Bacteriology Streptococcus
Question 1: Classify the gram-positive cocci. Describe the morphology, and culture characteristics of Streptococcus pyogenes.
Answer:
Gram-positive cocci are:
- Staphylococcus.
- Streptococcus
- Pneumococcus
- Micrococcus
- Sarcinococcus.
Read And Learn More: Microbiology Question And Answers
Streptococcus pyogenes
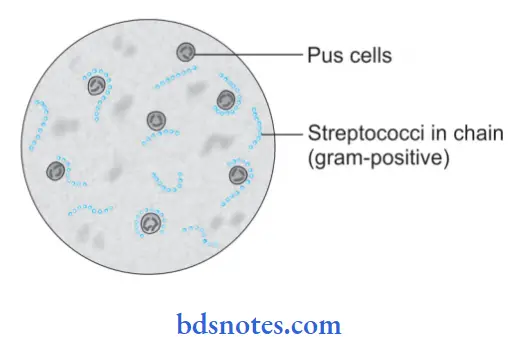
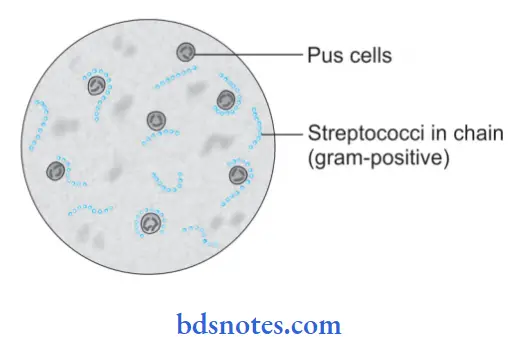
1. Morphology: It is 0.5 to 1 m in diameter and is arranged in a chain.
- Chain formation is due to colic dividing in one plane only and daughter cells fail to separate completely, best demonstrated in pus.
- It is usually encapsulated.
- Group B and D-polysaccharide capsule
- Group C-hyaluronic acid capsule
- Non-sporing and non-motile.
Culture characters: Streptococcus pyogenes is an aerobic and facultative anaerobe.
- Growth occurs in optimum temperature at 37°C at pH –7.4
- Enriched media with whole blood, serum as citric flid, or glucose favors rapid growth.
- Fluid media: Serum broth, 24 hours after culture shows granular growth with powdery deposits.
- Blood agar: After 24 hours of incubation colony is small and (pinpoint colony) circular, transparent low area of hemolysis.
- Strain with capsules produces mucoid colonies.
- Virulent strains produce mature colonies.
Question 2. Describe diagramof streptococci.
Answer:
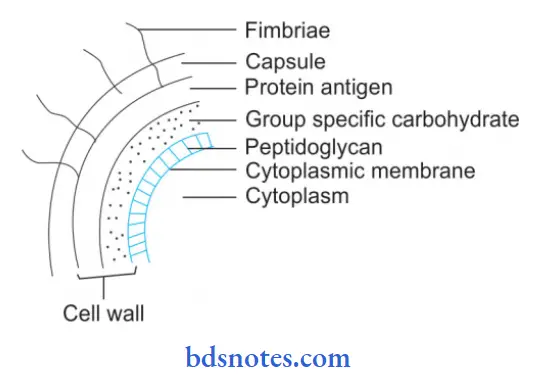
Structure of Streptococci
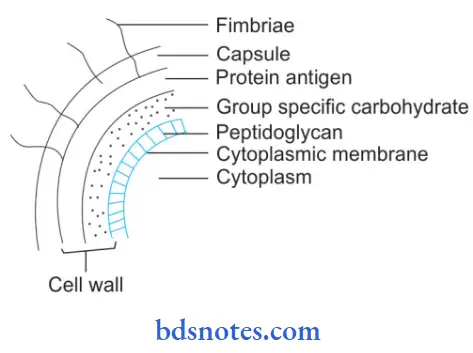
- Capsular hyaluronic acid: This capsule inhibits phagocytosis
- Protein antigen: It inhibits phagocytosis and forms fimbriae, which are covered in lipopolysaccharide and help the organism to attach to the cell
- Group-specific polysaccharide antigen: The cell wall is composed of an outer layer of protein (Fimbria containing protein) and lipoteichoic acid.
- The middle layer is of group-specific carbohydrates and an inner layer of peptidoglycans.
- The peptidoglycan is responsible for wall rigidity.
- Type-specific antigen: The outer part of the cell wall contains protein antigens M, T, and R.
- Toxins and enzymes: Streptococcus pyogenes produces several exotoxins and enzymes which contribute to its virulence.
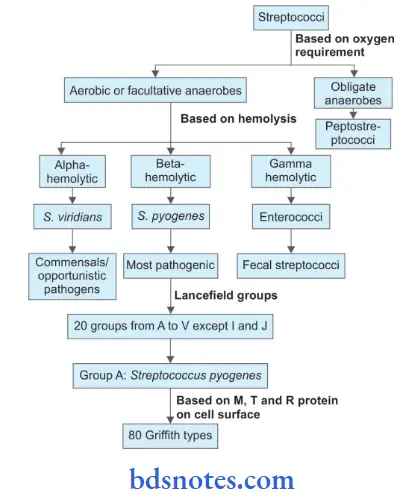
Question 3. Givetheclassifiationofstreptococcianddistinguishing features of each type.
Answer:
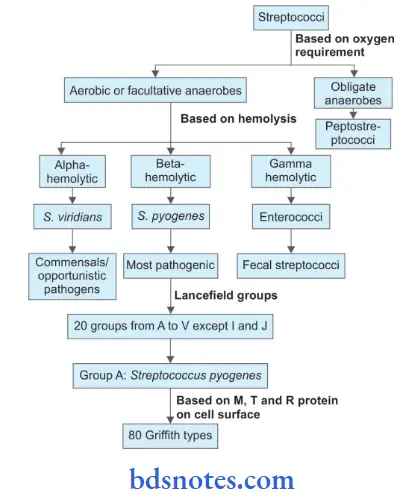
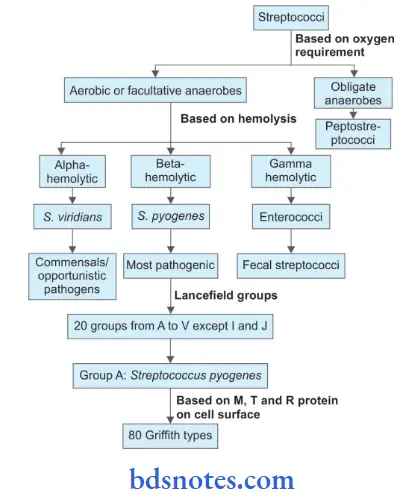
Streptococci are gram-positive cocci that are arranged in chains (see flowchart).
Distinguishing Features of Streptococci:
- Group A: Streptococcus pyogenes:
- It is arranged in a chain. It is usually encapsulated, non sporing and non-motile.
- S. pyogenes is an aerobic and facultative anaerobe.
- It ferments lactose, glucose, etc.
- It produces acid but no gas.
- It is easily destroyed by heat.
- It produces septicemia, there is a tendency to spread locally along lymphatics and through the bloodstream.
- It produces respiratory infection, skin infection, genital tract infection, acute rheumatic fever and acute glomerulonephritis.
- Group B: Streptococcus agalactiae:
- It is responsible for mastitis in cows.
- It may be present in the human throat and vagina as commensal.
- It is rarely pathogenic in man. Sometimes they may cause pupiral infection, septicemia, meningitis, and ulcerative endocarditis.
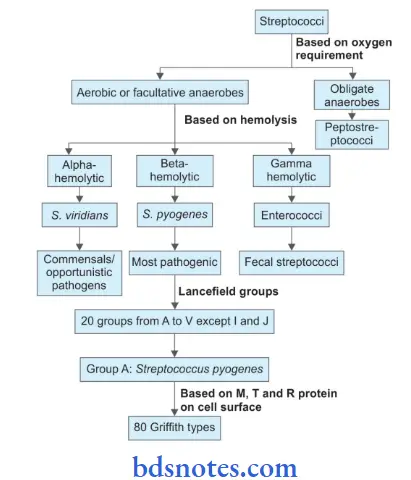
- Group C: Streptococcus equisimilis
- It may produce streptolysin O and firinolysin.
- The organism has been isolated from pupiral infection, cellulitis, wound, and scarlet fever.
- Group D:
- Group D streptococci can be divided into enterococci.
- Enterococci may cause urinary tract infection, wound infection, infective endocarditis, biliary tract infection, peritonitis, suppurative abdominal lesions, and septicemia.
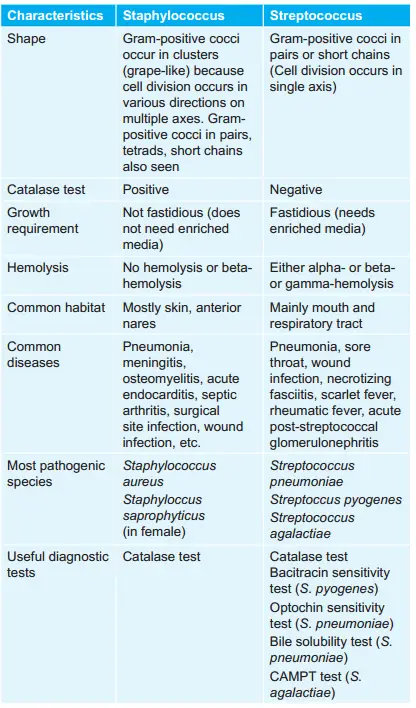
Question 4. Write a short note on the morphology of pyogenic cocci.
Answer:
The pyogenic cocci are:
- Staphylococcus aureus
- Streptococcus pyogenes.
Morphology
1. Morphology of Staphylococcus
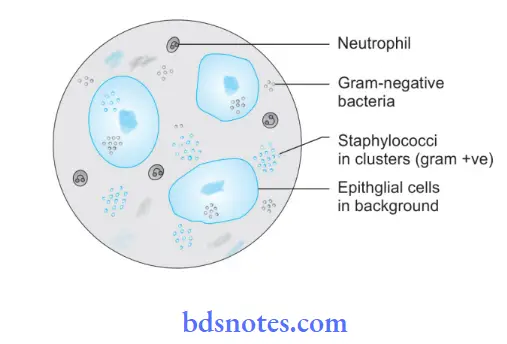
Spherical cocci are arranged characteristically in grapes-like cluster. Staphylococcus are non-motile and non-sporing. A few strains possess visible capsules, else they are noncapsulated. Stain readily with aniline dyes are uniformly gram-positive and about 1 m in diameter.
Types of Staphylococcus
Staphylococci contain multiple species but species of medical importance are as follows:
- Staphylococcus aureus: It is a pathogenic staphylococcus which leads to suppurative infections in man.
- Staphylococcus epidermidis: It leads to skin infections.
- Staphylococcus saprophyticus: It is an opportunistic pathogen.
Staphylococcus Cultural Characteristics
- Aerobes and facultative anaerobes: Optimum pH is 7.4–7.6. The optimum temperature is 37°C.
- Colony characteristics in different media are:
- Nutrient Agar: Smooth, shiny convex, opaque, golden yellow some may be white, orange, or yellow. They are large and 2 to 4 mm in diameter especially on sheep and rabbit blood agar
- Nutrient Agar Slope: Oil paint appearance.
- Blood Agar: Produces β type of hemolysis.
- Mac-Conkey medium: Small lactose-forming colonies (pink).
- Selective media: Various selective media are used for isolating S. aureus from different specimens. Selective media are:
- Salt milk agar or salt broth
- Ludlam’s medium: It has lithium chloride and tellurite
- Mannitol salt agar: Acts as both selective and indicator media. Mannitol-fermented staphylococcal colonies are surrounded by a yellow zone.
- Polymyxin agar: It is the selective media that favor the growth of coagulase-positive S. aureus.
Staphylococcus Aureus Laboratory Diagnosis
Specimen collected is pus, sputum, blood, urine, CSF, feces, and vomit.
- Microscopy: Gram-stained smears of pus or wound exudate is useful. Gram-positive cocci in the cluster are seen. On Gram staining, gram-positive cocci are arranged in grape-like clusters. Non-motile cocci in clusters are seen in hanging drop preparation.
- Culture: Specimens are inoculated on blood agar and peptone water. Specimens, where staphylococci are expected to be scanty or outnumbered by other bacteria, are inoculated in selective media such as salt agar, salt milk agar, and Robertson’s cooked meat medium. Inoculated media is incubated at 37°C for 18-24 hours. The next day culture plates are examined for the morphology of bacterial colonies. Uniform turbidity is produced on peptone water.
- Biochemical Reactions:
- Catalase test: All staphylococci are catalase positive.
- Coagulase test: Positive in S. aureus but negative in other staphylococcal species.
- Mannitol fermentation: There is the production of acid without gas.
- Gelatin liquefication is positive.
- Tellurite reduction is positive.
- Bacteriophage Typing: It is done to ascertain epidemiological purposes to trace the source of S. aureus infection. Other typing methods are antibiogram pattern, plasmid typing, ribotyping, and DNA fingerprinting.
2. Streptococcus pyogenes
Morphology: It is 0.5 to 1 m in diameter and is arranged in a chain.
- Chain formation is due to colic dividing in one plane only and daughter cells fail to separate completely, best demonstrated in pus.
- It is usually encapsulated.
- Group B and D-polysaccharide capsule
- Group C-hyaluronic acid capsule
- Non-sporing and non-motile.
Streptococcus pyogenes Culture characters: Streptococcus pyogenes is an aerobic and facultative anaerobe.
- Growth occurs in optimum temperature at 37°C at pH –7.4
- Enriched media with whole blood, serum as citric flid, or glucose favors rapid growth.
- Fluid media: Serum broth, 24 hours after culture shows granular growth with powdery deposits.
- Blood agar: After 24 hours of incubation colony is small and (pinpoint colony) circular, transparent low area of hemolysis.
- Strain with capsules produces mucoid colonies.
- Virulent strains produce mature colonies.
Question 5. Draw a labeled diagram of Streptococcus.
Answer:
Question 6. Classify Streptococcus organisms. Describemorphology, cultural features, and pathogenecity of S. pyogenes and viridians group of Streptococcus.
Answer:
Classification of Streptococcus Organisms
Morphology of S. pyogenes
- The individual cocci are spherical or oval, 0.5 to 1.0 µm in diameter, and are arranged in chains. Chain formation is there because cocci are divided in one plane and daughter cells fail to separate completely.
- Streptococci are gram-positive, non-motile, and non sporing.
- Some strains of Streptococcus pyogenes have capsules, i.e. group B, C, and D
- Groups B and D have a polysaccharide capsule
- Group C has a hyaluronic acid capsule.
Streptococcus Organisms Culture Characteristics
- They are aerobes and facultative anaerobes, growing best at a temperature of 37°C (range 22-42°C). These are most exacting in nutritive requirements, with growth occurring only in media containing blood, serum or sugars.
- On blood agar, after overnight incubation, the colonies are small (0.5-1.0 mm, pinpoint), circular, semitransparent, and low convex with a wide zone of β-hemolysis around them. Growth and hemolysis are promoted by the presence of 10% CO2 in the environment.
- Selective media containing 1:500,000 crystal violet permit the growth of streptococci but inhibit other bacteria, especially staphylococci. In liquid media, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Bacterial chains being heavier set down as deposits.
Pathogenesis
Streptococci lead to both suppurative infections and nonsuppurative complications.
1. Suppurative Infections:
- Respiratory tract infection
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occurs secondary to viral infection of the lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and heald without producing a scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated.
- Intravascular coagulation and multiple system failure—streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- The spread of infection from pharynx or tonsils causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitis.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications:
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both the heart and joints.
- It occurs in a small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross-reaction between group A streptococci and myocardium, so antibodies produced against Streptococcus, cross-react, with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross-reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen-antibody complexes and complement activation.
- It follows infection with nephritogenic strains of streptococci.
Viridans Streptococci
- Morphology: They are commensals of the mouth and upper respiratory tract. This group contains many species, for example,S. salivarius, S. mutans,
S. sanguis, and S. milleri. They are ordinarily non-pathogenic but on occasion cause disease. - Culture Characteristics: This group of streptococci produces alpha hemolysis on blood agar. They are known as viridans streptococci due to greenish discoloration on blood agar.
- Pathogenesis: Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques. These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci.
- S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Question 7. Write laboratory methods for the identification of streptococci in streptococcal infections.
Answer:
Diagnosis of acute suppurative infections is made by culture, while in non-suppurative conditions it depends on the demonstration of antibodies.
1. Acute suppurative infection
Specimens collected should be swabs, pus, blood, or CSF.
- Gram staining of smear: Gram-positive cocci in chains are indicative of streptococcal infection. Smears are of no value where streptococci are present as part of the resident flares such as in infections of the throat and genitalia.
A smear examination is important in specimens such as pus and CSF. The specimen is inoculated on a blood agar medium and incubated at 37°C for 18-24 hours. Hemolysis develops better under anaerobic conditions or in the presence of 5-10% carbon dioxide. - Colony morphology and staining: The colonies of streptococci are small 0.5-1.0 mm, circular, low convex with a zone of β-hemolysis around them. In a liquid medium, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Gram staining from colonies shows gram-positive cocci in chains. Hanging drop preparation from liquid medium shows non-motile cocci.
- Biochemical reactions: Streptococci are catalase negative which is one of the important tests to differentiate streptococci from staphylococci.
- Identification of various groups of streptococci: S. pyrogens (Group A) is more sensitive to bacitracin than other streptococci. Group B streptococci may be identified by CAMP reaction. Group ‘D’ can be isolated by performing heat resistance test.
- Antigen detection test: ELISA and agglutination tests are used to demonstrate group A streptococcal antigen from a throat swab.
2. Non-suppurative complications
- In both rheumatic fever and glomerulonephritis serological tests give retrospective evidence of streptococcal infection.
- The routine test done is antistreptolysin O titer. Titration of 200 units or more is significant for rheumatic fever.
- In glomerulonephritis, titer is low so antiDNaase B estimation is more reliable. Titre more than 300 or 350 is signifiant.
- Anti-DNAase B estimation is useful for retrospective diagnosis of streptococcal pyoderma.
- Streptozyme test is a passive slide haemagglutination test that is positive after streptococcal infections for all types of streptococci whether of throat or skin.
Question 8. Classify streptococci. Describe cultural characteristics, pathogenicity, and laboratory diagnosis of Streptococcus pyogenes.
Answer:
Classification of Streptococcus Organisms:
Morphology of S. pyogenes
- The individual cocci are spherical or oval, 0.5 to 1.0 µm in diameter, and are arranged in chains. Chain formation is there because cocci are divided in one plane and daughter cells fail to separate completely.
- Streptococci are gram-positive, non-motile, and non sporing.
- Some strains of Streptococcus pyogenes have capsules, i.e. group B, C, and D
- Groups B and D have a polysaccharide capsule
- Group C has a hyaluronic acid capsule.
Culture Characteristics
- They are aerobes and facultative anaerobes, growing best at a temperature of 37°C (range 22-42°C). These are most exacting in nutritive requirements, with growth occurring only in media containing blood, serum or sugars.
- On blood agar, after overnight incubation, the colonies are small (0.5-1.0 mm, pinpoint), circular, semitransparent, and low convex with a wide zone of β-hemolysis around them. Growth and hemolysis are promoted by the presence of 10% CO2 in the environment.
- Selective media containing 1:500,000 crystal violet permit the growth of streptococci but inhibit other bacteria, especially staphylococci. In liquid media, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Bacterial chains being heavier set down as deposits.
Pathogenesis
Streptococci lead to both suppurative infections and nonsuppurative complications.
1. Suppurative Infections:
- Respiratory tract infection
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occurs secondary to viral infection of the lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and heald without producing a scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure—streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- The spread of infection from pharynx or tonsils causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitis.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications:
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both the heart and joints.
- It occurs in a small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross-reaction between group A streptococci and myocardium, so antibodies produced against Streptococcus, cross-react, with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross-reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen-antibody complexes and complement activation.
- It follows infection with nephritogenic strains of streptococci.
Viridans Streptococci
- Morphology: They are commensals of the mouth and upper respiratory tract. This group contains many species, for example,S. salivarius, S. mutans,
S. sanguis, and S. milleri. They are ordinarily non-pathogenic but on occasion cause disease. - Culture Characteristics: This group of streptococci produces alpha hemolysis on blood agar. They are known as viridans streptococci due to greenish discoloration on blood agar.
- Pathogenesis: Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques.These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci.
- S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Laboratory Diagnosis of Streptococcus pyogenes
- Microscopic Examination:
- This is done for pus and CSF.
- CSF wet preparation shows plenty of pus cells.
- Gram-stained smear show gram-positive cocci in chain
with pus cells. - The fluorescent antibody technique is used for detecting bacteria in smear by use of fluorescent-tagged antibody.
- Culture:
- Blood agar and selective media, i.e. crystal violet blood agar and PNF media are used for specimens taken from the vagina and throat.
- The promotion of growth is by 5 to 10% carbon dioxide supplementation.
- On blood agar, typical colonies are seen with beta hemolysis. This is further processed for identification by biochemical reactions.
- Biochemical Reactions:
- S. pyogenes is both catalase-negative and bile solubility negative.
- Bacitracin Sensitivity:
- On an inoculated culture plate of streptococci, a bacitracin disc with 0.04 mg of bacitracin is placed.
- After 24 hours zone of inhibition is observed.
- S. pyogenes show a wider zone of inhibition.
- Antigen Detections:
- The Antigen of S. pyogenes is detected by ELISA and agglutination test.
- Antibody Detection:
- The routine test done is antistreptolysin O titer. Titration of 200 units or more is significant for rheumatic fever. In glomerulonephritis, titre is low so anti-DNAase B estimation is more reliable. Titer more than 300 or 350 is signifiant.
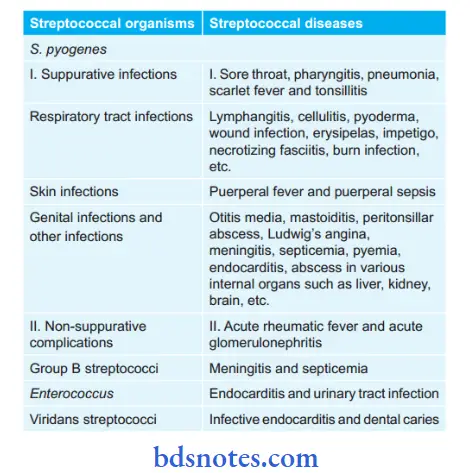
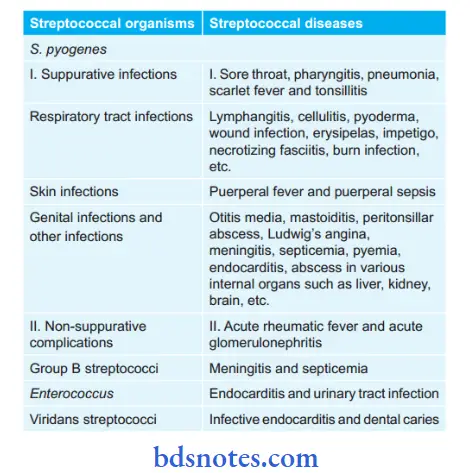
Question 9. Write a short note on Streptococcal Diseases.
Answer:
Question 10. Write a short note on Streptococcus Viridians.
Answer:
Classification of Streptococcus Organisms:
Morphology of S. pyogenes
- The individual cocci are spherical or oval, 0.5 to 1.0 µm in diameter, and are arranged in chains. Chain formation is there because cocci are divided in one plane and daughter cells fail to separate completely.
- Streptococci are gram-positive, non-motile, and non sporing.
- Some strains of Streptococcus pyogenes have capsules, i.e. group B, C, and D
- Groups B and D have a polysaccharide capsule
- Group C has a hyaluronic acid capsule.
Morphology of S. pyogenes Culture Characteristics
- They are aerobes and facultative anaerobes, growing best at a temperature of 37°C (range 22-42°C). These are most exacting in nutritive requirements, with growth occurring only in media containing blood, serum or sugars.
- On blood agar, after overnight incubation, the colonies are small (0.5-1.0 mm, pinpoint), circular, semitransparent, and low convex with a wide zone of β-hemolysis around them. Growth and hemolysis are promoted by the presence of 10% CO2 in the environment.
- Selective media containing 1:500,000 crystal violet permit the growth of streptococci but inhibit other bacteria, especially staphylococci. In liquid media, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Bacterial chains being heavier set down as deposits.
Pathogenesis
Streptococci lead to both suppurative infections and nonsuppurative complications.
1. Suppurative Infections:
- Respiratory tract infection
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occurs secondary to viral infection of the lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and heald without producing a scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure—streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- The spread of infection from pharynx or tonsils causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitis.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications:
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both the heart and joints.
- It occurs in a small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross-reaction between group A streptococci and myocardium, so antibodies produced against Streptococcus, cross-react, with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross-reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen-antibody complexes and complement activation.
- It follows infection with nephritogenic strains of streptococci.
Viridans Streptococci
- Morphology: They are commensals of the mouth and upper respiratory tract. This group contains many species, for example,S. salivarius, S. mutans, S. sanguis, and S. milleri. They are ordinarily non-pathogenic but on occasion cause disease.
- Culture Characteristics: This group of streptococci produces alpha hemolysis on blood agar. They are known as viridans streptococci due to greenish discoloration on blood agar.
- Pathogenesis: Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques. These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci.
- S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Question 11. Describe different lesions caused by Streptococcus.
Answer:
Lesions that are caused by streptococci are enumerated in
1. Suppurative Infections
- Respiratory tract infection:
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occur secondary to viral infection of lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and healed without producing scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure— streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- Spread of infection from pharynx or tonsil causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitits.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both heart and joints.
- It occurs in small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross reaction between group A streptococci and myocardium, so antibodies produced against streptococcus Group A cross-react with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen–antibody complexes and compliment activation.
- It follows infection with nephritogenic strains of streptococci.
Diseases caused by viridians streptococci:
- Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques. These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci. S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Question 12. Write a short note on Pyogenic infection.
Answer:
Pyogenic infections are caused by streptococci.
1. Suppurative Infections
- Respiratory tract infection:
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occur secondary to viral infection of lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and healed without producing scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure— streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- Spread of infection from pharynx or tonsil causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitits.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both heart and joints.
- It occurs in small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross reaction between group A streptococci and myocardium, so antibodies produced against streptococcus Group A cross-react with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen–antibody complexes and compliment activation.
- It follows infection with nephritogenic strains of streptococci.
Question 13. Discuss in short the classification of streptococcal organisms. Discuss important pathogenicity and clinical features of infection due to streptococcal pyogenes Group A and Gr D Laboratory diagnosis of streptococcal infection.
Answer:
Morphology of S. pyogenes
- The individual cocci are spherical or oval, 0.5 to 1.0 µm in diameter, and are arranged in chains. Chain formation is there because cocci are divided in one plane and daughter cells fail to separate completely.
- Streptococci are gram-positive, non-motile, and non sporing.
- Some strains of Streptococcus pyogenes have capsules, i.e. group B, C, and D
- Groups B and D have a polysaccharide capsule
- Group C has a hyaluronic acid capsule.
Culture Characteristics
- They are aerobes and facultative anaerobes, growing best at a temperature of 37°C (range 22-42°C). These are most exacting in nutritive requirements, with growth occurring only in media containing blood, serum or sugars.
- On blood agar, after overnight incubation, the colonies are small (0.5-1.0 mm, pinpoint), circular, semitransparent, and low convex with a wide zone of β-hemolysis around them. Growth and hemolysis are promoted by the presence of 10% CO2 in the environment.
- Selective media containing 1:500,000 crystal violet permit the growth of streptococci but inhibit other bacteria, especially staphylococci. In liquid media, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Bacterial chains being heavier set down as deposits.
Pathogenesis
Streptococci lead to both suppurative infections and nonsuppurative complications.
1. Suppurative Infections
- Respiratory tract infection:
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occur secondary to viral infection of lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and healed without producing scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure— streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- Spread of infection from pharynx or tonsil causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitits.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both heart and joints.
- It occurs in small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross reaction between group A streptococci and myocardium, so antibodies produced against streptococcus Group A cross-react with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen–antibody complexes and compliment activation.
- It follows infection with nephritogenic strains of streptococci.
Viridans Streptococci
- Morphology: They are commensals of the mouth and upper respiratory tract. This group contains many species, for example,S. salivarius, S. mutans, S. sanguis, and S. milleri. They are ordinarily non-pathogenic but on occasion cause disease.
- Culture Characteristics: This group of streptococci produces alpha hemolysis on blood agar. They are known as viridans streptococci due to greenish discoloration on blood agar.
- 3. Pathogenesis: Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques. These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci.
- S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Pathogenicity and clinical features caused by Group A Streptococcus pyogenes:
1. Suppurative Infections
- Respiratory tract infection:
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occur secondary to viral infection of lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm
Pathogenecity and clinical features caused by Group D Streptococcal pyogenes:
- Streptococci belonging to group D are enterococcus and non-enterococcal.
- Enterococci lead to urinary tract infections, endocarditis, wound infection, septicemia, peritonitis, and biliary tract infection.
- Non-enterococci lead to endocarditis and genitourinary infections.
- Enterococci are present in the intestine genital tract and saliva.
- E. faecalis is the frequently isolated from the urinary tract infection and wound infections.
For laboratory diagnosis of streptococcal infection:
Diagnosis of acute suppurative infections is made by culture, while in non-suppurative conditions it depends on the demonstration of antibodies.
1. Acute suppurative infection
Specimens collected should be swabs, pus, blood, or CSF.
- Gram staining of smear: Gram-positive cocci in chains are indicative of streptococcal infection. Smears are of no value where streptococci are present as part of the resident flares such as in infections of the throat and genitalia.
A smear examination is important in specimens such as pus and CSF. The specimen is inoculated on a blood agar medium and incubated at 37°C for 18-24 hours. Hemolysis develops better under anaerobic conditions or in the presence of 5-10% carbon dioxide. - Colony morphology and staining: The colonies of streptococci are small 0.5-1.0 mm, circular, low convex with a zone of β-hemolysis around them. In a liquid medium, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Gram staining from colonies shows gram-positive cocci in chains. Hanging drop preparation from liquid medium shows non-motile cocci.
- Biochemical reactions: Streptococci are catalase negative which is one of the important tests to differentiate streptococci from staphylococci.
- Identification of various groups of streptococci: S. pyrogens (Group A) is more sensitive to bacitracin than other streptococci. Group B streptococci may be identified by CAMP reaction. Group ‘D’ can be isolated by performing heat resistance test.
- Antigen detection test: ELISA and agglutination tests are used to demonstrate group A streptococcal antigen from a throat swab.
2. Non-suppurative complications
- In both rheumatic fever and glomerulonephritis serological tests give retrospective evidence of streptococcal infection.
- The routine test done is antistreptolysin O titer. Titration of 200 units or more is significant for rheumatic fever.
- In glomerulonephritis, titer is low so antiDNaase B estimation is more reliable. Titre more than 300 or 350 is signifiant.
- Anti-DNAase B estimation is useful for retrospective diagnosis of streptococcal pyoderma.
- Streptozyme test is a passive slide haemagglutination test that is positive after streptococcal infections for all types of streptococci whether of throat or skin.
Question 14. Differentiate between Staphylococcus and Streptococcus with examples(If any)
Answer:
Question 15. Describe the various infections caused by Streptococcus pyogenes. Add a note on Streptococcus viridans in infective endocardialitis.
Answer:
Streptococcus pyogenes lead to suppurative infections and non-suppurative complications.
Morphology of S. pyogenes
- The individual cocci are spherical or oval, 0.5 to 1.0 µm in diameter, and are arranged in chains. Chain formation is there because cocci are divided in one plane and daughter cells fail to separate completely.
- Streptococci are gram-positive, non-motile, and non sporing.
- Some strains of Streptococcus pyogenes have capsules, i.e. group B, C, and D
- Groups B and D have a polysaccharide capsule
- Group C has a hyaluronic acid capsule.
Culture Characteristics
- They are aerobes and facultative anaerobes, growing best at a temperature of 37°C (range 22-42°C). These are most exacting in nutritive requirements, with growth occurring only in media containing blood, serum, or sugars.
- On blood agar, after overnight incubation, the colonies are small (0.5-1.0 mm, pinpoint), circular, semitransparent, and low convex with a wide zone of β-hemolysis around them. Growth and hemolysis are promoted by the presence of 10% CO2 in the environment.
- Selective media containing 1:500,000 crystal violet permit the growth of streptococci but inhibit other bacteria, especially staphylococci. In liquid media, such as glucose broth, growth occurs as granular turbidity with a powdery deposit. Bacterial chains being heavier set down as deposits.
Pathogenesis
Streptococci lead to both suppurative infections and nonsuppurative complications.
1. Suppurative Infections:
- Respiratory tract infection
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occurs secondary to viral infection of the lung.
- Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
- Skin and soft tissue infections:
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions are seen in adults.
- Impetigo: Skin infection in young children which is characterized by superficial skin lesion as a discrete spot of 2 to 5 cm and heald without producing a scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone.
- Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated intravascular coagulation and multiple system failure—streptococcal toxic shock syndrome.
- Genital infections: S. pyogenes lead to puerperal sepsis and fever.
- Other suppurative infections:
- The spread of infection from pharynx or tonsils causes otitis media, mastoiditis, endocarditis, peritonsillar abscess, cellulitis, Ludwig’s angina, and cervical lymphadenitis.
- Septicemia and pyemia can cause meningitis, endocarditis, and abscesses in internal organs.
2. Non-Suppurative Complications:
- Acute rheumatic fever:
- S. pyogenes lead to acute rheumatic fever involving both the heart and joints.
- It occurs in a small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross-reaction between group A streptococci and myocardium, so antibodies produced against Streptococcus, cross-react, with the heart leading to damage.
- Acute glomerulonephritis:
- It occurs as a result of cross-reaction between Group A streptococci and antigen of glomerular basement membrane or deposition of antigen-antibody complexes and complement activation.
- It follows infection with nephritogenic strains of streptococci.
Viridans Streptococci
- Morphology: They are commensals of the mouth and upper respiratory tract. This group contains many species, for example, S. salivarius, S. mutans,
S. sanguis, and S. milleri. They are ordinarily non-pathogenic but on occasion cause disease. - Culture Characteristics: This group of streptococci produces alpha hemolysis on blood agar. They are known as viridans streptococci due to greenish discoloration on blood agar.
- Pathogenesis: Viridians streptococci are associated with dental caries and subacute bacterial endocarditis.
- Dental caries is caused by S. mutans. It breaks down dietary sucrose, producing acid and a tough adhesive dextran.
- The acid damages dentine while the dextran binds together food debris, mucus, epithelial cells, and bacteria to form dental plaques. These plaques lead to dental caries.
- About 40% of subacute bacterial endocarditis is caused by viridans group of streptococci.
- S. mitis is the predominant agent followed by S. mutans and S. milleri.
- They cause endocarditis in persons with predisposing factors such as valvular disease of the heart, congenital heart disease, and cardiac surgery.
- Following some dental procedures such as tooth extraction, they may cause transient bacteremia and get implanted on damaged or prosthetic valves or in a congenitally diseased heart, and grow to form vegetation.
Question 16. Name three diseases caused by S. pyogenes.
Answer:
Three diseases caused by S. pyogenes are:
- Respiratory tract infection
- Skin and soft tissue infections
- Acute rheumatic fever.
Respiratory Tract Infection
- Sore throat is the most common disease.
- It can also lead to pharyngitis and tonsillitis.
- Streptococcal pneumonia occurs secondary to viral infection
of lung. - Scarlet fever is the combination of sore throat and generalized erythematous rash with punctuate spots.
Skin and Soft Tissue Infections
- S. pyogenes causes suppurative infections of the skin with a predilection to produce lymphangitis and cellulitis.
- Infection of minor abrasions may sometimes lead to fatal septicemia.
- The two typical streptococcal skin infections are erysipelas and impetigo.
- Erysipelas: In this disease-causing spreading sharply demarcated erythematous lesions are seen in adults.
- Impetigo: Skin infection in young children which is characterized by a superficial skin lesion as a discrete spot of 2 to 5 cm and healed without producing a scar.
- A streptococcal pyoderma is a severe form of ulcerative skin lesion.
- Necrotizing fasciitis is caused by aerobes and anaerobes as a mixed infection or streptococci alone. Clinically there is extensive necrosis of subcutaneous tissue, muscle, and fascia along with TSS-like systemic involvement in the form of disseminated.
- Intravascular coagulation and multiple system failure – streptococcal toxic shock syndrome.
Acute Rheumatic Fever
- S. pyogenes lead to acute rheumatic fever involving both the heart and joints.
- It occurs in a small number of cases after 2 to 3 weeks of pharyngeal infection.
- Antigen cross-reaction between group A streptococci and myocardium, so antibodies produced against Group A
- Streptococcus cross-react with the heart leading to damage.
Leave a Reply