Diseases of Tongue: Questions and Answers
Question 1. Write a short note on glossodynia.
Answer. Glossodynia is defined as the painful tongue.
Glossodynia Etiology
Glossodynia Local Factors
- Habits: Excessive use of tobacco, excessive drinking, bruxism.
- Dental causes: Various local causes such as dentures, irritating clasp or recently fixed bridges.
- Referred pain: It is from the infected teeth or tonsils.
- Sensitizers: Various sensitizers, such as peppermint oil and primary and secondary sensitizers
- Tongue disorders: Such as plicated tongue, lichen planus, geographic tongue etc.
- Electrogalvanic current: It is produced when two dissimilar metals come in contact
- Atherosclerotic changes: These changes occur in the lingual arteries.
- Allergy: Allergy to various dental materials, metallic restoration, food, medication, dentifrices etc.
“Understanding diseases of the tongue through FAQs: Q&A explained”
Glossodynia Systemic Factors
- Various systemic diseases lead to glossodynia such as multiple myeloma, amyloidosis muscular tension, hypoestrogenism, pernicious anemia, pellagra etc.
- Gastric disturbances such as hyperacidity or hypoacidity, angioneurotic edema
- Xerostomia, prolong antibiotic activity and hypothyroidism.
Read And Learn More: Oral Medicine Question And Answers
Glossodynia Neurological Factors
- Trigeminal neuralgia, damage of lingual nerve after surgery, glossopharyngeal neuralgia.
- Cerebral sclerosis and subclinical cerebrovascular accidents.
Glossodynia Idiopathic
When no local systemic or neurological cause are detected in these circumstances, depressions, cancerophobia and neurosis are possible cause.
“Importance of studying tongue diseases for better diagnostic outcomes: Questions explained”
Glossodynia Clinical Features
- Presence of burning, tingling or numbness of tongue.
- It may occur as isolated features or it may be one form group of oral symptoms.
- It may occur with clinically, absorbable changes in tongue or without observable changes.
Tongue Diseases: Key Questions and Answers
Glossodynia Management
- Removal of local cause, construction of plastic retainers.
- Treatment of muscular problems by correction of malocclusion or by giving muscle relaxant such as diazepam.
- Treatment of systemic cause should be carried out.
- Surgical exploration of glossodynia with neuropathy.
- Use of topical analgesic 0.5% aqueous diphenhydramine alone or mixture with 0.5% of lidocaine.
“Common challenges in diagnosing tongue diseases effectively: FAQs provided”
Question 2. Write short note on black hairy tongue.
Answer. It is also called as lingua valiosa, lingua nigra.
- It designates an overgrowth of filiform papilla on dorsum of tongue, giving tongue a superficial resemblance as that of hairiness.
- This condition is commonly referred to as black hairy tongue, but hairy tongue may also appear as brown, white, green, pink or variety of hues depending on specific etiology and the secondary factors.

“Why is early detection critical for managing tongue diseases? Answered”
Black Hairy Tongue Etiology
- Fungal organisms such as Candida albicans and systemic disturbances.
- Use of certain drugs such as sodium perborate and penicillin.
- Extensive X-ray radiation around head and neck for treatment of tumors.
- Occur in patient with intermaxillary fixation and with disturbed orophysiology.
- Lowered pH of oral secretion, which blocks normal desquamation of epithilial cells covering filiform papillae.
- Debilitating diseases. Tongue movements restricted due to illness.
- Various foods such as coffee and tea.
Black Hairy Tongue Clinical Features
- It is commonly seen in persons having HIV.
- Lesion involves dorsum of tongue, particularly middle and posterior 1/3rd of tongue.
- Papilla, which is of considerable length, will brush the palate and produce gagging.
- Hypertrophy of filiform papillae is seen. Papillae may reach to size of 2 cm.
- In appearance, papillae are elongated and have appearance of hair.
- The color varies from yellowish white to brown or black depending on extrinsic factors such as tobacco, certain foods, medicines or chromogenic organisms of oral cavity.
Black Hairy Tongue Management
- Brushing of tongue twice daily for 2 minutes, making gentle movements over involved area towards tip of tongue.
- Topical application of keratolytic agent such as podophyllum in acetone and alcohol suspension seems to be quite affective.
- Oral antibiotics can also be given for 10 to 14 days. Antibiotic of choice is phenoxymethyl penicillin 500 mg four times a day. Patient who is allergic to penicillin can take erythromycin ethyl succinate 400 mg three times a day.
- Surgical removal of papillae by electrodessication, carbon dioxide laser or even the scissor.
“Factors influencing success with tongue disease treatment: Q&A”
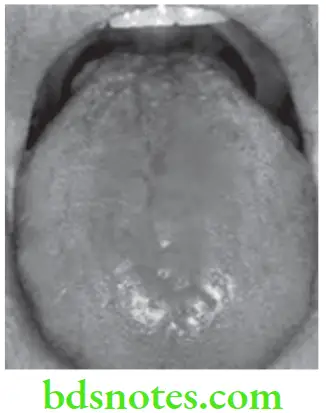
Question 3. Write short note on geographic tongue.
Or
Write short note on benign migratory glossitis.
Answer. It is also called as benign migratory glossitis or wondering rash or glossitis areata exfoliativa and erythema migrans.
It is defined as irregularly-shaped reddish area of depapillation and thinning of dorsal tongue epithelium which is surrounded by narrow zone of regenerating papillae which are whiter than surrounding tongue surface.
Geographic Tongue Etiology
- Immunological reaction, allergic, emotional factors and hereditary factors
- Infections and nutritional deficiencies due to history of asthma, eczema and hay fever.
Geographic Tongue Classification
Geographic Tongue Type 1: Lesion confined to tongue, with both active and remission phases.
Geographic Tongue Type 2: As type-I with similar lesions elsewhere in mouth.
Geographic Tongue Type-3: Lesions on the tongue that are not typical and that may be accompanied by lesions elsewhere in mouth. It consists of two forms:
- Fixed form: Few areas of tongue are affected, but no movement is seen.
- Abortive form: It starts as yellow white patch but disappear before acquiring appearance of geographic tongue.
Geographic Tongue Type 4: No tongue lesions are present but geographic areas are present in mouth.
“Steps to explain causes of tongue diseases: Infections vs nutritional deficiencies: Q&A guide”
Geographic Tongue Clinical Features
- It is common in young and middle-aged persons with age ranging from 5 to 84 years with predilection for females.
- Lesion is confined to the dorsal surface and lateral border of tongue, but may occur in ventral surface. It is variable in size and diameter and may be single or multiple.
- It is asymptomatic, but patient may complain of burning sensation which is made worse by spicy or citrus fruits.
- It appears as erythematous, non-indurated, atrophic lesion, bordered by slightly elevated distinct rim that varies from grey to white to light yellow.
- Multiple areas of desquamation of filiform papilla in irregular circinate fashion.
- Central portion of lesion, sometimes appears inflammed, while border is outlined by thin yellow white line or band.
- Fungiform papilla persists in desquamated areas as small elevated red dots.
- Areas of desquamation remain for short time in one location then heal and appear in other location thus giving rise to term migration.
Geographic Tongue Differential Diagnosis
- Psoriasis: Psoriasis shows cutaneous lesions while geographic tongue does not.
- Lichen planus: Shows Wickham’s striae while geographic tongue does not.
- Pityriasis rosea: Shows cutaneous lesions while geographic tongue does not.
- Reiter’s syndrome: It shows combination of cutaneous, ophthalmic and urethral lesions along with arthritis while geographic tongue does not.
Geographic Tongue Management
- For control of burning topical local anesthetic agents such as lidocaine, diphenhydramine.
- Balanced diet, elimination of irritants and psychological reassurance.
- Topical corticosteroids and topical application of salicylic acid and tretinoin for external use.
- According to recent researches zinc supplement is effective in symptomatic geographic tongue.

“Role of bacteria and fungi in causing tongue diseases: Questions answered”
Question 4. Write note on bald (smooth) tongue.
Answer. By bald tongue, we mean the depapillation of the tongue.
Mainly two things are responsible for the smooth tongue, i.e.
- Local disease.
- Systemic disease.
Bald (smooth) Tongue Local Disease
- Eosinophilic granuloma: It is characterized by a well demarcated proliferative ulceration covered by thick masses of fibrin. It is located on dorsum, margin or inferior surface of the tongue. Putrid odor is present.
- Traumatic injuries: The tongue may be repeatedly traumatized, either mechanically or chemically. Trauma is mainly due to the jagged teeth, rough margin of restoration and long term contact of tongue with the dental medications. Localized area of depapillation are often noted with papillary regeneration around such areas.
- Lesion due to automutilation: Self-inflicted bite can produce injury to tongue. This occurs in mentally handicapped patients.
- Allergic stomatitis: It refers to edematous changes in part or all of the oral and lingual mucosa, due to hypersensitivity reaction. There is edematous swelling of the tongue.
- Facial hemiatrophy: There is presence of unilateral atrophy of tongue, subcutaneous tissue and muscle of face. Atrophy of half of tongue is present due to which there is presence of depapillation of tongue.
- Chronic candidiasis: It is present on the dorsum of the tongue. It is difficult to distinguish from median rhomboid glossitis.
Bald (smooth) Tongue Systemic Disease
- Iron deficiency anemia: There is presence of atrophic changes on the dorsum of the tongue. The changes firstly occur over the tip and lateral borders of tongue along with the loss of filiform papillae. In extreme cases, complete dorsum becomes smooth and glazed. Tongue is painful and can be fiery red.

“How does vitamin B12 deficiency lead to glossitis? FAQ explained”
- Pernicious anemia: Here the patient has burning and itching sensation in oral mucous membrane with disturbance of taste and occasional xerostmia. Atrophy of fungiform and filiform papillae is seen. In advanced cases, entire dorsum gets atrophic, smooth and have fiery red surface. Tongue appears to be flabby.
- Niacin deficiency: Pellagra is the condition occurs due to deficiency of niacin. In patients with niacin deficiency tongue becomes fiery red and devoid of papilla. Here, filiform papilla disappear first and fungiform papilla become enlarged. In advanced cases all papillae become lost and reddening of tongue increases.
- Folic acid deficiency: The tongue is fiery red and there is atrophy of filiform and fungiform papillae. The tongue is swollen and small cracks appear on the dorsum of the tongue.
- Syphilis: Depapillation of tongue occur in the secondary and tertiary syphilis. Atrophy of fungiform and filiform papillae is present.
- Zoster infection: Numerous vesicles appear on the ventral surface of the tongue, hence the tongue appears smooth.
- Tuberculosis: In cases with tuberculosis most commonly the involved area is dorsum of tongue. Ulcer is present with irregular outline and the undermined borders which are covered by yellowish grey fibrinous layer.
- Diabetes: It leads to atrophic glossitis. There is presence of central papillary atrophy of dorsum of tongue in which low flat papillae are noticed just anterior to the row of circumvallate papillae.
- Lupus erythematosus: There is presence of isolated irregular areas of lingual mucosa with atrophy and ulceration.
Bald (smooth) Tongue Differential Diagnosis
- If tongue is completely bald, xerostomia is the technique which is to be considered. Recognition of xerostomia is done by seeing the absence of salivary pool in floor of mouth or by sticking tongue blade on oral mucosa at the time of oral examination.
- If there is presence of partial baldness conditions such as benign migratory glossitis, lichen planus, median rhomboid glossitis etc should be considered.
Question 5. Classify disorders of tongue and enumerate causes of papillary atrophy of tongue.
Answer.
Disorders of Tongue
- Developmental
- Aglossia or hypoglossia
- Ankyloglossia
- Bifid tongue
- Lingual polyp
- Macroglossia
- Median rhomboid glossitis
- Infectious
- Bacterial
- Fungal and saprophytic
- Parasitic
- Viral
- Cystic
- Epidermoid
- Dermoid
- Lymphoepithelial
- Mucus
- Anterior median lingual cyst
- Gastric mucosal cyst
- Parasitic cyst
- Bronchogenic cyst
“Early warning signs of issues addressed by understanding tongue disease pathogenesis: Common questions”
- Neoplastic
- Benign
- Fibroma
- Granular cell myoblastoma
- Leiomyoma
- Rhabdomyoma
- Neurofibroma
- Keratoacanthoma
- Traumatic neuroma
- Papilloma
- Pyogenic granuloma
- Adenoma
- Hemangioma
- Lymphangioma
- Malignant
- Squamous cell carcinoma
- Transitional cell carcinoma
- Verrucous carcinoma
- Mucoepidermoid carcinoma
- Reticular cell carcinoma
- Lymphosarcoma
- Angiosarcoma
- Kaposi’s sarcoma
- Melanoma
- Rhabdomyosarcoma
- Metastatic lesions from
- Kidney
- Liver
- Stomach
- Lung
- Benign
- Red and White Lesions
- Leukoplakia
- Erythroplakia
- Lichen planus
- Oral submucous fibrosis
- Candidiasis
- Psoriasis
- Focal epithelial hyperplasia
- White sponge nevus
- Pemphigus
- Syphilitic mucus patches
- Verruca vulgaris
“Asymptomatic vs symptomatic effects of ignoring tongue disease triggers: Q&A”
- Neurological
- Dyskinesia-involuntary movements
- Glossodynia
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Polyneuritis
- Neurofibromatosis
- Tongue thrusting
- Dysgeusia
- Papillary Changes in Tongue
- Atrophic
- Median rhomboid glossitis
- Geographic tongue
- Pernicious anemia
- Protein deficiency
- Lichen planus
- Oral submucous fibrosis
- Scleroderma
- Hypertrophic
- White and black hairy tongue
- After antibiotic therapy
- After steroid therapy
- Hydrogen peroxide mouthwash
- Immunosuppressive drugs
- Smoking
- High fever
- Constipation
- Hyperacidity.
- Atrophic
- Fissured Tongue
- Congenital
- Syphilis
- Amyloidosis
- Melkersson-Rosenthal syndrome
- Papillon-Lefèvre syndrome
- Traumatic bite.
“Can targeted interventions improve outcomes using knowledge of etiology? Answer provided”
- Systemic Diseases Manifested in Tongue
- Infection—bacterial, viral and fungal
- Blood disorders
- Metabolic disorders
- Dermatological disorders
- Collagen and autoimmune disorders.
Causes of Papillary Atrophy of Tongue.
- Local Disease
- Eosinophilic granuloma.
- Traumatic injuries.
- Lesions due to auto-mutilation.
- Allergic stomatitis.
- Facial hemiatrophy.
- Cranial arthritis.
- Chronic candidiasis.
- Systemic Diseases
- Iron deficiency anemia.
- Plummer-Vinson syndrome.
- Pernicious anemia.
- Niacin deficiency.
- Folic acid deficiency.
- Peripheral vascular disease.
- Dermatomyositis.
- Diabetes.
- Syphilis.
- Zoster infection.
- Tuberculosis.
“Steps to educate patients about tongue diseases and their importance: Q&A format”
Question 6. Write short note on median rhomboid glossitis.
Answer. It is also called as central papillary atrophy of tongue.
It is a developmental defect resulting from incom-plete descent of tuberculum impar and entrapment of portion between fusing lateral halves of tongue.
“Role of counseling in clarifying goals for managing tongue diseases: Questions answered”
Median Rhomboid Glossitis Etiology
- Developmental: Persistent tuberculum impar suggest its developmental origin.
- Fungal infection with Candida albicans.
- Metabolic: It is more commonly seen in diabetics.
Median Rhomboid Glossitis Clinical Features
- It occurs in 15 to 84 years and is predominant in males.
- It is located just anterior to foramen cecum or dorsal surface of tongue, in midline and anterior to circumvallate papilla.
- It appears as ovoid, diamond or rhomboidal shape reddish patch or plaque on dorsal surface of tongue immediately anterior to circumvallate papilla.
- Surface is dusky red and completely devoid of filiform papilla and is usually smooth.
- It is asymptomatic, but pain and ulceration are reported.
- Rest of the tongue is coated or matted.
Median Rhomboid Glossitis Diagnosis
- Clinical diagnosis: Rhomboidal shaped lesion present on posterior part of tongue.
- Laboratory diagnosis: Biopsy shows loss of papillae having varying degree of hyperparakeratosis. Proliferation of spinous cell layer is present along with enlarged rete pigs which can branch and anastomose.
Median Rhomboid Glossitis Management
- Anti-fungal agent, i.e. nystatin is to be given.
- In long-standing cases, cryosurgery or excisional biopsy is to be done.
“How do educational materials explain complex tongue disease concepts? FAQ explained”
Question 7. Write short note on local causes of depapillation of tongue.
Answer. Following are the local causes of depapillation of tongue:
- Eosinophilic granuloma.
- Traumatic injuries.
- Lesions by automutilation.
- Allergic stomatitis.
- Facial hemiatrophy.
- Cranial arthritis.
- Chronic candidiasis.
Question 8. Write short note on allergic stomatitis.
Answer. Allergic stomatitis is one of the local causes of depapillation of tongue.
- In allergic stomatitis, edematous changes occur in part or all of oral and lingual mucosa because of hypersensitivity reaction.
- Allergic stomatitis occurs due to certain drugs such as antibiotics, cancer drugs and anti-cholinergic agents.
- Allergic stomatitis also occurs due to various allergic agents such as denture material, mouthwash, chewing gum, etc.
- Edematous swelling is present over the tongue.
- Depapillation of tongue is also present.
“Early warning signs of knowledge gaps in patient understanding of tongue diseases: Common questions”
Question 9. Discuss differential diagnosis of red lesions on the tongue.
Answer. Following is the differential diagnosis of red lesions on the tongue:
- Erythroplakia
- Erosive oral lichen planus
- Erythematous candidiasis
- Oral pemphigus
- Ulcerative granuloma secondary to eosinophilia
- Carcinoma of tongue
- Sarcoidosis
- Oral lesion secondary to Crohn’s disease
- Median rhomboid glossitis
- Benign migratory glossitis
- Iron deficiency anemia
- Pernicious anemia
Erythroplakia: Erythroplakia is defined as ‘‘a fiery red patch that cannot be characterized clinically or pathologically as any other definable disease”. Tobacco and alcohol are commonly considered important aetiologic factors. Shear described erythroplakia as three variants: 1) Homogeneous erythroplakia – lesion that appeared flat, velvety, with uniformly red appearance; 2) Granular erythroplakia – red lesions with granular surface; 3) Speckled erythroplakia/erythroleukoplakia – predominantly red lesion speckled with white spots. Histopathologically, it usually shows some degree of dysplasia and in some cases carcinoma in situ or invasive carcinoma.
Erosive lichen planus: Erythematous lesions surrounded by whitened striae are the conventional clinical manifestation of erosive oral lichen planus which is a chronic autoimmune disease that affects the skin, genital mucosa, the oral mucosa, scalp, and nails. Atrophic or erosive lichen planus is clinically significant because burning sensation or pain or both often are present.
Erythematous candidiasis: It is a common opportunistic oral infection. It appears bright red in color and may be asymptomatic or associated with a burning sensation and pain. A cytologic smear is useful in confirming the clinical diagnosis.
Oral pemphigus: Erosions and ulcers are the main features of oral pemphigus which initially occur as vesiculobullous lesions which rupture and ulcerate. Ulcers heal slowly, but scarring is rare. Pemphigus rarely remains localized during its clinical course. The predicament of why the disease is localized in some patients and involves multiple sites.
Ulcerative granuloma secondary to eosinophilia: It is a rare self-limited oral condition mostly occurring in the sixth and seventh decades of life that manifests as a solitary ulceration varying in size from few millimeters to several centimeters, with elevated and indurated borders and with peripheral erythema, a white or yellowish base and fibrinous membrane affecting mostly the tongue, buccal mucosa or lip. Pain may hinder food intake. It may regress spontaneously in less than a month with or without recurrence and may sometimes be associated with enlarged regional lymph nodes.
“Can interactive tools improve adherence to tongue disease care protocols? FAQs provided”
Carcinoma of tongue: It may resemble a leukoplakia, a verrucous leukoplakia, an erythroleukoplakia, or an erythroplakia, and may develop into a necrotic looking ulcer with irregular, raised indurated borders, or into a broad based exophytic mass with a surface texture which may be verrucous, pebbled or smooth. When traumatized, oral squamous cell carcinoma bleeds readily and often becomes superficially secondarily infected. Pain may or may not be present unless secondarily infected. Large lesions may interfere with normal speech, mastication or swallowing.
Sarcoidosis: It involves multiple systems and most commonly affects young adults. It may be acute or insidious in onset where acute onset cases show a spontaneous resolution and progressive fibrosis may occur in cases with insidious onset. The diagnosis is confirmed by clinicoradiographic findings of hilar lymphadenopathy, pulmonary infiltration, ocular and skin lesions and histological evidence of epithelioid granulomas in more than one system.
Median rhomboid glossitis: It appears as ovoid, diamond or rhomboidal shaped red patch or plaque over the dorsum of tongue, immediately anterior to circumvallate papillae. Surface is dusky red and is completely devoid of filiform papillae.
“Asymptomatic vs symptomatic effects of poor communication about tongue diseases: Answered”
Benign migratory glossitis: It appears as small erythematous, non-indurated atrophic lesion which is bordered by slightly elevated distinct rim which vary from grey to white to light yellow. Here area of desquamation remains for small time in one location then heals and appears in another location.
Iron deficiency anemia: Here, the tongue is painful and fiery red in color. Loss of papillae is present due to which tongue become smooth and glazed. Laboratory investigation of the iron profile is diagnostic along with general signs of iron deficiency anemia.
Pernicious anemia: In advanced cases tongue becomes smooth and fiery red in appearance. There is atrophy of fungiform and filiform papillae. Laboratory investigation of the vitamin B12 deficiency test is diagnostic.
Leave a Reply