aspirate with a wide-bore needle. - Soft tissue sarcoma in the thigh can be confused for a deep-seated abscess. However, throbbing pain, high-grade fever with chills and rigours and short duration of the swelling clinches the diagnosis of an abscess.
Antibiotic
It is antibiotic-induced swelling (oma). However once an abscess is formed, antibiotics seldom effect a cure if given because pus gets partially sterilised. Antibiotics also produce fibrosis, resulting in thickening of the abscess wall. Clinically, this may result in a hard lump. Sites of antibioma are breast, thigh, ischiorectal fossa, etc. Antibiotics in the breast may mimic carcinoma of the breast.
Pyaemic Abscess
This is due to pus-producing organisms in the circulation (pyaemia). It is the systemic effect of sepsis. It commonly occurs in diabetics and patients receiving chemotherapy and radiotherapy. Pyaemic abscess is characterised by the following features.
- They are multiple
- They are deep-seated
- Tenderness is minimal
- Local rise in temperature is not present
Hence, it is called a nonreactive abscess to differentiate it from a pyogenic abscess. This is treated by multiple incisions over the abscess site and drainage (like a pyogenic abscess) along with systemic antibiotics.
Cold Abscess
- Even though it is a chronic abscess due to a chronic disease (tuberculosis), for the completeness of the chapter on abscess and for the convenience of reading, it is discussed here.
- A cold abscess means an abscess which has no signs of inflammation. Usually, it is due to tuberculosis, for example. following tubercular lymphadenitis or due to tuberculosis of the spine.
- However, other chronic diseases like leprosy, actinomycosis, Madura foot, etc. also produce abscesses which are ‘cold’ in nature. In this chapter, a cold abscess due to tubercular lymphadenitis in the neck is discussed.
Cold Abscess—Causes
- Tuberculosis
- Actinomycosis
- Leprosy
- Madura’s foot
Tuberculous Lymphadenitis
- Etiopathogenesis: In 80% of the cases, mycobacteria pass through tonsillar crypts and affect tonsillar node or jugulodigastric group of nodes, in the anterior triangle of the neck.
- In 20% of the cases, lymph nodes in the posterior triangle are affected due to the involvement of adenoids.
- Rarely, infection can spread from tuberculosis at the apex of the lung. Organisms directly penetrate Sibson’s fascia (suprapleural membrane) and can cause enlargement of the supraclavicular node.
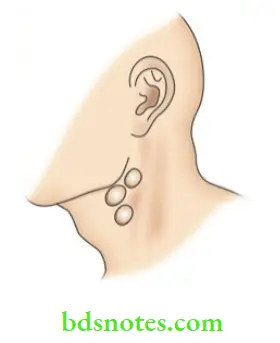
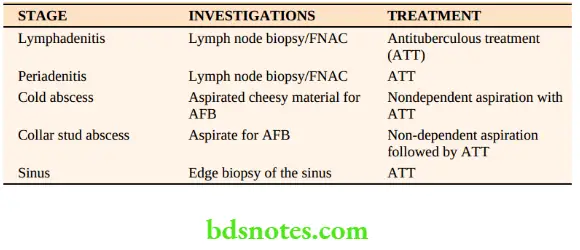
Stages Of Tuberculous (TB) Lymphadenitis
Stage of Lymphadenitis
- Common in young adults between 20 and 30 years
- Upper anterior deep cervical nodes are enlarged
- Non-tender, discrete, mobile, firm lymph nodes are palpable.
Stage of periodontitis/Stage of matting
- Results due to involvement of capsule
- Nodes move together
- Firm, non-tender
- Matting1 is the pathognomonic of tuberculosis.
- Other rare causes of matting are chronic lymphadenitis and anaplastic variety of lymphoma.
Stage Of Cold Abscess
It occurs due to caseation necrosis of lymph nodes resulting in fluctuant swelling in the neck.
Clinical features of cold abscess in the neck are:
- No local rise in temperature
- No tenderness
- No redness
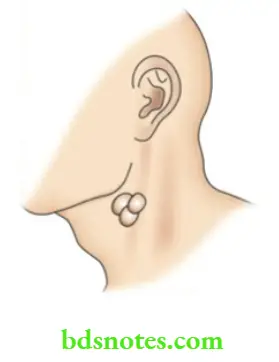

- Soft, cystic and fluctuant swelling
- Transillumination is negative
- On the Sternocleidomastoid contraction test, it becomes less prominent indicating that it is deep to deep fascia.
Differential Diagnosis
Branchial cysts can be confused for cold abscesses in the anterior triangle. Branchial cyst is of longer duration and patients with cold abscess may have other lymph nodes in the neck.
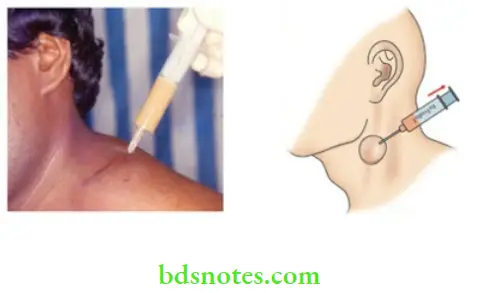
Treatment Of Cold Abscess
- Non-dependent aspiration avoids the formation of sinuses.
- A wide bore needle is preferred because the caseous material is thick.
- Incision and drainage should not be done as they cause persistent tuberculous sinus.
- Antituberculous treatment is given.
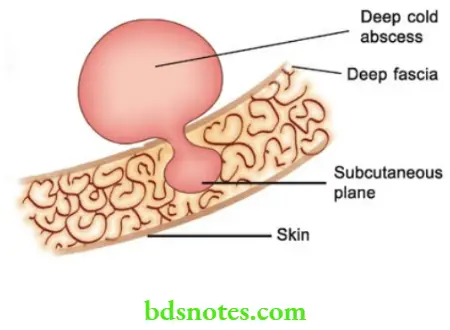
Stage Of Collar Stud Abscess
It results when a cold abscess which is deep to deep fascia ruptures through the deep fascia and forms another swelling in the subcutaneous plane which is fluctuant. Cross fluctuation test may be positive. It is treated like a cold abscess.
Stage of Sinus
- The sinus is a blind tract leading from the surface down into the tissues.
- It occurs when a collar stud abscess ruptures through the skin
- The tubercular sinus is the most common sinus in the neck in India.
- Common in young females
- It can be multiple
- The tubercular sinus will have a wide opening
- Resembles an ulcer with an undermined edge

- No induration
- The skin surrounding the sinus shows pigmentation and sometimes it is bluish in colour.
- A group of lymph nodes is usually palpable underneath the sinus.
Investigations In Tubercular Lymphadenitis
- A complete blood picture may reveal low Hb.
- ESR is elevated in the majority of cases.
- Chest X-ray is usually negative, so also sputum for AFB (Acid-fast bacilli).
- FNAC (Fine needle aspiration cytology) can give a diagnosis in about 75% of cases.
- Lymph node biopsy reveals central caseation surrounded by epitheloid cells with Langhans type of giant cells. Langhan’s type of giant cell usually has more than 20 nuclei.
- If it is a cold abscess, aspiration will reveal cheesy material.
- Edge biopsy from the sinus
Tubercular Lymphadenitis Treatment
After confirming the diagnosis anti-tuberculous treatment is given.
Antituberculous Treatment (ATT) For Lymphatic Tuberculosis
The World Health Organisation’s recommendation for extra-pulmonary tuberculosis is as follows:
- The three-drug regime—INH, rifampicin, pyrazinamide (H.R.Z.)—for two months followed by INH and Rifampicin for another four months.
- The dosage is as given below:
INH: 6 mg/kg body weight—the usual adult dose is 300 mg/day.
Rifampicin: 10 mg/kg body weight—usual adult dose is 4500600 mg/day.
Pyrazinamide: 30 mg/kg body weight— usual adult dose is 1,500 mg/day.
- Detailed dosages of ATT and side effects of these drugs are discussed in medicine textbooks.
Role of surgery in tuberculous lymphadenitis
- Biopsy—Lymph node biopsy, wedge biopsy from the edge of the sinus.
- Aspiration—Non-dependent aspiration of cold abscess.
- Excision of the lymph nodes if they persist in spite of antituberculous treatment.
- Excision of sinus wall along with the tract.
Other special types of pyogenic infections
Boil
- This is also called furuncle. It is a hair follicle infection caused by Staphylococcus aureus or a secondary infection of a sebaceous cyst. Diabetic patients are more vulnerable to boiling.
- It starts with painful indurated swelling with surrounding oedema. After about 1–2 days, softening occurs in the centre and a pustule develops which bursts spontaneously discharging pus. Necrosis of subcutaneous tissues produces a greenish slough. The skin overlying the boil also undergoes necrosis. Hence, a boil is included under acute infective gangrene.
Boil Precipitating Factors
- Scratching
- Diabetes
- Poor immunity
Boil Common Locations
- Face and back of the neck
- Axilla
- Gluteal region
Facts About A Boil
- Dangerous boil: On the skin of the face
- Most painful boil: External auditory
- Boll likes: Oil skin
- Blind boil or dull boll: Subsides without suppuration
- Furuncle of the external auditory meatus is a very painful condition because of the rich nerve supply of the skin. Pain is also due to dense adherence of skin to the perichondrium (there is no subcutaneous tissue).
Treatment of Boil
Incision and drainage with excision of the slough. Antibiotic cloxacillin is given. Diabetes, if present, is treated.
Complications of Boil
- Necrosis of the skin
- Pyaemic abscess and septicaemia
- Cavernous sinus thrombosis due to boiling on the face or stye on the eyelid.
Carbuncle
This is an infective gangrene of the subcutaneous tissue caused by Staphylococcus aureus. It commonly occurs in diabetic patients. With poor immunity, radiotherapy patients can also develop carbuncle.
Staphylococcal Infections Of Surgical Importance
- Boil
- Carbuncle
- Breast abscess
- Parotitis
- Osteomyelitis
Sites: The Nape of the neck is the commonest site followed by the back and shoulder region. The skin of these sites is coarse and has poor vascularity
Carbuncle Pathology
- The initial lesion is similar to a boil in the form of hair follicle infection with perifolliculitis. Since the majority of patients are diabetics, infection takes a virulent course and results in necrosis of subcutaneous fat which gives rise to multiple abscesses.
- These abscesses are intercommunicating and they open to the exterior by multiple openings which are called sievelike openings. This appearance is described as cribriform appearance which is pathognomonic of carbuncle.

Carbuncle Clinical features
- Typically, the patient is a diabetic.
- Severe pain and swelling in the nape of the neck
- Constitutional symptoms like fever with chills and rigours are severe.
- The surface is red, angry looking like a red hot coal.
- The surrounding area is indurated.
- Later, skin on the centre of the carbuncle softens and peripheral satellite vesicles appear, which rupture discharging pus and giving rise to a cribriform appearance.
- The end result is the development of a large crateriform ulcer with a central slough.
Carbuncle Complications
- Worsening of the diabetic status results in diabetic ketoacidosis.
- Extensive necrosis of skin overlying carbuncle. Hence, it is included under acute infective gangrene.
- Septicaemia, toxaemia.
Carbuncle Treatment
- Diabetes control preferably with injectable insulin
- Appropriate parenteral antibiotics are given till complete resolution occurs. Most strains of staphylococcal aureus are sensitive to cloxacillin, flucloxacillin, erythromycin and some of the cephalosporins. However, Methicillin Resistant Staphylococcal Aureus (MRSA) infections are resistant to the drugs mentioned above. They are sensitive only to expensive drugs such as Vancomycin which has to be given intravenously.
- Improve the general health of the patient
- If the carbuncle does not show any softening or if it shows evidence of healing, it is not incised. It can be left open to the exterior or saline dressings are applied to reduce oedema. Complete resolution may take place within 10–15 days.
- Surgery is required when there is pus. The cruciate incision is preferred because of multiple abscesses and extensive subcutaneous necrosis.
- Edges of the skin flap are excised, pus is drained, loculi are broken down, the slough is excised, and a cavity is treated with antiseptic agents. Like a pyogenic abscess, a wound heals with granulation tissue from the depth. Practically it amounts to the excision of a carbuncle.


Summary Of Carbuncle
- Caused by Cocci
- Abscesses Communicating
- Red hot like Coal
- Appearance Cribriform, Crateriform ulcer
- Gangrene Cutaneous and (subcutaneous)
- Drug of choice Cloxacillin
- Diabetes Control
- Incision Cruciate
Erysipelas
- It is an acute inflammation of the skin and subcutaneous tissues associated with severe lymphangitis. The causative organism is Streptococcus pyogenes. Precipitating factors are malnourishment, chronic diseases, etc. Thus, children and old people are commonly affected.
- Infection sets in after a small scratch or abrasion and spreads very rapidly resulting in toxaemia. Sites: Face, eyelids, scrotum and in infants, the umbilicus.
Erysipelas Clinical features
- Rose-pink rash with raised edge appreciated on palpation and has a consistency of buttonhole.
- Vesicles appear later and rarely become pustular.
- Oedema of eyelids or scrotum depending upon the site.
- Features of toxaemia
- When it occurs in the face, it involves the pinna because the erysipelas is basically a cuticular lymphangitis. This is described as Milian’s ear sign positive.
- This sign is used to differentiate cellulitis of the face from facial erysipelas. In cellulitis of the face, the pinna does not get involved because of the close adherence of skin to the cartilage.
Erysipelas Complications
- Toxaemia and septicaemia
- Gangrene of skin and subcutaneous tissue
- Lymphoedema of the face and eyelids due to lymphatic obstruction causing fibrosis of lymphatics.
Erysipelas Treatment
Injection crystalline penicillin 10 lakh units 6th hourly IM/IV for 5–10 days.
Gonorrhoea
This is a sexually transmitted disease caused by Neisseria gonorrhoeae (gonococcus). It is a Gram-negative intracellular diplococcus which affects mainly the epithelium of the urogenital tract, rectum, pharynx, and conjunctivae. In males, the anterior urethra is involved.
Gonorrhoea Clinical features
- In men: Dysuria and urethral discharge are the most common symptoms.
- In women: Vaginal discharge and dysuria are common symptoms. Bilateral salpingitis may lead to infertility.
Gonorrhoea Diagnosis
- Gram stain and culture on special media
- Two glass tests: The patient is asked to urinate. The haziness in the first glass indicates pus and in the next stream, urine is clear.
Gonorrhoea Treatment
Penicillin is the treatment of choice.
- Incubation period 2–14 days
- Early morning hazy urine
Gonorrhoea Complications
- Urethral structure
- Epididymoorchitis
- Prostatitis
- Proctitis
- Salpingitis
Anthrax
This disease is caused by Bacillus Anthracis which is a Gram-positive, spore-forming aerobic rod. The organism is capable of toxin production. As the disease is found in cattle, it is likely that it affects people who handle carcasses, wool, hides, etc., e.g. farmers, butchers and dealers in wool and animal hide.
Types of Clinical Features
Cutaneous type: After 3–4 days of the incubation period, an itching erythematous papule develops on the exposed portion of the body such as the hand, forearms, face, etc. The papules suppurate and form black slough. This type of lesion, surrounded by vesicles is called a malignant pustule. It is self-limiting in the majority of cases.
Induration of the surrounding tissue and toxaemia are the other features.
Alimentary type: Occurs following ingestion of spores. Gastroenteritis like picture such as vomiting, abdominal pain, diarrhoea and even haematemesis can occur.
Anthrax Pulmonary: It is also called Woolsorter’s disease. This results due to the inhalation of spores. Clinically, it manifests as a non-productive cough, fever and retrosternal discomfort.
Anthrax Treatment
Penicillin given orally or injectable for a period of 2 weeks is the treatment
Chronic Abscess
It results when the initial infective process or the cause is not fully identified and treated.
Chronic Abscess Sites
Foot, hand, etc.
Chronic Abscess Causes
- Foreign bodies: These are the most common causes of chronic abscess. A typical history of recurrent swelling discharging pus is present. Wooden pieces lodged in the thigh or in the foot are common. Synthetic mesh used in the repair of hernias getting infected is another example.
- Dead tissue: As it occurs in diabetes patients.
- Pilonidal sinus: This condition gives rise to recurrent abscesses. Typical history of pain and swelling which ruptures followed by spontaneous recovery is present. However, the sinus persists.
- Chronic disease: All features of a cold abscess are present but in an unusual situation (not a cold abscess arising from the lymph nodes).
Necrotising Fascitis
It is a spreading destructive invasive infection of the skin and soft tissues including deep fascia with relative sparing of muscle.
Common sites
Genitalia, groin, lower abdomen. In these places, it is comparable or similar to and called Meleney’s gangrene. Other sites are limbs.
Causative organism
Two types have been identified:
- Monomicrobial: It is due to Group A beta-haemolytic streptococci. It is also called Type 2 necrotising fasciitis.
- Polymicrobial: It is due to the synergistic combination of anaerobes and coliforms or nongroup A streptococci Type 1 Necrotising fascitis.
Specific Features Of Type 2 Necrotising Fascitis
- Caused by Streptococcus pyogenes
- Occur in young healthy people
- Minor abrasions and lacerations may be a precipitating factor
- Severe systemic illness with multiorgan failure—Streptococcal toxic shock syndrome
- Very often there is no history of injury when it occurs in the lower limbs.
Risk factors For Type I Necrotising Fascitis
Type I Necrotising Fascitis Clinical Features
- Sudden pain in the affected area with gross swelling of the part
- The part is swollen, red erythematous, and oedematous with skip lesions of skin necrosis and ulceration.
- High-degree fever, jaundice, and renal failure can occur soon in untreated cases. Often crepitus is palpable.
Type I Necrotising Fascitis Diagnosis
Full thickness biopsy taken at the bedside can give the full diagnosis. Watery pus (dishwater liquid) is also characteristic.
Type I Necrotising Fascitis Treatment
Early, aggressive treatment includes supportive and surgical treatment.
Type I Necrotising Fascitis Supportive treatment
- This includes hospitalisation, adequate hydration, and broad-spectrum antibiotics.
- Surgery involves wide excision, generous debridement followed a few days or weeks later by skin grafting
- In Type 2 Cases (Streptococcal): High-dose penicillins along with clindamycin is the treatment of choice. Clindamycin has a special effect as it is a potent suppressor of bacterial toxin synthesis.


Necrotising Fascitis—Risk Factors
- Diabetes mellitus, malnutrition
- Obesity, corticosteroids
- Immune deficiency

Leave a Reply